Background
In 1869, von Graefe first used the term malignant glaucoma to describe an entity characterized by elevated intraocular pressure (IOP) with a shallow or flat anterior chamber in the presence of a patent peripheral iridectomy. In its classic form, malignant glaucoma is rare but one of the most serious complications of glaucoma filtration surgery in patients with narrow-angle or angle-closure glaucoma. [1, 2]
The term malignant glaucoma refers to a sustained ongoing process that is difficult to treat and may progresses to blindness. It is sometimes unresponsive and occasionally worsened with conventional management. Modern vitreoretinal surgical techniques, as well as a better understanding of the disease, have improved the prognosis to some extent.
Many different terms, including ciliovitreal block and aqueous misdirection syndrome, have been proposed based on diverse unproven pathophysiologic and anatomic mechanisms.
Pathophysiology
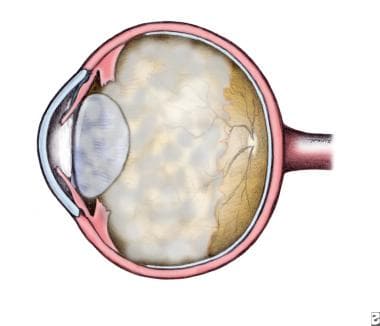
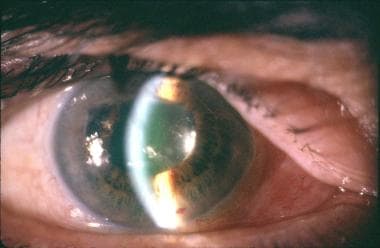
A blockage of the normal aqueous flow at the level of the ciliary body, lens, and anterior vitreous face is believed to cause malignant glaucoma. Posterior misdirection of aqueous humor into the vitreous cavity occurs producing a continuous expansion of the vitreous cavity and increased posterior segment pressure. This accumulation of aqueous fluid in the vitreous cavity causes anterior displacement of the lens-iris diaphragm in phakic and pseudophakic eyes or forward displacement of the anterior hyaloid in aphakic patients. Corneal edema is a frequent finding. [3] The resulting shallow or flat chamber (athalamia) [4] is believed to exacerbate the condition because of the decreased access of aqueous to the trabecular meshwork. The IOP often is markedly increased but may be normal. [5, 6]
Epstein et al proposed that forward displacement of the vitreous into apposition with the posterior ciliary body caused a decrease in available hyaloid surface, increasing the resistance to flow from the vitreous body. [7] Small hyperopic eyes are at higher risk for malignant glaucoma.
Malignant glaucoma has been described following: cataract surgery with or without intraocular implant (aphakic or pseudophakic malignant glaucoma), implantation of a large posterior chamber intraocular lens, cessation of topical cycloplegic therapy, induction of miotic therapy, laser iridotomy, laser capsulotomy, Nd:YAG cyclophotocoagulation, laser sclerotomy, Molteno implantation, Baerveldt glaucoma drainage device implantation, viscoelastic use, intravitreal injection of triamcinolone acetonide, Aspergillus flavus intraocular infection, and acute hydrops in Down syndrome. [8] Malignant glaucoma also has been described spontaneously in an eye with no antecedent of surgery or miotics. Surgical iridectomy had a 2% complication before YAG laser largely replaced the procedure. A pseudomalignant glaucoma syndrome has been reported after pars plana vitrectomy.
 Malignant glaucoma subsequently developed in a 70-year-old man with a history of nanophthalmos who underwent cataract extraction with spherical piggyback IOL implantation.
Malignant glaucoma subsequently developed in a 70-year-old man with a history of nanophthalmos who underwent cataract extraction with spherical piggyback IOL implantation.
Malignant glaucoma with a low IOP has been described after trabeculectomy. [9] In these cases, the pressure in the anterior chamber is lower than the pressure in the vitreous, causing shallowing of the anterior chamber. A functioning iridectomy and sclerotomy must be present for the fluid to escape and keep the pressure low. Anterior rotation of the ciliary processes has been observed. Choroidal effusion may not be present. [9] In a different case, trabeculectomy was complicated with unplanned zonulectomy and ciliovitreal block caused by vitreous herniation through the peripheral iridectomy. High IOP and a flat anterior chamber were observed. [10]
Epidemiology
Frequency
United States
Malignant glaucoma has been reported to occur in 0.6-4% of eyes following filtration surgery for angle-closure glaucoma. Trope et al reported that 71% of 14 patients with malignant glaucoma had chronic angle-closure glaucoma. [11]
International
In Germany, Duy and Wollensak reported 2 cases of ciliary block in 9000 patients following cataract extraction. [12] However, both patients had previous filtration procedures with temporary shallowing of the anterior chamber postoperatively. In China, Wu et al reported an incidence of 2% in patients with chronic angle-closure glaucoma surgery. [13]
Mortality/Morbidity
Malignant glaucoma remains a difficult clinical problem that results in irreversible blindness if not promptly treated. The surgeon should be aware preoperatively of eyes at risk and observe them closely postoperatively. Early recognition is the most important step to prevent irreversible vision loss. [14]
Age
Trope et al reported that the average age of patients with malignant glaucoma was 70 years. [11]
Prognosis
The prognosis depends on the length and the severity of the attack. In patients with relatively healthy optic nerves, the prognosis can be good if the attack is abated and intraocular pressure is controlled. [15]
Patient Education
For patient education resources, see the Glaucoma Center, as well as Glaucoma FAQs and Understanding Glaucoma Medications.
-
Phakic malignant glaucoma.
-
Malignant glaucoma subsequently developed in a 70-year-old man with a history of nanophthalmos who underwent cataract extraction with spherical piggyback IOL implantation.