Practice Essentials
Optic neuritis (ON) is an inflammatory process involving the optic nerve. Optic neuritis may be associated with other neuro-inflammatory syndromes that cause systemic effects.
Pediatric optic neuritis is a rare childhood presentation but can account for 25% of pediatric acute demyelinating syndromes.
Background
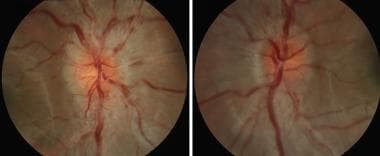
In children, most cases of optic neuritis are due to an immune-mediated process. Pediatric optic neuritis can account for 25% of pediatric acute demyelinating syndromes. [3] Children younger than 10 years usually present with bilateral optic neuritis, whereasile older children usually present with unilateral optic neuritis. [1] These cases of optic neuritis may be associated with a viral or other infection or with immunization. Less commonly, pediatric optic neuritis may be the first manifestation of multiple sclerosis (MS) or part of a more diffuse demyelinating disorder, including acute disseminated encephalomyelitis, neuromyelitis optica (Devic disease), or optic neuritis related to myelin oligodendrocyte glycoprotein (MOG) IgG antibody. [2, 36] Optic neuritis may be related to specific infections, diseases of the adjacent sinuses or orbital structures, and infectious and infiltrative diseases of the brain or meninges that involve the optic nerves. The image below depicts optic disc swelling in a child with bilateral optic neuritis.
The following definitions aid in further understanding optic neuritis:
-
Papillitis - Optic neuritis involving the optic disc with disc edema
-
Retrobulbar optic neuritis - Optic neuritis involving the optic nerve behind the globe. The optic disc appearance should be normal in first-time episodes of retrobulbar optic neuritis.
-
Bilateral simultaneous optic neuritis - Optic neuritis in both eyes occurring within 3 weeks of each other
-
Bilateral sequential optic neuritis - Optic neuritis occurring in both optic nerves but separated by a period of more than 3 weeks
-
Neuroretinitis - Inflammatory process involving the optic discs with exudative changes in the nerve fiber layer of the retina producing a partial or complete macular star. In the past, this condition was called Leber idiopathic stellate neuroretinitis, but now a number of underlying causes for this condition are known. Because this condition is not associated with demyelinating disease and does not imply a future risk of MS, the distinction is important.
Pathophysiology
Possible mechanisms of inflammation in immune-mediated optic neuritis are the cross-reaction of viral epitopes and host epitopes and the persistence of a virus in central nervous system (CNS) glial cells. Patients with optic neuritis due to neuromyelitis optica spectrum disorder lack the aquaporin-4 antibody. [1]
Epidemiology
Incidence
The incidence of pediatric optic neuritis in Canadian children is estimated to be 0.2 per 100,000
Mortality/Morbidity
Patients with optic neuritis have a good prognosis, but a minority of patients experience persistent visual loss. Patients with neuromyelitis optica generally have a poorer recovery. When optic neuritis is associated with other CNS diseases, the morbidity and mortality of those disorders contribute substantially to the final outcome.
Race
Optic neuritis is more common in whites than in other races. [5]
Sex
In both children and adults, a female predominance exists. Females comprise 60-75% of patients.
Age
Optic neuritis may occur at any age, including in infants younger than 1 year. The mean age of presentation for pediatric optic neuritis can range from 9-11 years of age. [4]
A comparison of adult optic neuritis and childhood optic neuritis is presented in Table 1. These features are generally true but are not absolute, and they do overlap.
