Practice Essentials
Retinopathy of prematurity (ROP) is a disease that affects immature vasculature in the eyes of premature babies. [1] It can be mild with no visual defects, or it may become aggressive with new blood vessel formation (neovascularization) and progress to retinal detachment and blindness.
Signs and symptoms
Retinopathy of prematurity (ROP) affects low-birth-weight premature infants and can lead to blindness; the incidence of ROP has increased, as smaller and younger babies are surviving.
Risk factors
-
Birth before 32 weeks' gestation, especially before 30 weeks
-
Birth weight of less than 1500 g, especially less than 1250 g
-
Possible risk factors include supplemental oxygen, hypoxemia, hypercarbia, concurrent illness
See Clinical Presentation for more detail.
Diagnosis
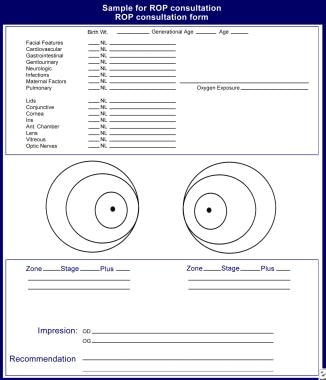
The image below depicts a sample consultation form and fundus drawing used in the evaluation of retinopathy of prematurity.
Diagnosis of ROP requires a dilated fundus examination with scleral depression, using the following instruments:
-
Sauer speculum (to keep the eyes gently open)
-
Flynn scleral depressor (to rotate and depress small eyes)
-
28-diopter lens (for proper identification of zones)
ROP is categorized by the severity of the disease in zones of the retina. It is categorized by the lowest zone and the highest stage observed in each eye.
The classification of acute ROP was developed by the International Classification of Retinopathy of Prematurity (ICROP) group first in 1984, then expanded in 1987. [2] This was based on clinical examination that classified acute ROP into 5 stages, 3 zones, and extent of retinal involvement. An additional feature included the presence of dilated and tortuous posterior pole vessels known as “plus” disease. An entity known as aggressive posterior ROP (APROP) was defined in 2005 to describe a posterior disease with prominent plus and ill-defined retinopathy that may rapidly progress to stage 5 disease. [2] Pre-plus disease was also described to include eyes with vessel tortuosity that did not meet “plus” criteria. Over the years, progress has been made in ophthalmic imaging and treatment options. Increasingly, we are aware of global differences in terms of ROP patterns, as well as subjectivity among ROP experts (see below). This provided the impetus for the ICROP 3rd edition (ICROP3) which provides further guidance and should be read in full text in the reference link by anyone reading this article as it is the current gold standard. [3] Important additions in ICROP3 include refined classification metrics such as “posterior zone II,” a notch, subcategorization of stage 5, recognition of a spectrum of vascular abnormality defining plus disease, the use of the term aggressive ROP (AROP) instead of specifically APROP, and description of regression, reactivation, and long-term sequelae. [4]
Zone 1
-
The center of zone 1 is the optic nerve
-
The zone extends twice the distance from the optic nerve to the macula in a circle
-
Any portion of the optic nerve in the same view as the ridge of ROP is considered zone 1
Zone 2
Zone 2 is a circle surrounding the zone 1 circle, with the nasal ora serrata as its nasal border. Zone 2 disease may progress quickly, but the following warning signs usually predate the threshold by 1-2 weeks:
-
The ridge shows signs of vascular arcading (increased branching); this is usually a sign that the disease is becoming aggressive
-
Increasing vascular dilation and tortuosity is present
-
A "hot dog" on the ridge (ie, a thickened, red, vascular area that may not show the typical fronds of neovascularization); it usually is seen in posterior zone 2 (borders zone 1); it indicates a poor prognosis
-
Threshold disease: 5 contiguous or 8 noncontiguous hours of neovascularization (stage 3) with plus disease in zone 1 or 2
Zone 3
-
Zone 3 is the crescent that the circle of zone 2 did not encompass temporally
-
Aggressive disease rarely is seen in zone 3
-
Slow vascularization is typical, requiring evaluations every few weeks
-
Many infants show inactive disease in zone 3, with a demarcation line and nonvascularized retina; this has been noted in toddlers, can be considered cicatricial peripheral disease, and has no known ill sequelae
Stage 0
-
The mildest form of ROP
-
Immature retinal vasculature
-
No clear demarcation of vascularized and nonvascularized retina is present
-
In zone 1, stage 0 may appear as a vitreous haze, with the optic nerve as the only landmark; weekly examinations should be performed
-
