Background
Leukemias are a group of heterogeneous neoplastic disorders of white blood cells. Based on their origin, myeloid or lymphoid, they can be divided into 2 types. Leukemias traditionally have been designated as acute or chronic, based on their untreated course. Acute leukemias usually present as hemorrhage, anemia, infection, or infiltration of organs.
Many patients with chronic leukemias are asymptomatic. Other patients present with splenomegaly, fever, weight loss, malaise, frequent infections, bleeding, thrombosis, or lymphadenopathy. The image below depicts an impending retinal vein obstruction and intraretinal hemorrhage in a patient with chronic myelogenous leukemia. Some chronic leukemias enter a blast phase where the clinical manifestations are similar to the acute leukemias.
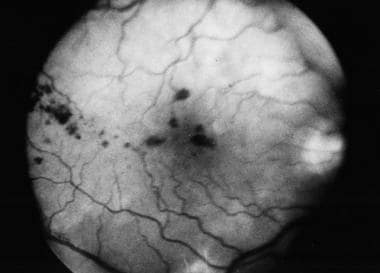 An impending bilateral central retinal vein obstruction was discovered during a routine examination of a 76-year-old man. Further workup revealed a WBC count of 709,000, a hemoglobin count of 12 mg/dL, and a platelet count of 104,000. The man was eventually diagnosed with CML. This image is a red-free photograph of the right fundus. Notice the intraretinal hemorrhages.
An impending bilateral central retinal vein obstruction was discovered during a routine examination of a 76-year-old man. Further workup revealed a WBC count of 709,000, a hemoglobin count of 12 mg/dL, and a platelet count of 104,000. The man was eventually diagnosed with CML. This image is a red-free photograph of the right fundus. Notice the intraretinal hemorrhages.
See Chronic Leukemias: 4 Cancers to Differentiate, a Critical Images slideshow, to help detect chronic leukemias and determine the specific type present.
Chronic myelogenous leukemia (CML) is characterized by an uncontrolled proliferation of granulocytes. An accompanying proliferation of erythroid cells and megakaryocytes usually is present. Many patients are asymptomatic but may present with splenomegaly, weight loss, malaise, bleeding, or thrombosis.
Chronic lymphocytic leukemia (CLL) represents a monoclonal expansion of lymphocytes. In 95% of cases, CLL is a predominantly malignant clonal disorder of B lymphocytes. The remainder is secondary to a T-cell clone. The neoplastic cell is a hypoproliferative, immunologically incompetent small lymphocyte. There is primary involvement of the bone marrow and secondary release into the peripheral blood. The recirculating lymphocytes selectively infiltrate the lymph nodes, the spleen, and the liver. Most patients are asymptomatic at diagnosis. As the disease progresses, lymphadenopathy, splenomegaly, and hepatomegaly develop. A secondary immune deficiency with hypogammaglobulinemia exists. A study by Wang et al found that when they studied the landscape of somatic mutations in chronic lymphocytic leukemia, pre-mRNA splicing was an important cellular process. [1]
Acute lymphocytic leukemia (ALL) is a malignant clonal disorder of the bone marrow lymphopoietic precursor cells. In ALL, progressive medullary and extramedullary accumulations of lymphoblasts are present that lack the potential for differentiation and maturation. An inhibition of the normal development of hematopoietic cell elements occurs. The clinical presentation is dominated by progressive weakness and fatigue secondary to anemia, infection secondary to leukopenia, and bleeding secondary to thrombocytopenia. When 50% of the bone marrow is replaced, then peripheral blood cytopenias are observed.
Acute myelogenous leukemia (AML) is a group of neoplastic disorders of the hematopoietic precursor cells of the bone marrow. AML is subdivided by the French-American-British system into 6 categories depending on the morphology. AML is not a disorder of rapidly proliferating neoplastic cells. The time for 1 cell division is prolonged with respect to that of normal bone marrow blast cells. A failure of maturation of the neoplastic cell clone exists. The bone marrow is gradually replaced by blast cells. Therefore, the most important complications are progressive anemia, leukopenia, and thrombocytopenia.
