Background
Observation of the arachnid Demodex folliculorum has been reported since 1840. This hair follicle mite is the only metazoan organism commonly found in the pilosebaceous components of the eyelid of humans. Coston "opened the eyes" of ophthalmologists when he described 22 patients with demodectic eyelid signs and symptoms. [1, 2]
Pathophysiology
D folliculorum (all stages) is found in small hair follicles and eyelash hair follicles. In all forms, immature and adult, it consumes epithelial cells, produces follicular distention and hyperplasia, and increases keratinization leading (in eyelashes) to cuffing, which consists of keratin and lipid moieties. Demodex brevis (all stages) is present in the eyelash sebaceous glands, small hair sebaceous glands, and lobules of the meibomian glands. Adults and immature forms consume the gland cells in all of these loci and, when infestations are heavy, can affect the formation of the superficial lipid layer of the tear film coacervate. Demodectic mites produce histologically observable tissue and inflammatory changes, epithelial hyperplasia, and follicular plugging.
Infestation of the eyelash hair follicle results in easier epilation and more brittle cilia. These mites also serve as vectors of infective elements and interrupt tissue integrity. They have been implicated in meibomian granulomas and are associated with specific dermatologic changes. All reported histologic sections of lid follicles infested with D folliculorum show distention and thickening. Coston claims that less than one-half of the specimens he observed showed perifollicular lymphocytic infiltration. [2]
Follicular inflammation produces edema and results in easier epilation of the eyelashes. It also affects cilia construction, and lashes are more brittle in the presence of demodicosis. Madarosis (loss of lashes) is associated with abundant mites, the loss of eyelashes due to intercellular edema in the hair shaft, and loss of hair resiliency. Although epithelial hyperplasia associated with follicular plugging often is encountered, dermal changes seldom extend beyond the perifollicular epidermal area. Once believed to be mite excreta, this plugging now is known to be epithelial hyperplasia with interspersed lipid layers. The formation of a collar of tissue around the base of the lashes is observed clinically. This occurs significantly more often in follicles infected with D folliculorum. The epithelial hyperplasia is hypothesized to be most likely a product of the abrasive action of the mite's claws.
Accumulation of waste material of the follicle mite may occur in affected follicles or sebaceous glands. Electron micrographs of the mite surface and feces show bacterial, viral, and rickettsial elements. Specific reports have revealed that both species pierce epithelial cells and consume cytoplasm. Only D brevis has been observed with channels burrowed to the germinal epithelium in the sebaceous glands.
Demodex species-induced pathologic changes have been implicated in dry eye conditions. When follicular plugging involves the meibomian gland (D brevis) or the gland of Zeis (D folliculorum or D brevis), reduction of the superficial lipid layer of the tear film occurs. The effect of D brevis on the meibomian structure has been implicated in chalazion formation. Chalazia are granulomatous inflammation of the meibomian glands, made of an organized core of epithelioid cells and histocytes surrounded by fibroblasts, lymphocytes, and plasma cells. These defense cells encircle particles too large for normal macrophages to engulf. D brevis has been observed in the center of these meibomian granulomas. Lid infestation by the Demodex species may or may not accompany dermatologic changes of the nose, the cheek, or the forehead.
D folliculorum has been suggested as a factor in pityriasis folliculorum. This dermal inflammation manifests as diffuse erythema of the affected areas; scaly, dry skin; and, in some instances, rosacea-like lesions. The dry skin cycle described by Ayres is initiated when the demodectic mite plugs the follicle and reduces the sebaceous outflow, leading to scaling and rough and dry skin texture. [3] Sebaceous outflow is further reduced when patients inadvertently decide to apply facial cream. The mite flourishes in this environment of oily additives, leading to an increase in the population of the mites and a continuation of the dry skin cycle.
Epidemiology
Frequency
International
Several individuals have attempted to estimate the prevalence of D folliculorum in the eyelash follicles. The initial report in 1961 suggested a prevalence of 95%. [4]
Mortality/Morbidity
Madarosis (loss of lashes) may result from untreated demodicosis.
Race
No racial predilection has been observed.
Sex
Infestation by these parasites is equal in males and females. Infestation is correlated to the number of sebaceous glands but not to the density of the hair follicles.