In zone 2, examinations should be performed every 2 weeks
-
In zone 3, an examination every 3-4 weeks should be sufficient
Stage 1
-
A fine, thin demarcation line between the vascular and avascular region is present
-
The demarcation line has no height and no thickness
-
In zone 1, the line should appear flat and thin (usually nasally first), with no elevation from the avascular retina, and retinal vessels should be smooth, thin, and supple
-
In zone 1, weekly examinations should be performed
-
In zone 2, examinations should be performed every 2 weeks
-
In zone 3, an examination every 2-3 weeks should be sufficient
Stage 2
-
A broad, thick ridge clearly separates the vascular from the avascular retina
-
In zone 1, any hint of pink or red in the ridge is an ominous sign
-
If there is any vessel engorgement in zone 1, the disease should be considered threshold and treatment commenced within 72 hours
-
In zone 2, if there are no vascular changes and the ridge has no engorgement, the eye should be examined within 2 weeks
-
In zone 2, prethreshold is defined as stage 2 with plus disease
-
In zone 3, examination every 2-3 weeks should be sufficient, unless there is any vascular tortuosity or straightening of the vascular arcades
Stage 3
Extraretinal fibrovascular proliferation (neovascularization):
-
Sites include the ridge, the posterior surface of the ridge, and anteriorly toward the vitreous cavity
-
The neovascularization gives the ridge a velvety appearance and a ragged border
-
In zone 1, any neovascularization is serious and requires treatment
-
In zone 2, prethreshold is defined as stage 3 without plus disease, or stage 3 with less than 5 contiguous or 8 noncontiguous hours; threshold is stage 3 with at least 5 contiguous or 8 noncontiguous hours and plus disease
-
In zone 3, examination every 2-3 weeks should be sufficient, unless there is any vascular tortuosity or straightening of the vascular arcades
Stage 4
-
Subtotal retinal detachment beginning at the ridge
-
The retina is pulled anteriorly into the vitreous by the fibrovascular ridge
-
Stage 4A does not involve the fovea
-
Stage 4B involves the fovea
Stage 5
This stage is a total retinal detachment in the shape of a funnel:
-
Stage 5A is an open funnel
-
Stage 5B is a closed funnel
Plus disease
-
Part of the subclassification of stages
-
The presence of plus disease is an ominous sign
Features of plus disease:
-
Arteriolar tortuosity and venous engorgement of the posterior pole
-
Iris vascular engorgement
-
Pupillary rigidity
-
Vitreous haze
Pre-plus disease
-
Vascular abnormalities of the posterior pole that are insufficient for the diagnosis of plus disease but that demonstrate more arteriolar tortuosity and more venular dilatation than normal
-
Pre-plus disease early in the course of ROP is strongly associated with development of severe ROP that required laser treatment
See Workup for more detail.
Management
Management of ROP is as follows:
-
Screening at-risk preterm infants at proper times and intervals, as recommended by the American Academy of Pediatrics [5]
-
Although oxygen therapy has been blamed for ROP progression in the past, maximizing the oxygen saturation (to 95%) may induce regression in prethreshold disease
-
Cryotherapy was the original mode of treatment (since the 1970s)
-
Laser surgery (eg, xenon, argon, diode) is as effective as cryotherapy, does not require general anesthesia, and has a lower complication rate
-
Scleral buckling surgery and/or vitrectomy is usually performed for stages 4 and 5
-
Surgery for stage 4A and stage 5 is controversial
See Treatment and Medication for more detail.
Background
Retinopathy of prematurity (ROP) is a disease that affects immature vasculature in the eyes of premature babies. It can be mild with no visual defects, or it may become aggressive with new blood vessel formation (neovascularization) and progress to retinal detachment and blindness. As smaller and younger babies are surviving, the incidence of ROP has increased.
During the 1940s and 1950s, ROP, also known as retrolental fibroplasia, was the leading cause of blindness in children in the United States. In 1942, Terry first reported the disease that was published in a report on the histologic findings of end-stage cicatricial disease. [6] In 1951, Campbell first suggested that ROP was related to the introduction of oxygen therapy into the newborn nursery, and this was confirmed by Patz. [7] Today, after oxygen therapy has been studied and found not to be the single causative agent, the factors that play a role in the pathogenesis of ROP are still unknown.