Table 1. Comparison of Features of Optic Neuritis in Adults and Children (Open Table in a new window)
Adult Optic Neuritis |
Pediatric Optic Neuritis |
Unilateral |
Often bilateral in children < 10 years [6] |
Retrobulbar optic neuritis |
Papillitis |
Commonly associated with pain on eye movements |
Commonly associated with headache |
Most often idiopathic |
Most often postinfectious or postimmunization |
High probability of recurrent inflammatory demyelinating events in the CNS and a diagnosis of MS |
Low probability of recurrent demyelinating events and a diagnosis of MS, with the exception of NMO |
Prognosis
The prognosis for visual recovery generally is considered good to excellent, regardless of medical treatment, except in cases of neuromyelitis optica (see Medical Care). [4, 7]
Approximately one third of children with optic neuritis present with recurrent symptoms. [1]
Multiple sclerosis
Older children and those with brain MRI abnormalities outside the visual system (viewed using T2-weighted and FLAIR sequences) at presentation are at greater risk for MS. [6] The increased risk for MS in older children may result from a difference in their immune system, hormonal change, or puberty; further research is required. In addition, the risk of evolving multiple sclerosis is probably less in children than in adults, but pediatric optic neuritis is more likely to be an initial manifestation of acute disseminated encephalomyelitis. [7]
Adults with isolated optic neuritis have a substantial risk of developing MS. Approximately 15% of patients with normal MRIs at the time of their optic neuritis develop MS in the next 4 years. However, MRI findings are strongly correlated with risk of recurrence of demyelinating events. [6] Fifty percent of patients whose MRIs demonstrate white matter lesions characteristic of MS at the time of their optic neuritis develop clinically definite MS in the next 4 years.
A large study from the Mayo Clinic with a mean follow-up of 20 years produced a life-table analysis showing 13% of children with optic neuritis had progressed to clinically or laboratory-supported definite MS at 10 years (see Table 2 below). As in adult studies, those patients converting to MS were more likely to do so early; however, the longer the follow-up interval, the more patients there were who developed MS. [6]
A smaller study by Wilejto et al found that 36% of children with optic neuritis developed MS. [8] All who did had abnormalities on the initial MRI, and bilateral cases were more likely to go on to develop MS.
Table 2. Life-Table Analysis of the Risk for Development of MS in Children With an Isolated Attack of Optic Neuritis [9] (Open Table in a new window)
Age |
Risk for Development of MS |
10 years |
13% |
20 years |
19% |
30 years |
22% |
40 years |
26% |
Both adults and children with more severe optic disc swelling are less likely to develop MS, and those with both severe optic disc swelling and retinal exudates rarely develop MS.
Patient Education
With Uhthoff symptom, patients who have had demyelinating lesions with recovery often have symptoms return with exercise, exposure to heat (eg, hot baths), or febrile illnesses; a rapid return to baseline occurs when body temperature returns to normal. Warning patients about Uhthoff symptom is important so that they do not think they are having a recurrence.
For excellent patient education resources, see eMedicineHealth's patient education article Multiple Sclerosis.
-
Optic disc swelling in the right eye and left eye in a child with bilateral optic neuritis.
-
Neuroretinitis in the right eye of an adolescent with cat scratch disease. The optic nerve is swollen, and a deposition of yellowish exudate in the nerve fiber layer of the macula produces a macular star.
-
T1 contrast enhanced axial section of an MRI of the orbital optic nerve of a child with optic neuritis on the left side. The arrows point to the left optic nerve that enhances along its entire orbital course.
-
T1 contrast enhanced coronal section of the MRI of the orbital optic nerve. The arrow points to the enhancing left optic nerve.
-
T1 contrast enhanced axial section of an MRI of the intracranial optic nerves. Enhancement of both optic nerves is seen. The arrow indicates the left optic nerve.
-
T1 contrast enhanced coronal section of the MRI showing the optic nerves that both enhance. The arrow points to the left optic nerve.
-
T2 axial section of an MRI through the cerebral hemisphere of a boy with bilateral optic neuritis. Note high-signal abnormalities in the cerebral white matter that are most prominent in the posterior hemispheres. This is suspicious for mild acute disseminated leukoencephalitis.
-
T2 axial sections of MRI of a man with optic neuritis showing scattered white matter lesions. The arrows point to 2 examples of the numerous lesions.