Practice Essentials
Bacterial endophthalmitis (see the image below) is an inflammatory reaction of the intraocular fluids or tissues caused by microbial organisms. Bacteria may gain entry into the eye via corneal or scleral trauma (surgical or accidental) or hematogenously. If not properly treated, bacterial endophthalmitis can result in complete vision loss and persistent ocular pain.
Signs and symptoms
The clinical presentation depends on the route of entry, the infecting organism, and the duration of the disease. In general, patients complain of the following:
-
Decreased vision
-
A red eye
-
Deep ocular pain
Bacterial endophthalmitis is classified on the basis of routes of entry (ie, exogenous or endogenous). [1] Disease from exogenous sources includes the following:
-
Delayed onset or chronic pseudophakic postoperative (>6 wk postoperative) [2]
-
Filtering bleb associated
-
Posttraumatic– History of trauma is present, and infection usually progresses rapidly [4]
On physical examination, general findings in bacteria endophthalmitis are as follows:
-
Visual acuity decreased below the level expected
-
Lid edema
-
Conjunctival hyperemia
-
Corneal edema
-
Anterior chamber cells and flare
-
Keratic precipitates
-
Hypopyon [5]
-
Fibrin membrane formation
-
Vitritis
-
Loss of red reflex
-
Retinal periphlebitis if view of fundus possible [6]
Specific physical examination findings are as follows:
-
Delayed onset or chronic cases– Occasionally, a white plaque within the equator of the remaining lens capsule
-
Filtering bleb associated– A purulent bleb is seen occasionally with areas of necrosis in the sclera from the use of antimetabolites
-
Endogenous– Patients may appear systemically ill
See Clinical Presentation for more detail.
Diagnosis
Perform culture and sensitivity studies on aqueous and vitreous samples to determine the type of organism and antibiotic sensitivity. [9, 10] If endogenous bacterial endophthalmitis is suspected, a systemic workup for the source is required, with cultures of blood, sputum, and urine. [11]
Sampling procedures
-
Anterior chamber tap
-
Vitreous tap
-
Vitreous biopsy: A 23-gauge vitrectomy cutter may be used if available
For anterior chamber taps, a 30-gauge needle on a tuberculin syringe is used to obtain a 0.1-mL sample under topical anesthesia through the limbus. For vitreous taps, a sub-Tenon or retrobulbar block with lidocaine with epinephrine is given, and a 21-gauge needle on a tuberculin syringe is used to obtain an adequate vitreous sample of 0.1-0.2 mL.
B-scan ultrasound
-
Perform B-scan ultrasound of the posterior pole if view of fundus is poor
-
Typically, choroidal thickening and ultrasound echoes in the anterior and posterior vitreous support the diagnosis
-
Occasionally, another source of inflammation other than or in addition to bacteria, such as retained lens material, may be seen
-
The ultrasound also provides a baseline prior to intraocular intervention and allows assessment of the posterior vitreous face and areas of possible traction [12]
-
Rarely, a retinal detachment is seen concurrently with endophthalmitis
Other imaging studies
In traumatic cases, a CT scan may show thickening of the sclera and uveal tissues associated with various degree of increased density in the vitreous and periocular soft tissue structures. For possible endogenous cases, imaging modalities to rule out potential sources of infection include 2-dimensional echocardiography and chest x-ray.
See Workup for more detail.
Management
Bacterial endophthalmitis is an ocular emergency, and urgent treatment is required to reduce the potential of significant visual loss. [13, 14] All patients should have therapy consisting of the following [15, 16, 17, 18] :
-
Intravitreal and topical antibiotics
-
Topical steroids (eg, ophthalmic prednisolone, dexamethasone, triamcinolone)
-
Cycloplegics (eg, atropine ophthalmic)
When the inflammation is severe, systemic and periocular therapy may be used in non–cataract-induced, delayed onset, filtering bleb–associated, and posttraumatic endophthalmitis. In endogenous endophthalmitis, systemic, topical, and possibly periocular therapy is usually required. [8]
Antibiotics
-
Vancomycin - For patients who cannot receive or have failed to respond to penicillins and cephalosporins or have infections with resistant staphylococci; Assaad et al showed that vancomycin was effective against 99.6% of gram-positive bacterial endophthalmitis isolates tested [19] ; Ahmed et reported that intravitreal, rather than intravenous, vancomycin is necessary for the treatment of bacterial endophthalmitis. [20] It is not necessary to monitor vancomycin levels when administered via intravitreal injection.
