Terminology
Bulbar conjunctiva - mucosal epithelium lining the surface of the eye
Palpebral conjunctiva - mucosal epithelium lining the inner surface of the eyelid
Caruncle - fleshy protuberance in the inner corner (canthus) of the eye
Fornix - loose fold of conjunctiva at the reflection from the bulbar to the palpebral conjunctiva, present superiorly and inferiorly
TNM classification - A system to describe the amount and spread of cancer in a patient's body, using TNM.
-
T describes the size of the tumor and any spread of cancer into nearby tissue;
-
N describes the spread of cancer to nearby lymph nodes, and
-
M describes metastasis (spread of cancer to other parts of the body).
Overview
Malignant melanoma of the conjunctiva presents as a raised pigmented or non-pigmented lesion. [1]
This lesion is uncommon but potentially lethal. It can arise in previously unblemished and unpigmented regions (approximately 10% of cases), from a preexisting nevus (about 20% of cases), or the flat, spreading pigmentation of primary acquired melanosis with atypia (60%-70% of cases).
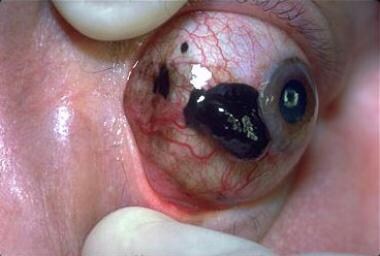 Conjunctival melanomas may be associated with primary acquired melanosis (75%) or may arise from a preexisting nevus or de novo. Reprinted from University of Utah, Peter DeBry, Kwok Li, and Nick Mamalis, MD, Ophthalmic Pathology: An Internet Ocular Pathology Archive, with permission from University of Utah Ophthalmic Pathology.
Conjunctival melanomas may be associated with primary acquired melanosis (75%) or may arise from a preexisting nevus or de novo. Reprinted from University of Utah, Peter DeBry, Kwok Li, and Nick Mamalis, MD, Ophthalmic Pathology: An Internet Ocular Pathology Archive, with permission from University of Utah Ophthalmic Pathology.
 Conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
Conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
 Conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
Conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
 Tarsal conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
Tarsal conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
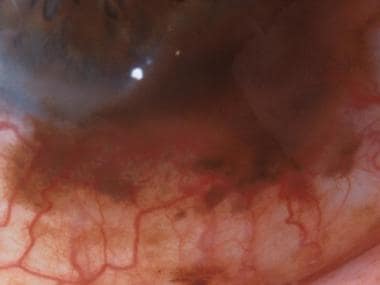
 Invasive conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
Invasive conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
In addition to spreading by lymphatics and the bloodstream, conjunctival melanoma can undergo direct extension to the eyeball and orbit. [2]
The most frequent site of metastasis is the lung, followed by the liver, brain, and bone. In managing these patients, palpating the regional lymph nodes is important because the spread to the conjunctival sac's ipsilateral preauricular, submandibular, and cervical nodes is well recognized. Cohen et al. reported an isolated gastric metastasis from a conjunctival melanoma. [3] Gastric metastases are frequently seen in cutaneous melanoma.
Go to Ciliary Body Melanoma, Choroidal Melanoma, and Iris Melanoma for complete information on these topics.
Etiology
Together with mucus-secreting goblet cells within the stratified epithelium, melanocytic cells are found in the basal layer of the conjunctiva. These melanocytic cells are of neuroectodermal origin, and melanocytic tumors may arise from these cells.
Theoretically, conjunctival melanoma may originate from primary acquired melanosis, preexisting nevi, or de novo lesions (without any histologic or clinical evidence of a preexisting lesion). It may be challenging to determine the precursor lesion in many cases. [4]
Primary acquired melanosis
Approximately 50% to 75% of cases of conjunctival melanoma arise in a setting of primary acquired melanosis. Typically, primary acquired melanosis is found in middle-aged whites; along with malignant melanomas, it is infrequent in the younger population.
The natural history of primary acquired melanosis begins with the development of superficial epithelial pigmentation, with a typical peppered pigment distribution. These lesions can slowly evolve over the years, waxing and waning, extending radially over larger areas of conjunctiva and skin.
Nevus
Evidence indicates that approximately 20% to 25% of patients with conjunctival melanoma have a history or microscopic evidence of a benign conjunctival nevus.
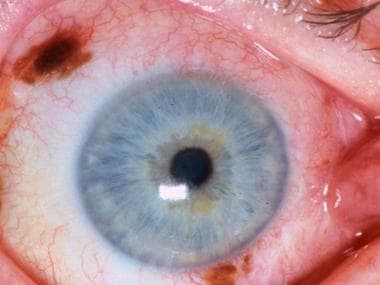
 Conjunctival nevus. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
Conjunctival nevus. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
Malignant melanomas arising from nevi (they may arise from junctional and compound nevi) usually appear as a change (increasing nodularity, variegated pigmentation, bleeding, or inflammation) in known pigmented lesions of the conjunctiva. Still, it may be impossible to establish a clear clinical history of a preexisting history of nevus.