Pathophysiology
In leukemias, a clone of malignant cells may arise at any stage of maturation, that is, in the lymphoid, myeloid, or pluripotential stage. The cause for this clonal expansion is poorly understood in most cases, but it appears to involve some rearrangement of the DNA. External factors, such as alkylating drugs, ionizing radiation, and chemicals, and internal factors, such as chromosomal abnormalities, lead to DNA changes.
Chromosomal rearrangements may alter the structure or regulation of cellular oncogenes. For instance, in the B-cell lymphocytic leukemias, chromosomal translocations may put the genes that normally regulate heavy and light chain immunoglobulin synthesis next to the genes that regulate normal cellular activation and proliferation. This results in proliferation of lymphoblasts. As the population of cells expands, the bone marrow starts to fail. Pancytopenia is typical and results in part from the physical replacement of normal marrow elements by the immature cells. In addition, the abnormal cells may secrete factors that inhibit normal hematopoiesis.
As the bone marrow becomes replaced, the abnormal cells spill into the circulation and infiltrate other organs, such as the liver, the spleen, and the eye. Any of the ocular structures may be affected. Ocular involvement may occur prior to the diagnosis of leukemia, during the disease course, or as a sign of relapse. The ocular manifestations may be secondary to direct infiltration of the leukemic cells, as a result of abnormal systemic hematological parameters, opportunistic infections, or iatrogenic complications arising from chemotherapy.
Epidemiology
Frequency
United States
The American Cancer Society estimates that 60,650 [2] new cases of leukemia will be diagnosed in the United States in 2022. Of the leukemias, 20,160 [3] will be CLL; 20,050 [2] will be AML; 6660 [4] will be ALL; and 8860 [5] will be CML.
Clinical series show variable data regarding prevalence and incidence of ocular involvement in patients with leukemia. These differences arise from the differences in study design. In some studies, patients were examined at different stages of the disease. In others, ophthalmologists examined only symptomatic patients. In most studies, no distinction is made between the different leukemias.
Three prospective studies reveal that 14-53% of patients had ocular manifestations of the disease prior to the start of chemotherapy. Leukemia is responsible for 2-6% of orbital tumors in children. Furthermore, up to 11% of children with proptosis will have some form of acute leukemia. [6, 7]
Autopsy series show the highest frequency of ocular involvement. It is presumed that dying patients have a higher disease burden. In addition, histopathological methods allow detection of lesions that are not clinically detectable. About 28-80% of cases have intraocular manifestations. An autopsy study reports 8-12% have orbital involvement. [8]
Despite changes in treatment and survival over the past decades, ocular involvement, as examined by histopathological methods, has remained fairly constant in the past 70 years.
International
According to GLOBOCAN, 474,519 new cases of leukemia were diagnosed worldwide in 2020, representing 2.5% of all cancer sites/types reported. [9]
Mortality/Morbidity
When all leukemias are lumped together, the global 5-year survival is 20%. In developed countries, 31% survive for 5 or more years, compared with 15% in developing countries. This underscores the lack of access to high-tech treatment in the developing world. In 2002, 222,506 deaths were reported globally, secondary to all leukemias. It was estimated that, in the United States during 2009, there would be a total of 21,870 deaths secondary to all leukemias.
The breakdown of deaths according to the different subtypes is as follows [10, 11, 8, 12] :
-
Deaths secondary to ALL and AML have been reported at 1400 and 6900, respectively.
-
In children with ALL, 90% of patients achieve a complete remission, and up to 80% can remain disease free at 5 years following treatment. In adults with ALL, remissions occur in 60-80%, while 20-35% will maintain a leukemia-free survival.
-
Currently, 65-70% of patients with AML attain remission. The 5-year survival rate during the period 1989-1994 was 43%.
-
In a study from Italy, the presence of specific orbital or ocular lesions in ALL and AML was associated with a higher frequency of bone marrow relapses and CNS involvement, which led to a lower survival rate. [13]
-
Secondary to CLL, 5100 deaths have occurred; secondary to CML, 2300 deaths have occurred; and secondary to other leukemias, 6400 deaths have occurred.
