Background
The central retinal artery, a branch of the ophthalmic artery, enters the eye through the optic disc and divides into multiple branches to perfuse the inner layers of the retina. A branch retinal artery occlusion (BRAO) occurs when one of these branches of the arterial supply to the retina becomes occluded. Examples are shown in the images below.
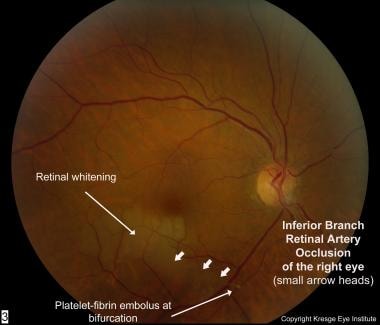 Color fundus photo of right eye with inferior branch retinal artery occlusion from a platelet-fibrin embolus. Retinal whitening surrounding the occluded artery is noted.
Color fundus photo of right eye with inferior branch retinal artery occlusion from a platelet-fibrin embolus. Retinal whitening surrounding the occluded artery is noted.
 Color fundus photo of right eye with inferior branch retinal artery occlusion. Courtesy of Vanderbilt Eye Institute.
Color fundus photo of right eye with inferior branch retinal artery occlusion. Courtesy of Vanderbilt Eye Institute.
 Color fundus photo of right eye with superior branch retinal artery occlusion. Courtesy of Vanderbilt Eye Institute.
Color fundus photo of right eye with superior branch retinal artery occlusion. Courtesy of Vanderbilt Eye Institute.
Pathophysiology
Most commonly, BRAO results from an embolus. Emboli typically originate within vessels upstream where they dislodge and travel within the circulatory system to ultimately become lodged downstream in a vessel with a smaller lumen. The most common include cholesterol emboli from aorto-carotid atheromatous plaques, platelet-fibrin emboli from thrombotic disease, and calcific emboli from cardiac valvular disease. Various other endogenous emboli as well as exogenous emboli and nonembolic causes have been reported. [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14]
Ischemia of the inner layers of the retina leads to intracellular edema as a result of cellular injury and necrosis. This intracellular edema has the ophthalmoscopic appearance of grayish whitening of the superficial retina. Primate studies have shown that complete occlusion of arterial supply to the retina results in reversible ischemic injury in up to 97 minutes. This may help explain why patients may give a history of transient loss of vision prior to an episode of BRAO. Possibly, these episodes are secondary to emboli transiently becoming lodged, causing temporary occlusions and then reperfusing the retina as the emboli are released.
BRAO is most likely to occur at the bifurcation of an artery because bifurcation sites are associated with a narrowed lumen. In 90% of cases, BRAOs involve the temporal retinal vessels. Whether the temporal retinal vessels are affected more often or whether the nasal retinal vessel occlusions are more often undetected is unclear.
Patients with BRAO have a higher risk for morbidity and mortality secondary to cardiovascular and cerebrovascular disease. A thorough medical workup is indicated for all patients with BRAO, and an etiology can be identified in as many as 90% of patients.
Epidemiology
Frequency
United States
Central retinal artery occlusions (CRAOs) account for 58% of acute retinal artery obstructions, BRAOs account for 38%, and cilioretinal artery occlusions account for 5%.
Mortality/Morbidity
Multiple studies have shown increased mortality in patients with retinal arterial emboli. Increased mortality secondary to fatal stroke has been shown in studies, but the most common cause of death in this population is cardiovascular disease. One study found that acute coronary syndrome occurred 1.72 times more often in patients with retinal artery occlusion than in controls. [15] A10-fold increase in the annual rate of stroke in patients with retinal emboli compared with controls after a follow-up period of 3.4 years was demonstrated in another study. [16] Over a similar period, another study showed a 20% incidence of stroke in patients with retinal artery occlusion. [17]
Regarding mortality, 1 study found a 3-fold higher risk for 8-year mortality from stroke in patients with documented retinal emboli at baseline compared with patients without emboli. A case series reported that 15% of patients with retinal emboli died within 1 year, and a mortality rate of 54% was shown within 7 years. Given the higher incidence of cardiovascular and cerebrovascular complications in these patients, appropriate subspecialist referrals should be made at the time of diagnosis.
From an ocular standpoint, and in the absence of subsequent retinal artery occlusions, vision usually stabilizes soon after the ischemic event. A rare, long-term ophthalmic complication is neovascularization. The incidence of neovascularization in all retinal artery obstructions is less than 5%. In BRAO, the incidence is even less common. One large study demonstrated a < 1.0% incidence of neovascularization after BRAO. [18] Neovascularization, when it does occur, is more likely in patients with diabetes. Clinical cases have been reported in which neovascular glaucoma developed after BRAO. [19]
Race
One study compared retinal artery occlusions in Black and White patients and found that both groups have the same risk factors for retinal arterial occlusive disease. [20] This study also suggested that Whites were more likely to have identifiable carotid disease than Blacks.
Sex
Among elderly patients, men are 2.5 times more likely than women to have retinal emboli. This correlates with the higher rate of stroke found in men.
Age
Typically, BRAO presents in the seventh decade of life. BRAO due to embolic causes is rare in patients younger than 30 years. Less than 1 per 50,000 outpatient visits to the ophthalmologist are estimated to involve a person younger than 30 years with retinal arterial obstruction. These cases are more likely to be nonembolic causes of retinal arterial occlusions.
Prognosis
Recovery from BRAO usually is very good without treatment; 80-90% of patients improve to a visual acuity of 20/40 or better. However, some degree of visual field deficit usually persists.
Patient Education
Patients should know that this disorder may serve as a warning of more serious systemic diseases, such as cardiovascular disease or stroke.
For excellent patient education resources, visit eMedicineHealth's Eye and Vision Center and Cholesterol Center. Also, see eMedicineHealth's patient education articles Anatomy of the Eye, High Cholesterol, and Cholesterol FAQs.
-
Fluorescein angiogram of right eye with inferior branch retinal artery occlusion. Delayed filling of the artery (arrow heads) by the fluorescein is noted.
-
Red-free photograph (before injection of fluorescein) of right eye with inferior branch retinal artery occlusion. The red-free photograph greatly accentuates the retinal whitening surrounding the occluded artery.
-
Color fundus photo of right eye with inferior branch retinal artery occlusion from a platelet-fibrin embolus. Retinal whitening surrounding the occluded artery is noted.
-
Optical coherence tomography (OCT) of right eye with inferior branch retinal artery occlusion. Cross-section goes through inferior retina to superior retina, capturing the abnormally thickened retina associated with intracellular edema.
-
Optical coherence tomography (OCT) over time of a branch retinal artery occlusion. Taken 24 hours after symptom onset, A shows an unaffected portion of the macula, while B shows swelling of the inner retina in the area affected by the branch retinal artery occlusion (BRAO). Two weeks later, this swelling/increased thickness is beginning to resolve (C). Two months later, the inner retina has thinned notably, and the inner plexiform layer, inner nuclear layer, and outer plexiform layer are difficult to distinguish from one another. Courtesy of British Journal of Ophthalmology.
-
Color fundus photo of left eye with branch retinal artery occlusion caused by embolization of ethylene vinyl alcohol copolymer (Onyx), a liquid embolic agent used in the treatment of saccular aneurysms, into the retinal circulation. Courtesy of Vanderbilt Eye Institute.
-
Color fundus photo of right eye with inferior branch retinal artery occlusion. Courtesy of Vanderbilt Eye Institute.
-
Color fundus photo of right eye with superior branch retinal artery occlusion. Courtesy of Vanderbilt Eye Institute.






