Practice Essentials
When treating complex apical orbital fractures, surgeons must be familiar with endoscopic as well as trancranial approaches. Therefore, management should involve a multidisciplinary approach, including ophthalmology, facial trauma surgery and neurosurgery.
Background
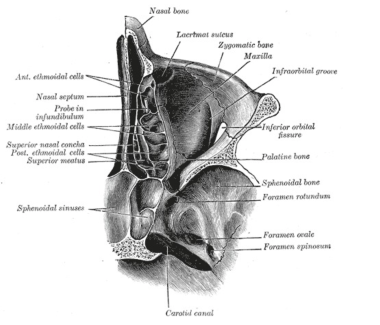
The orbital apex is the most posterior portion of the pyramidal-shaped orbit, positioned at the craniofacial junction. The anatomy of the orbital apex is significant for the complex association between bony, neural, and vascular elements. [1] Fractures of the apex rarely are isolated because they occur in the association with or as extension of fractures of the facial skeleton, base of skull, or other more anterior orbital fractures. They are usually seen after severe trauma to the head. Apical fractures may include the posterior lateral or medial walls, the posterior roof, and the optic canal. Very posterior orbital fractures are uncommon because of the anatomy of this region. The apex is made up of the posterior medial wall medially, the lesser wing of the sphenoid superiorly and the greater wing of the sphenoid laterally. The superior and lateral walls are made of thick bones which need considerable force to fracture.
 Axial CT scan exhibiting a left apex fracture through the optic canal. Note associated lateral wall and medial wall fractures. This patient also required a craniotomy for a subdural hematoma.
Axial CT scan exhibiting a left apex fracture through the optic canal. Note associated lateral wall and medial wall fractures. This patient also required a craniotomy for a subdural hematoma.
The anatomy of the orbital apex should be reviewed briefly, with emphasis on the neurovascular structures traversing the optic canal, superior orbital fissure (SOF), and inferior orbital fissure.
Two bony roots that connect the lesser wing of the sphenoid with the body of the sphenoid form the optic canal. The inferior root separates the optic canal from the superior orbital fissure and also is referred to as the optic strut. The superior root forms the roof of the optic canal and separates it from the anterior cranial fossa. The body of the sphenoid forms the medial wall of the canal. From an anterior view, the entrance to the optic canal is the most superior and medial structure in the apex. Each optic canal passes posteromedially at an angle of approximately 35° to the sagittal and opens posteriorly into the chiasmatic groove (which terminates posteriorly at the tuberculum sellae). The canal has an intimate relationship to the sphenoid sinus, and with extensive sinus pneumatization, the optic canal may become completely surrounded by a posterior ethmoidal Onodi air cell, the sphenoid sinus, or an aerated anterior clinoid process.
In adults, the canal is 6.5 mm in diameter and about 8 to 12 mm in length. The canal transmits the optic nerve and the ophthalmic artery. Throughout its intraorbital and intracanalicular course, the optic nerve is surrounded by pia mater, arachnoid, and dura mater, giving the nerve a sheath. Therefore, optic nerve is a white matter tract of the brain and carries with it meningeal coverings. Within the orbit, the optic nerve is quite mobile; however, within the canal, the optic nerve sheath remains adherent to the sphenoid periosteum and thus is fixed.
The SOF is situated between the greater and lesser sphenoid wings, with the optic strut at its superomedial margin. It lies between the roof and lateral wall of the orbit. The SOF is divided at the spina recti lateralis by the annulus of Zinn, the common tendinous origin of the recti muscles. Lateral to the annulus of Zinn, the SOF transmits the lacrimal nerve, frontal nerve, trochlear nerve, the superior ophthalmic vein, and it may transmit a recurrent branch of the lacrimal artery. Within the annulus pass the superior division of III, nasociliary nerve, inferior division of III, abducent nerve, and fibers from the internal carotid sympathetic plexus.
The inferior orbital fissure lies between the orbital floor and lateral wall and communicates with the pterygopalatine and infratemporal fossae. It transmits the maxillary nerve (which continues to give the infraorbital nerve), the zygomatic nerve, the infraorbital artery, venous communications between the inferior ophthalmic vein and the pterygoid plexus, and an orbital branch of the pterygopalatine ganglion.