-
In CLL, the natural history is highly variable. The median survival is 6 years, and the natural history is not altered by therapy. Infection is the leading cause of death. The median survival of CML with treatment is 5 years. Granulocytic sarcoma of the orbit, also known as chloroma, represents an extramedullary site of AML or CML. Survival has been reported to range from 1 month to 30 months after the onset of ocular signs and symptoms. Some studies suggest that the presence of intraocular leukemic infiltrates correlates with CNS involvement and with decreased survival.
Race
In the United States, ALL and CLL are more common in Whites than in Blacks.
Sex
Of the estimated 44,790 new cases of leukemia to be diagnosed in the United States during 2009, 25,630 cases will be in males and 19,160 cases in females. [14]
The breakdown of new cases of leukemia by gender and category is as follows:
-
CLL: 9200 cases in males and 6290 cases in females
-
CML: 5,120 in men and 3,740 in women [5]
-
ALL: 3,740 in males and 2,920 in females; childhood ALL demonstrates a notable male predominance. [4]
-
AML: 6290 cases in males and 5890 cases in females
-
In other leukemias, 3230 cases in males and 2450 cases in females 5680 total cases
Age
Most childhood leukemias are acute.
ALL is the most common malignancy in children, especially affecting those aged 2 years to 10 years. ALL is seen in only 20% of adult acute leukemias and behaves more aggressively than the childhood type.
AML constitutes 15-20% of acute leukemias in children. Incidence of AML increases with age; in persons younger than 65 years, the incidence is 1.3, and in persons older than 65 years, the incidence is 12.2.
CML constitutes less than 5% of childhood leukemias. The incidence of CML increases slowly with age until the middle 40s, when the incidence starts to rise rapidly.
Incidence of CLL is over 10 per 100,000 for persons older than 70 years but is less than 1 per 100,000 for those younger than 50 years. Mean age at diagnosis of CLL is 60 years.
Prognosis
Retinal involvement in patients with leukemia appears to have a prognostic value. Those with retinopathy have more aggressive disease and therefore worse outcomes. [15, 16] The presence of cotton wool spots decreases the mean survival significantly. [17] A recent Iranian study from three tertiary centers reported higher mortality rates in patients with ocular involvement. [18]
Patients in remission may rarely present with ophthalmic manifestations that represent a recurrence. A high index of suspicion is required to make the diagnosis to avoid delay in treatment in these potentially blinding conditions. [19]
-
A 4-year-old boy presented with sudden proptosis of his left eye.
-
Same patient as in the image above. A CBC revealed anemia (Hb 8.6 mg/dL), thrombocytopenia (64,000), and leukocytosis (12,900). The peripheral smear revealed the presence of blasts 28%, lymphocytes 44%, segmented 14%, monocytes 6%, bands 2%, metamyelocytes 1%, and myelocytes 1%. The boy was diagnosed with AML type M4-M5 chloroma of the left orbit.
-
CT scan reveals infiltration in the left orbit. Notice that the bone is uninvolved. A lumbar puncture revealed that the cerebral spinal fluid was clean of leukemic cells.
-
Systemic chemotherapy was instituted, and the proptosis resolved. Unfortunately, 4.5 months later, the boy passed away secondary to multiorgan failure.
-
An impending bilateral central retinal vein obstruction was discovered during a routine examination of a 76-year-old man. Further workup revealed a WBC count of 709,000, a hemoglobin count of 12 mg/dL, and a platelet count of 104,000. The man was eventually diagnosed with CML. This image is a red-free photograph of the right fundus. Notice the intraretinal hemorrhages.
-
Same patient as in the image above. This image is a red-free photograph of the left eye showing intraretinal hemorrhages.
-
A 14-year-old boy with a past medical history of ALL complained of a sudden loss of vision OD. Visual acuities were counting fingers OD and 20/20 OS. Notice the macular hemorrhage responsible for the loss of vision. Courtesy of Dr Rafael Jiménez.
-
Same patient as in the previous image. The hematological workup revealed a hemoglobin count of 5.6, a WBC count of 1800, and a platelet count of 3000. Courtesy of Dr Rafael Jiménez.








