Background
Angle-recession glaucoma is classified as a type of traumatic secondary open-angle glaucoma. [1] This condition may be underdiagnosed because onset is often delayed and because a history of eye injury may be distant or forgotten.
Traumatic glaucoma refers to a heterogeneous group of posttraumatic ocular disorders with different underlying mechanisms that lead to the common pathway of abnormal elevation of intraocular pressure (IOP) and increased risk for optic neuropathy.
Angle recession, with or without glaucoma, is a common sequela of blunt ocular trauma and one characterized by a variable degree of cleavage between the circular and the longitudinal fibers of the ciliary muscle. Traumatic microhyphema and gross hyphema are both equally associated with a high risk for angle recession. [2, 3]
Treacher Collins based the first report of this postcontusional angle deformity on gross examination of enucleated eyes in 1892.
In 1944, D'Ombrain observed the association of ocular trauma and chronic unilateral glaucoma, suggesting abnormalities in the region of the trabecular meshwork as the underlying cause. This theory was substantiated by the classic histologic findings of angle recession published in 1962 by Wolf and Zimmerman, [4] and numerous authors have confirmed the relationship of glaucoma with traumatic angle abnormalities.
Although a relatively uncommon phenomenon, angle-recession glaucoma may be overlooked in the management of nonpenetrating eye trauma. [5] Long-term follow-up care of patients with recognized contusional angle abnormality is warranted because of the risk of delayed asymptomatic onset.
Pathophysiology
The mechanism of glaucoma associated with angle recession appears to involve five processes.
First, blunt force delivered to the globe initiates an anterior to posterior axial compression with equatorial expansion. Sudden indentation of the cornea may be a key factor in angle trauma, creating a hydrodynamic effect by which aqueous is rapidly forced laterally, deepening the peripheral anterior chamber and increasing the diameter of the corneoscleral limbal ring. Ballistic experiments using porcine eyes have demonstrated relatively low energy impact thresholds of 3.5-7.0 joules resulting in moderate-to-severe angle recession. [6]
Second, this transient anatomic deformity results in a shearing force applied to the angle structures, causing disruption at the weakest points if the force applied exceeds the elasticity of the tissues.
Third, although multiple anterior segment structures can be damaged by the above mechanism, a common site of avulsion involves the ciliary muscle. In angle recession, the ciliary body is torn in a manner such that the longitudinal muscle remains attached to its insertion at the scleral spur, while the circular muscle, with the pars plicata and the iris root, is displaced posteriorly. A mechanism of forceful asymmetric contraction of ciliary fibers combined with an intrinsically weak anatomic zone has been suggested. [7]
During traumatic separation of the circular and longitudinal ciliary structures, shearing of the anastomotic branches of the anterior ciliary arteries can occur, resulting in a hyphema. The anterior chamber typically becomes abnormally deep in the meridians of recessed angle due to posterior deviation of the relaxed iris-lens diaphragm. Subsequently, a fissure representing the separation of the longitudinal and circular fibers may be visible by gonioscopy or by histologic examination. [7]
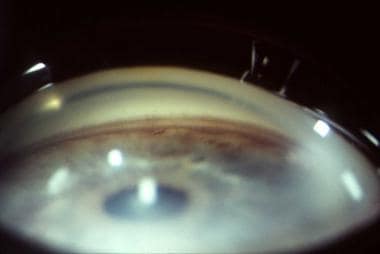
 Angle recession. Note the marked posterior displacement of the iris, with a wide ciliary body band posterior to the scleral spur.
Angle recession. Note the marked posterior displacement of the iris, with a wide ciliary body band posterior to the scleral spur.
Fourth, in some cases, angle recession progresses to glaucoma. The contusional deformity, when extensive, may result in trabecular dysfunction, which may lead to early or delayed loss of outflow facility and elevation of IOP. The mechanism is not well understood, but evidence suggests an increased incidence of primary open-angle glaucoma (POAG) in the other eye of affected patients. One theory suggests that patients with angle-recession glaucoma have an independent, perhaps genetic, predisposition to chronically diminishing trabecular function in both eyes. A finite portion of the trabecular meshwork in eyes with angle recession is initially rendered dysfunctional by the injury and/or the healing process. With time, the outflow capacity of the remaining meshwork is gradually reduced because of preexisting innate factors; the ultimate result is elevated IOP. [7]
Fifth, chronic elevation of IOP leads to optic neuropathy characterized by progressive optic cupping and visual field loss.
Epidemiology
Frequency
United States
The reported frequency of angle recession as a complication of blunt trauma is 20-94%. Several reports have described incidences of angle recession in more than 75% of bluntly injured eyes. [4] Angle recession after traumatic hyphema occurs in 71-100% of cases.