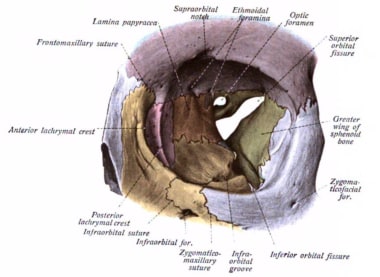 Orbital anatomy showing the bony anatomy and the relationships of the optic canal, the superior and the inferior orbital fissures. Courtesy of Wikimedia Commons [Sobotta's Atlas and Textbook of Human Anatomy, 1909, https://commons.wikimedia.org/wiki/File:Sobo_1909_95.png].
Orbital anatomy showing the bony anatomy and the relationships of the optic canal, the superior and the inferior orbital fissures. Courtesy of Wikimedia Commons [Sobotta's Atlas and Textbook of Human Anatomy, 1909, https://commons.wikimedia.org/wiki/File:Sobo_1909_95.png].
Pathophysiology
Orbital apex fractures may be the result of nonpenetrating blunt trauma, such as seen with motor vehicle accidents or assaults, or penetrating trauma such as with orbital foreign bodies. [2, 3, 4, 5]
Radiographically, orbital apex fractures consist of the following three basic types: linear, without dislocation of fragments; comminuted, usually with fragment dislocation; and apex avulsion, with an intact optic foramen. In a series of 23 apex fractures by Unger in 1984, 20 were comminuted, one was linear, and two consisted of avulsion of the extreme apex with an intact optic foramen within the avulsed fragment. [6] Clinically, fractures into a sinus are technically open fractures, and a risk for contamination from the sinus microbiological flora exists.
Orbital apex fractures present with different symptoms and signs depending on the degree of injury to important neural and vascular structures. [7] Various syndromes have been defined to describe these clinical presentations. However, in view of the complex anatomy and response to injury of the apex, the clinical findings in any single patient may be unreliable in defining the exact site and extent of any fractures seen on neuroimaging. It is apparent that significant injury to the neurovascular structures of the orbital apex may be present without a fracture. [8] Optic canal fractures may be seen in about 50% of patients with posterior traumatic optic neuropathy. [9, 10]
Epidemiology
Frequency
United States
The frequency of recognized orbital apex fractures has increased with the improvement of imaging techniques. Several series reviewed the incidence of fractures with trauma. Unger et al examined 490 patients admitted with nonpenetrating blunt head trauma and found orbital apex fractures in six patients, sphenoid bone fractures in 78 patients (of which eight involved the lesser wing), and 30 injuries that involved the body of the sphenoid bone. Ghobrial et al reviewed 112 consecutive patients with base of skull fractures; 15% had sphenoid fractures.
Mortality/Morbidity
Mortality associated with orbital apex fractures are due to associated intracranial trauma or are associated with injury to the adjacent internal carotid artery. Morbidity is common due to injury to neurovascular structures.
Injury to the optic nerve leads to visual loss, being most commonly from an indirect posterior traumatic optic neuropathy. The visual loss from traumatic optic neuropathy may vary from partial to complete, and the degree of recovery may vary. Also reported is visual loss from optic nerve sheath hematoma, optic nerve transection, and optic nerve impingement from a penetrating foreign body or bony fracture. Vision loss from optic nerve compression associated with retrobulbar hemorrhage also has been reported.
Injury to cranial nerves III, IV, and VI presents as extraocular muscle nerve palsy, with manifest diplopia.
Injury to cranial nerve V presents as sensory disturbance to areas supplied by branches of the trigeminal (V) nerve.
Sex
A review of 490 traumatic blunt head injury patients resulted in a male-to-female ratio of approximately 1.5:1, reported by Unger et al.
-
Axial CT scan exhibiting a left apex fracture through the optic canal. Note associated lateral wall and medial wall fractures. This patient also required a craniotomy for a subdural hematoma.
-
Coronal reconstruction of CT scan of left orbital apex fracture through the optic canal. This patient presented with an orbital apex syndrome. Note the displaced bone fragment from the lateral wall of the sphenoid sinus.
-
Orbital anatomy showing the bony anatomy and the relationships of the optic canal, the superior and the inferior orbital fissures. Courtesy of Wikimedia Commons [Sobotta's Atlas and Textbook of Human Anatomy, 1909, https://commons.wikimedia.org/wiki/File:Sobo_1909_95.png].
-
Bony anatomy of the orbital apex. Courtesy of Wikimedia Commons [Anatomy of the Human Body, 1918, https://commons.wikimedia.org/wiki/File:Gray191.png].