Occasional reports of cases showing the presence of both acquired melanosis and a nevus have been documented.
However, some uncertainty surrounds the role of nevi in the histogenesis of malignant melanoma. Previously, compressed cells at the melanoma base were considered nevi, but reports now suggest that these flattened cells are, in fact, compressed melanoma cells and not nevus cells.
De novo
Approximately 25% of cases of conjunctival melanoma come from de novo lesions. These lesions can be ulcerative, amelanotic, papillary, or fungating.
Epidemiology
Incidence in the United States
Primary malignant melanoma of the conjunctiva is much less common than intraocular or skin melanomas. Malignant melanoma of the conjunctiva accounts for only 5% of all ocular malignancies. [1]
International Incidence
A population-based study of conjunctival melanoma incidence across all Canadian provinces and territories during 1992-2010 used two independent population-based registries that reported that the mean annual incidence rate of CM in Canada was 0.32 cases per million individuals. [5]
The incidence of primary acquired melanosis with atypia or malignant melanoma of the conjunctiva has been estimated to be 0.052 cases per year per 100,000 population in Denmark. [6] The overall incidence of conjunctival melanoma was 0.5 per million (population) per year. [7]
In the Netherlands, conjunctival melanoma has a reported incidence rate of 0.05 per 100,000 population. [8]
In Sweden, only two new cases of primary malignant melanoma of the conjunctiva were diagnosed in 1987; the age-standardized incidence of conjunctival melanoma is 0.74 cases per 1 million population in men and 0.45 cases per 1 million population in women. The incidence of conjunctival melanoma increased in Sweden between 1960 and 2005. [9]
Race, sex, and age predilections
Conjunctival melanoma occurs predominantly in Whites and rarely is seen in Blacks.
Ghazawi reported in 2020 that conjunctival melanoma occurred in 0.35 and 0.29 cases per million individuals for men and women, respectively, in Canada). [5]
No strong sex predilection has been established.
Typically, conjunctival melanoma occurs in patients in their early 50s. It is rarely seen in people younger than 20, although Strempel and Kroll reported three cases of conjunctival malignant melanoma in children. [10]
Patient History
Eliciting a good history of the growth characteristics of each lesion is essential in patients with conjunctival melanomas. The well-informed patient often is aware of subtle changes that may be crucial in identifying these lesions.
Melanomas that arise without a preexisting conjunctival nevus are usually at the limbus and are believed to initially have a short horizontal growth phase followed by a rapid vertical growth phase.
Melanomas that arise in a preexisting nevus often are characterized by the growth of the lesion or by increased vascularity.
Any nevus that has increased in vascularity, size, or solidity, or that has become fixed to the underlying sclera (nevi are always freely movable over the sclera, except at the fixation point at the limbus) should be suspected of being a malignant melanoma.
In the case of primary acquired melanosis, the onset of malignant degeneration often is heralded by the development of nodular thickening in a previously flat area of pigmentation. Other noteworthy features of malignant degeneration include increased vascularity, fixation of the conjunctiva to the underlying sclera, and hemorrhage.
Physical Examination
The clinical presentation of conjunctival melanoma can vary and depends on the antecedent status of the conjunctiva. Melanoma can be distinguished from primary acquired melanosis by its tendency to become fixed to the underlying tissues, which is not a feature of primary acquired melanosis.
In managing patients with conjunctival melanoma, it is important to palpate the regional lymph nodes because the spread to the ipsilateral preauricular, submandibular, and cervical nodes from the conjunctival sac is well recognized.
Conjunctival melanomas may extend onto the peripheral limbus. Most melanomatous nodules at the limbus affect the peripheral cornea; some grow circumferentially around the limbus. Rarely, a melanomatous nodule may be located more centrally in the cornea.
Pigmentation of the eyelid margins and skin occasionally accompanies primary conjunctival melanomas, particularly those located on the palpebral conjunctiva and fornix; this combined presentation discloses a poorer prognosis.
Other uncommon manifestations include poliosis.
Monitoring
Documentation by photography and observation for the growth of conjunctival melanomas over regular intervals of time is recommended for small lesions.
Differential Diagnosis
Not all conjunctival melanomas are pigmented; melanomas with little or no pigment can look like squamous and sebaceous gland carcinomas, papillomas, lymphoid hyperplasia, and even pterygia. Amelanotic melanomas can puzzle even the pathologist; staining with the S-100 protein stain and the more specific homatropine methylbromide (HMB-45) antibody stain can assist in diagnosis.