Of eyes with identifiable angle recession, 0-20% develop glaucoma. The onset of glaucoma is extremely variable, ranging from immediately after trauma to months or even many years later. Two peak incidences have been suggested to represent the early and late onset of angle-recession glaucoma; this observation may indicate separate pathologic mechanisms. The underlying differences are not well understood. The risk of eventual progression to glaucoma is generally thought to be proportionate to the extent of the angle recession, [8] though the presence of angle recession alone is not a good predictor of glaucoma. Other risk factors for progression to glaucoma after ocular contusion include chronic elevation of intraocular pressure, poor initial visual acuity, advancing age, lens injury, hyphema, and microhyphema. [8, 9, 10, 11, 12] No difference has been shown between the incidences of angle-recession glaucoma when comparing hyphema versus microhyphema. [12]
Glaucoma after angle recession of less than 180° is unusual; recessions greater than 180° are associated with a 4-9% incidence of glaucoma. Eyes with angle recession of greater than 240° appear to be at the highest risk of chronic glaucoma.
More than 1 million Americans have ocular injuries each year. A 1988 population-based study of adults in New England yielded an annual rate of 9.75 eye injuries per 1000 population based on self-reported histories. [13] In 1990, the estimated hospitalization rate with ocular trauma was 15.2 cases per 100,000 children per year. [14]
Work-related injuries have been reported as 13-18% of all cases of eye trauma. Injuries at home account for 27-31%, followed by assault (11-37%), sports and recreation (about 25%), travel (about 5%), and miscellaneous causes (eg, injuries at school, unknown causes; < 5%). [15, 16, 17, 18, 19, 20, 21] Rates of bilateral injuries are as high as 27%.
The incidence of angle recession in the United States is not reported, but it has been described in 20-94% of eyes affected by blunt trauma. A 1987 study involving the routine examination of asymptomatic boxers found angle recession in 19%, with 8% having bilateral angle recession. [22] Blunt eye injuries are estimated to account for more than 60% of all episodes of eye trauma. Angle recession is one of the most common complications after ocular contusion. Angle recession is observed in 71-100% of cases of traumatic hyphema. By contrast, angle-recession glaucoma occurs relatively infrequently. Of those eyes with known angle recession, 7-9% subsequently develops glaucoma. [23]
International
Specific epidemiologic data regarding angle recession in other countries is scarce. Limited, worldwide epidemiologic data regarding eye trauma are similar to findings in the United States; however, differences exist in the high-risk activities leading to eye trauma, especially when rural and urban populations are compared. Most reports verify that contusional injuries represent most cases of eye trauma, but rates of angle recession or traumatic glaucoma are not well documented.
A study of Australian adults older than 40 years yielded a lifetime cumulative rate of eye injury of 21.1%. [24] Among men, the rural rate was 42.1% compared with 30.5% for urban men. Workplace injuries predominated at 60%, with home injuries closer to agreement with the US figure of 24%.
Results of 1995 study of ocular trauma in the Nigerian population were in agreement regarding the rate of home injuries, revealing a rate of 26.4%. [25] This study showed that women and children at the greater risk of sustaining eye trauma during domestic activities.
The 1988 Israeli Ocular Injuries Study showed that injuries occurring at home were the most frequent type of eye trauma in Israel. [26] A 1996 report described a predominance of home injuries in Scotland. [27]
In a 1994 population-based survey on gonioscopy in individuals older than 40 years in a community in South Africa, the authors reported a cumulative prevalence of angle recession of 14.6%. Among eyes with 360° of angle recession, 8% had glaucoma, and the overall prevalence of glaucoma of eyes with any degree of angle recession was 5.5%. [28]
Mortality/Morbidity
Ocular injury is a relatively common comorbidity in patients admitted with major head trauma.
A study in 1999 revealed ocular injuries in 55% of all patients with facial injuries and in 16% of those with major trauma. [29] Angle recession has been reported in 7.5% of cases of zygomatic-complex fractures. [30]
Mortality in association with serious ocular trauma is related to nonophthalmic complications of the underlying trauma, though specific rates have not been reported.
Estimating the public magnitude of visual disability resulting from traumatic glaucoma is difficult because of its chronic nature and the lack of reported outcomes. Published reports of visual outcomes after eye trauma usually describe short-term results.
A 1996 epidemiologic study showed that the annual cumulative incidence of serious ocular trauma necessitating hospital admission is approximately 8 cases per 100,000 population. Of those cases, approximately 13% of patients had a poor visual outcome, and 10.7% had blindness as an outcome. [31]
Angle-recession glaucoma can have onset years after the original episode of trauma. The long-term incidence of substantial vision loss or blindness due to posttraumatic glaucoma has not been reported.