Pathophysiology
The retinal vasculature begins in the 16th week of gestation. Retinal vessels grow out of the optic disc as a wave of mesenchymal spindle cells. As these mesenchymal spindle cells lead the shunt, endothelial proliferation and capillary formation follow. These new capillaries will form the mature retinal vessels. The choroidal vessels (that are vascularized by the 6th week of gestation) supply the rest of the avascularized retina. The nasal portion of the retina is completely vascularized to the ora serrata by the 32nd week of gestation. The larger temporal area usually is completed at 40-42 weeks (term).
Two theories exist on the pathogenesis of ROP. The mesenchymal spindle cells, exposed to hyperoxic extrauterine conditions, develop gap junctions. These gap junctions interfere with the normal vascular formation, triggering a neovascular response, as reported by Kretzer and Hittner. [8] Ashton theorizes that 2 phases exist. [9] The first phase, a hyperoxic phase, causes retinal vasoconstriction and irreversible capillary endothelial cell destruction. As the area becomes ischemic, angiogenic factors, such as vascular endothelial growth factor (VEGF), is made by the mesenchymal spindle cells and ischemic retina to provide new vascular channels. These new vascular channels are not mature and do not respond to proper regulation.
The most conspicuous question in the pathophysiology of ROP is why it progresses in some premature infants despite rigorous and timely intervention, whereas, in other infants with similar clinical characteristics, it regresses. Csak et al believe that perhaps the genetic differences between infants could be an explanation. [10] Although many causative factors, like low birth weight, low gestational age, and supplemental oxygen therapy, are associated with ROP, several indirect lines of evidence suggest the role of a genetic component in the pathogenesis of ROP. The incidence of ROP is more frequent in white infants than in black infants and in male infants than in female infants. Genetic polymorphism may alter the function of the genes that normally control retinal vascularization, such as VEGF, which may also be involved in the pathogenesis of ROP.
In the future, evaluation of candidate genetic polymorphism influencing the outcome of ROP may provide new information about the pathogenesis of the disease. Screening of genetic polymorphisms may also help to identify and treat those infants who are at high risk in a more timely manner.
A 2023 review of the pathophysiology of ROP was published in Survey of Ophthalmology. [1]
Frequency
United States
The incidence of ROP in premature infants is inversely proportional to their birth weight. Fielder studied infants weighing less than 1700 g and noted development of ROP in 51%. [11]
In general, more than 50% of premature infants weighing less than 1250 g at birth show evidence of ROP, and about 10% of the infants develop stage 3 ROP.
International
In 1995, ROP accounted for 10.6% of cases of blindness in children in schools for the blind in South Africa. [12]
Mortality/Morbidity
On average, 500-700 children become blind because of ROP in the United States each year. In terms of life years of blindness, this translates to 30,000 life years of vision.
Annually, 2100 infants will be affected with cicatricial sequelae, including myopia, strabismus, blindness, and late-onset retinal detachment.
The rule of thumb is that approximately 20% of all premature babies will develop some form of strabismus or refractive error by the time they are age 3 years. This is why babies who are younger than 32 weeks or less than 1500 g receive follow-up care every 6 months, whether or not ROP is present.
Race
Palmer and colleagues showed that African Caribbean infants are less likely to develop ROP than their Caucasian counterparts. [13]
Sex
The incidence is slightly greater in male infants than in female infants.
Age
ROP is a disease of premature infants. All babies less than 1500 g birth weight or younger than 32 weeks' gestational age at birth are at risk of developing ROP.
As younger and smaller infants are surviving, the screening protocols are changing to include earlier gestational age. In any neonatal intensive care unit (NICU), the timing of the first evaluation must be based on the gestational age at birth. (See the Gestational Age from Estimated Date of Delivery calculator.)
-
If the baby is born at 23-24 weeks' gestational age, the first eye examination should be performed at 27-28 weeks gestational age.
-
If the baby is born at or beyond 25-28 weeks' gestational age, the first examination should occur at the fourth to fifth week of life.
-
Beyond 29 weeks, the first eye examination probably should occur before the infant is discharged.
Prognosis
The prognosis is guarded until zone 3 is reached.
Patient Education
Patients should be educated about the following:
-
Awareness of the risk of potential visual loss from amblyopia, strabismus, retinal detachment, or glaucoma
-
Possible need for repeated surgical procedures
-
Possible patching for amblyopia, thick glasses for myopia, or possible strabismus surgery
-
Retinopathy of prematurity consultation form and fundus drawing.