Age
Post reported that D folliculorum was observed in 84% of the sample population with a mean age of 61 years and 100% of those older than 70. [5] Liang L et al [6] reported in 2010 that ocular demodicosis should be considered as a potential cause of pediatric (2.5-11 years) refractory blepharoconjunctivitis.
Prognosis
The prognosis of symptomatic relief from D folliculorum is excellent.
Previous clinical experience shows that total eradication is unlikely, but the mite population can be brought down to an acceptable level with little effort and easily maintained with proper hygiene.
There are promising reports of total eradication with the use of tea tree oil, terpinon-4-ol, and ivermectin 1% cream.
Recurrence of the symptoms is possible if proper hygienic measures are not used.
Patient Education
The suggested home treatment, including the eyelash scrub technique, should be demonstrated to the patient as follows:
-
Soak the washcloth in warm water, and wring it.
-
Apply enough baby shampoo to form a lather on the washcloth.
-
With the eye closed, massage the lashes on the lid margin, moving from left to right 15 times. (Do not touch the eye itself.) Repeat on the other eye.
-
Rewet the cloth, and rinse off the shampoo.
-
Squeeze 1 inch of the ointment onto the index finger and gently rub into the lashes with the eye closed. Repeat on the other eye.
To the eye care professional, the presence of Demodex species, together with signs or symptoms of lid inflammation, is of a more significant concern than the prevalence of Demodex species in a general population.
Tea tree oil and tea tree oil shampoo may be purchased from specialty shops locally and online.
-
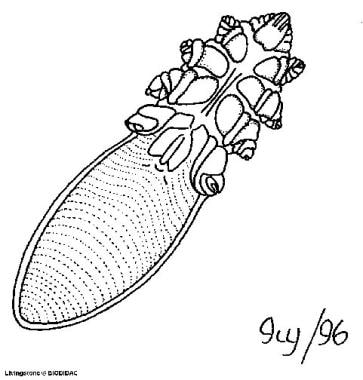
Illustration of Demodex folliculorum. Reprinted with permission from Antoine Morin, BIODIDAC, University of Ottawa.
-
Eyelid section shows Demodex folliculorum (M) in the hair follicle. Note mite mouthparts (arrow) embedded in epithelium and straplike layers of keratin (hematoxylin and eosin, X400). Reprinted with permission from Elsevier Science.
-
Section of sebaceous gland of an eyelash shows Demodex brevis (M). Note gland cell (C) destruction (McManus, X375). Reprinted with permission from Elsevier Science.
-
Cross-section through small hair follicle of the eyelid. Note distension, hyperplasia, and moderate epithelial keratinization caused by the activities of Demodex folliculorum (arrow) (hematoxylin and eosin, X375). Reprinted with permission from Elsevier Science.
-
Section of eyelid shows eyelash (L), cuffing (C), and small segment of Demodex folliculorum (M). Note layering of cuff (Masson, X275). Reprinted with permission from Elsevier Science.
-
Demodex folliculorum.
-
Demodex along the shaft of the cilia.
-
Demodex along the shaft of the cilia (higher magnification).
-
Backsides of numerous pubic crabs with infestation of the lashes and secondary blepharitis. Reprinted with permission from HD Riley, OD, Indiana University School of Optometry.
-
Phthiriasis (Phthirus pubis) pubic crab lash infestation and secondary blepharitis. Reprinted with permission from HD Riley, OD, Indiana University School of Optometry.
-
Phthiriasis (pubic lice). Reprinted with permission from HD Riley, OD, Indiana University School of Optometry.
-
Demodex infestation is an under diagnosed cause of chronic blepharitis. Image courtesy of Rendia, Inc. Copyright 2017 Rendia, Inc.
-
Blepharitis secondary to Demodex infestation. Image courtesy of Rendia, Inc. Copyright 2017 Rendia, Inc.
-
A novel in-office treatment using a mechanical rotating handpiece with a microsponge tip combined with PolyaminopropylBiguanide foam solution removes oil, scurf, and debris; exfoliates the eyelids, and claims to decrease Demodex infestation. Image courtesy of Rendia, Inc. Copyright 2017 Rendia, Inc.
-
Intense pulsed light. Courtesy of OPTIMED (https://www.optimed.co.uk/), E-referral and patient engagement platform.