Background
The oculomotor (third) cranial nerve plays an important role in the efferent visual system by controlling ipsilateral eye movements, pupil constriction, and upper eyelid elevation. Accordingly, damage to the third cranial nerve may cause diplopia, pupil mydriasis, and/or upper eyelid ptosis. The clinical manifestations of third cranial nerve dysfunction reflect its constituent parts. Outer parasympathetic fibers supply the ciliary muscles of the eye and the sphincter pupillae (sphincter muscles that cause pupillary constriction). The inner somatic fibers of the third cranial nerve supply the levator palpebrae superioris in the eyelid (controlling upper eyelid elevation), and four extraocular muscles that govern ocular motility (the superior, medial, and inferior recti muscles, and the inferior oblique muscle). [1, 2, 3, 4, 5] Classically, third cranial nerve impairment is associated with a “down and out” appearance of the ipsilateral eye (Figure 1). This eye position reflects the unopposed actions of depression and abduction of the globe, which are governed by superior oblique (innervated by the fourth cranial nerve) and lateral rectus (innervated by the sixth cranial nerve) muscles, respectively. Localizing an isolated third cranial nerve palsy, particularly one that causes a “down and out” position of the ipsilateral eye is relatively straightforward when there is complete involvement of the levator palpebrae superioris (causing complete ptosis), complete paralysis of innervated extraocular muscles, and complete pupillary mydriasis. In reality, however, third cranial nerve palsies are often incomplete and result in partial deficits that may be relatively subtle and easily overlooked (Figure 2). For this reason, it is imperative to carefully establish a good history and perform a thorough examination to localize third cranial nerve lesions, which may herald vision and life-threatening problems.
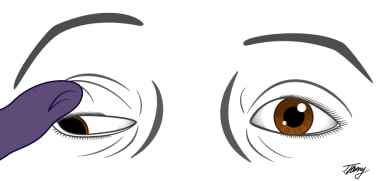 Illustration of a complete right oculomotor palsy demonstrating the classic "down and out" appearance, complete ptosis and mydriasis of the right eye. Courtesy of Tyler Henry, MD, Medical Illustrator (tylerhenrymd.com).
Illustration of a complete right oculomotor palsy demonstrating the classic "down and out" appearance, complete ptosis and mydriasis of the right eye. Courtesy of Tyler Henry, MD, Medical Illustrator (tylerhenrymd.com).
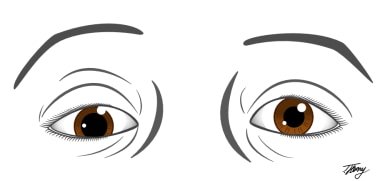 Illustration of a partial right oculomotor nerve palsy demonstrating incomplete ptosis, hypotropia and mydriasis of the right eye. Courtesy of Tyler Henry, MD, Medical Illustrator (tylerhenrymd.com).
Illustration of a partial right oculomotor nerve palsy demonstrating incomplete ptosis, hypotropia and mydriasis of the right eye. Courtesy of Tyler Henry, MD, Medical Illustrator (tylerhenrymd.com).
Pathophysiology
The third cranial nerve, alternatively known as the oculomotor nerve, has multiple important functions. Owing to its elegant anatomical organization and course, third cranial nerve deficits can be readily localised to specific site (nucleus, fascicular portion, cavernous sinus segment, or orbit), depending on the pattern of oculomotor dysfunction observed and associated clinical findings. Broadly speaking, nuclear third cranial nerve palsies may be isolated, or accompanied by other neurologic symptoms given the proximity of the oculomotor nucleus to other important structures in the midbrain tegmentum. [1, 2, 3, 4] The fascicular portion of the oculomotor nerve courses ventrally from the nucleus in the midbrain, crosses through the red nucleus near the corticospinal tract, and emerges from the medial aspect of the cerebral peduncle (Figure 3). [4] Its close proximity to other midbrain structures means that fascicular lesions often co-associate with neurological findings, in addition to oculomotor palsy. [4] The cisternal portion of the third cranial nerve travels in the subarachnoid space anterior to the midbrain after exiting between the superior cerebellar and posterior cerebral arteries (Figure 3). Here, it is vulnerable to compressive effects from vascular lesions, such as aneurysms (Figure 4). The oculomotor nerve runs through the lateral wall of the cavernous sinus. [4] Lesions of the cavernous sinus often produce third nerve palsies that are accompanied by one or more other neurologic findings including palsies of the fourth, fifth (first division), and sixth cranial nerves, with or without an associated Horner syndrome. [4] Finally, the oculomotor nerve enters the orbit through the superior orbital fissure adjacent to the fourth cranial nerve. Usually, the third cranial nerve branches into superior and inferior divisions within the posterior orbit, but, occasionally, divisional branching occurs in cavernous sinus. The superior division of the third cranial nerve innervates the levator palpebrae and the superior rectus muscles. The inferior division innervates all the other muscles innervated by the third nerve, and supplies the preganglionic parasympathetic fibers to the ciliary ganglion, which in turn innervate the iris sphincter. [4] As a general rule of thumb, orbital lesions may be associated with other clinical signs such as proptosis, which can help in the localization process. A more detailed description regarding how anatomical site of injury impacts third cranial nerve function is discussed in the sub-section ”Localizing Third Cranial Nerve Palsies: How Does Form Affect Function?”