-
Ceftazidime - First-line choice for intravitreal gram-negative coverage; ceftazidime was effective against 100% of gram-negative bacterial endophthalmitis isolates in a study by Assaad et al [19]
-
Amikacin - Second-line choice for intravitreal injection for gram-negative coverage
-
Ciprofloxacin/ofloxacin/levofloxacin/moxifloxacin/gatifloxacin ophthalmic - Fluoroquinolones with activity against Pseudomonas, streptococci, MRSA, S epidermidis, and most gram-negative organisms; may have limited activity against anaerobes
Surgical care
Surgical intervention is usually performed urgently; however, elective surgery may suffice in delayed-onset cases. Indications for surgical therapy include the following:
-
Acute pseudophakic postoperative– When the presenting vision is light perception or worse [21]
-
Delayed onset or chronic postoperative– If marked inflammation or a subcapsular plaque is identified, surgical removal is required
-
Filtering bleb–associated– If marked inflammation is present
-
Posttraumatic– If marked inflammation or rapid onset occurs
See Treatment and Medication for more detail.
Background
Bacterial endophthalmitis is an inflammatory reaction of the intraocular fluids or tissues caused by microbial organisms.
Pathophysiology
The entry of bacteria into the eye occurs from a breakdown of the ocular barriers. Penetration through the cornea or sclera results in an exogenous insult to the eye. If the entry is through the vascular system, then an endogenous route occurs. After the bacteria gain entry into the eye, rapid proliferation occurs.
The vitreous acts as a superb medium for bacteria growth, and, in the past, animal vitreous was used as a culture medium. Bacteria, as foreign objects, incite an inflammatory response. The cascade of inflammatory products occurs resulting in an increase in the blood-ocular barrier breakdown and an increase in inflammatory cell recruitment. The damage to the eye occurs from the breakdown of the inflammatory cells releasing the digestive enzymes as well as the possible toxins produced by the bacteria. Destruction occurs at all tissue levels that are in contact with the inflammatory cells and toxins.
Frequency
United States
Incidence after intraocular surgery is less than 0.1%. Incidence of culture-proven endophthalmitis is similar to that of extracapsular cataract extraction and phacoemulsification.
Europe
Creuzot-Garcher et al report an incidence of postoperative endophthalmitis after stand-alone cataract surgery in France of 0.102%, increasing to 0.149% when cataract surgery was combined with corneal, glaucoma, or vitreoretinal procedures. [22]
Mortality/Morbidity
If not properly treated, a risk of complete vision loss and the possibility of persistent ocular pain exist. Infection very rarely spreads beyond the confines of the sclera and tracks into surrounding tissue structures.
Prognosis
The prognosis depends on the following:
-
Duration of endophthalmitis
-
Time to treatment
-
Virulence of bacteria
-
Etiology of entry
-
Existing ocular diseases
From the EVS, the percentage of patients achieving a final visual acuity of 20/100 or better were as follows:
-
Gram-positive, coagulase-negative micrococci - 84%
-
S aureus - 50% [23]
-
Streptococci - 30%
-
Enterococci - 14%
-
Gram-negative organisms - 56%
A statistically significant number (P < 0.001) of poorer visual outcomes occurred with a positive Gram stain or when bacteria other than gram-positive, coagulase-negative cocci were found. [13]
Patient Education
Direct patients to maintain hygienic practice after surgery.
-
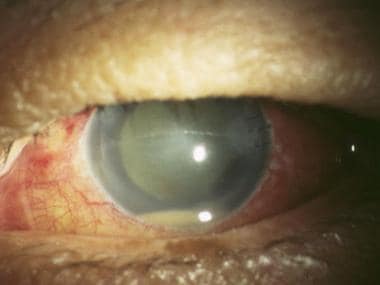
Bacterial endophthalmitis. Hypopyon, 3 days after phacoemulsification.
-
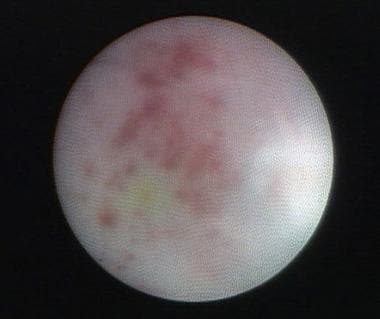
Bacterial endophthalmitis. Retinopathy induced by Enterococcus faecalis endotoxin.