Race
No known racial predilection exists.
Because of the possible relationship of POAG with angle-recession glaucoma, it can be theorized that African Americans may be at an increased risk for glaucoma after contusional eye trauma.
In addition, one urban study reported in 1991 showed that, at an inner-city hospital in Los Angeles, African-American patients had eye injuries more than twice as frequently as Hispanic patients. [32]
A comparison of the rates of progression to angle-recession glaucoma among different races has not yet been reported.
Sex
No sex predilection has been reported specifically for angle-recession glaucoma, but blunt eye injuries are significantly more common in males.
A strong predominance of eye trauma exists in men, with a male-to-female ratio of 4:1. Therefore, it may be assumed that angle recession and angle-recession glaucoma occur most frequently in men.
Among children, eye injuries occur more frequently in boys than girls.
Compared with men, women appear to be at greater risk of sustaining eye injuries at home.
Age
Advancing age has been reported as an independent predictive factor for the risk of developing glaucoma after ocular contusion injury.
Because of the potential for delayed or late onset after a blunt injury, angle-recession glaucoma is most likely diagnosed in mid or late adulthood. It may be misidentified as POAG because late angle abnormalities may be subtle on examination. A distant or even forgotten history of eye trauma may result in the condition being overlooked, especially in elderly persons.
In general, ocular trauma occurs most commonly during young adulthood. Participation in sports appears to be a risk factor. An 18% incidence of angle recession following cricket ball injury has been reported. [33]
The annual incidence of pediatric eye injuries has been reported at 15 cases per 100,000 population. Pediatric ocular trauma is predominantly associated with playing sports and engaging in outdoor activities. Angle-recession glaucoma has been described in childhood, with a reported pediatric incidence of 19% following closed globe injury and 7% following open globe trauma. [34]
Among adults, the risk of injury appears to steeply decline with advancing age. Studies of urban populations have indicated that elderly persons have only 1.6% of all eye traumas, and for persons older than 65 years, eye injuries are most often the result of a fall.
Prognosis
Owing to the highly variable clinical course of angle recession and angle-recession glaucoma, the prognosis of these conditions cannot be generalized. It is widely accepted that a greater extent of angle recession, especially over 180°, is associated with an increased long-term risk of glaucoma. No epidemiologic data characterizing long-term visual outcomes of eyes with chronic angle-recession glaucoma have been published. As with other types of glaucoma, angle-recession glaucoma can result in progressive visual field loss and blindness. The risk for vision loss depends on many factors, particularly timeliness of initial diagnosis and response to treatment.
No formal data indicate the long-term visual outcomes of eyes with chronic angle-recession glaucoma. Eyes that develop early-onset angle-recession glaucoma are thought to represent a subgroup with most extensive angle injury, but the visible degree of angle recession is not correlated with the severity of glaucoma in this group.
Angle recession of more than 180° is a risk factor for glaucoma. [2] Late-onset angle-recession glaucoma almost always occurs in eyes with more than 180° of angle recession, and the risk appears to increase with the extent of angle recession. Eyes with a 360° angle recession are at greatest risk.
As in most types of glaucoma, angle-recession glaucoma can cause progressive visual field loss and blindness. [35] The risk of visual loss depends on many factors, particularly the timeliness of initial diagnosis and the course of management. Response of elevated IOP to medical therapy varies, and with time, IOP control may deteriorate despite dependence on multiple medications. Favorable results have been reported for surgical intervention of angle-recession glaucoma, but success rates are lower than those of other forms of glaucoma.
Patient Education
Patients with angle recessions of greater than 180°, without evidence of glaucoma, should be advised of the need for lifelong follow-up care.
For patient education resources, see the Glaucoma Center, as well as Angle Recession Glaucoma, Understanding Glaucoma Medications, and Glaucoma FAQs.
-
Irregular widening of the visible ciliary body in a quadrant with angle recession.
-
Angle recession. Note the marked posterior displacement of the iris, with a wide ciliary body band posterior to the scleral spur.
-
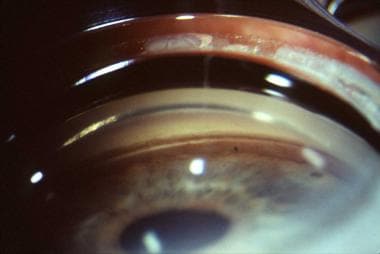
Gonioscopic examination many years after blunt trauma in a patient with angle-recession glaucoma. Note the irregular contour of the iris, with loss of detail of angle structures. Classic findings of angle recession may become subtle or be obscured over time.