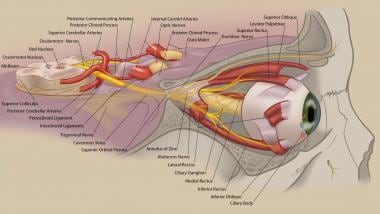 Anatomy of the oculomotor nerve. Courtesy of Tyler Henry, MD, Medical Illustrator (tylerhenrymd.com).
Anatomy of the oculomotor nerve. Courtesy of Tyler Henry, MD, Medical Illustrator (tylerhenrymd.com).
Epidemiology
Frequency
In a recent population-based cohort study by Fang and colleagues [6] , 145 cases of acquired third cranial nerve palsy diagnosed over a 37-year period in Olmsted County, Minnesota were assessed. The age- and sex-adjusted annual incidence of acquired third nerve palsy was 4.0 per 100 000. [6] Not surprisingly, the annual incidence was higher in older patients (aged greater than 60 years) relative to younger patients (12.5 vs 1.7 per 100 000; difference, 10.8 per 100 000; P < .001). [6] This observation likely reflected the higher predilection for microvascular ischemic third nerve cranial nerve palsies in older versus younger adults. [6] In this study, the most common causes of acquired third nerve palsy were presumed microvascular injury (42%), trauma (12%), compression (from neoplastic lesions) (11%), post-operative neurosurgical cases (10%), and aneurysmal compression (6%). [6] Notably, 10 patients (17%) with microvascular ischemic third nerve palsies had pupil involvement, whereas pupil involvement was seen in not all, but only 16 patients (64%) with compressive third nerve palsies. [6] The findings from Fang et al [6] bear careful consideration, because although compressive lesions had a higher likelihood of pupil involvement, pupil involvement did not exclude microvascular third nerve palsy; moreover, lack thereof did not rule out potentially life-threatening causes of compressive third nerve palsy.
Mortality/Morbidity
The morbidity and mortality caused by third cranial nerve palsies are intrinsically linked to etiology, the details of which are beyond the scope of this article.
That said, several important causes of mortality and morbidity presenting with evidence of oculomotor dysfunction include: subarachnoid hemorrhage from a ruptured aneurysm of the posterior communicating artery, meningitis, and infiltrative meningeal processes. [4]
Prognosis
The overall prognosis of any oculomotor palsy depends on the etiology. Post-traumatic, post-infectious, post-inflammatory, and ischemic oculomotor palsies may spontaneously recover to a variable degree. [4] Compressive lesions (including aneurysm or tumor) may also improve or resolve after appropriate surgical intervention. [4] Cause notwithstanding, patients with chronic and stable ptosis or ophthalmoplegia due to oculomotor nerve palsy may benefit from reconstructive lid or strabismus surgery over the course of their follow up. [4]
Patient Education
Patients should be informed regarding potentially life-threatening causes of an acquired third cranial nerve palsy, appropriately weighted to the context of their case. Accordingly, they should undergo appropriate evaluation and treatment of their third cranial nerve palsy in a manner that is tailored to their needs. Finally, patients should be provided information that facilitates a good understanding regarding the implications of their diagnosis and prognosis for recovery.
-
Illustration of a complete right oculomotor palsy demonstrating the classic "down and out" appearance, complete ptosis and mydriasis of the right eye. Courtesy of Tyler Henry, MD, Medical Illustrator (tylerhenrymd.com).
-
Illustration of a partial right oculomotor nerve palsy demonstrating incomplete ptosis, hypotropia and mydriasis of the right eye. Courtesy of Tyler Henry, MD, Medical Illustrator (tylerhenrymd.com).
-
Anatomy of the oculomotor nerve. Courtesy of Tyler Henry, MD, Medical Illustrator (tylerhenrymd.com).
-
Illustration of common causes of an oculomotor nerve palsy. Courtesy of Tyler Henry, MD, Medical Illustrator (tylerhenrymd.com).