Differentials:
-
Conjunctival squamous cell carcinoma
-
Conjunctival melanosis
-
Conjunctival mycosis
-
Conjunctival seborrheic keratosis
-
Acquired melanosis (primary or secondary)
-
Foreign body (eg, graphite)
-
Drug toxicity (eg, epinephrine)
-
Conjunctival pseudomelanoma - Iatrogenic secondary to scleral tunnel
Slit lamp photography
Slit-lamp photography, using properly mounted cameras or DIY smartphone photography, is essential for documenting the location and size of the lesion. This procedure must be performed at every visit to assist in monitoring the progression or regression of the lesion. Serial photography, together with clinical mapping, is a vital tool for tracking the growth and advancement of melanotic conjunctival lesions.
Anterior Segment Optical Coherence Tomography
Anterior segment optical coherence tomography can help reveal hyperreflective subepithelial lesions with significant shadowing in conjunctival melanomas. [11]
Ultrasonographic Biomicroscopy
Extrascleral extension of a ciliary body melanoma sometimes can simulate a conjunctival melanoma. Ultrasonographic biomicroscopy (UBM) of such eyes confirms the presence, character, and extent of the underlying ciliary body tumor and often reveals the route of access of the tumor to the surface by way of a scleral emissary canal. [12]
UBM may be an additional diagnostic tool to estimate the tumor thickness before surgical resection of conjunctival melanoma. [13]
Conjunctival Excision Biopsy
Because acquired melanosis, nevi, melanomas, and other pigmented lesions (eg, papillomas, adrenochrome deposits, foreign bodies, blood-filled cysts) may have comparable clinical features, biopsies of such lesions usually should be taken before more extensive therapy is considered. A biopsy of a malignant melanoma does not seem to augment its lethality and may prevent needless, mutilating surgery. Conjunctiva is an easily accessible tissue source for diagnostic biopsy. [14, 15, 16, 17]
Other diagnostic tools
Impression Cytology
Impression cytology has been reported a few times to have a good correlation with conjunctival melanoma [18] ; however, because impression cytology only evaluates superficial epithelial cells, leaving out deeper lesion components, and morphological changes could be induced in the samples with brush cytology, this is not recommended as an effective diagnostic tool. [19]
Histopathology
Invasive melanoma cells may be small polyhedral, epithelioid, spindled, or ballooned. Detecting the atypical melanocytes of conjunctival melanoma can be difficult, especially when comprised purely of small polyhedral cells. When atypical melanocytes are seen to invade the substantia propria, with loss of maturation and loss of normal polarity, the pathologic diagnosis of conjunctival melanoma is made.
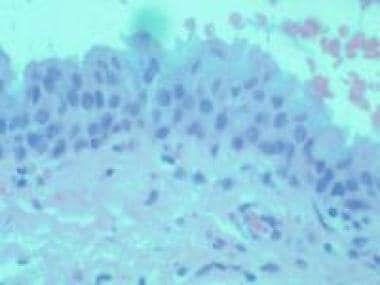 Histologic findings of invasive melanoma cells may be small polyhedral, epithelioid, spindled, or ballooned. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
Histologic findings of invasive melanoma cells may be small polyhedral, epithelioid, spindled, or ballooned. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
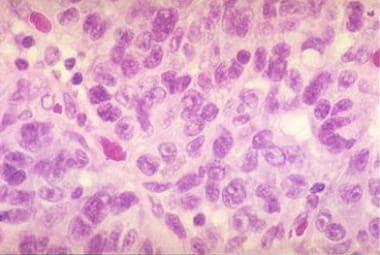 Dysplastic melanocytes may invade beyond the epithelium into the substantia propria or into the globe or lids. Reprinted from University of Utah, Peter DeBry, Kwok Li, and Nick Mamalis, MD, Ophthalmic Pathology: An Internet Ocular Pathology Archive, with permission from University of Utah Ophthalmic Pathology.
Dysplastic melanocytes may invade beyond the epithelium into the substantia propria or into the globe or lids. Reprinted from University of Utah, Peter DeBry, Kwok Li, and Nick Mamalis, MD, Ophthalmic Pathology: An Internet Ocular Pathology Archive, with permission from University of Utah Ophthalmic Pathology.
Melanoma versus Nevus
Melanoma cells are larger than nevus cells and grow as irregular nests or as individual cells in nodules that extend through all the layers of the epidermis and dermis. Typically, these cells have large nuclei with chromatin clumping at the periphery of the nuclear membrane and distinct eosinophilic nucleoli. The ascent of atypical melanocytes to the conjunctival epithelium's surface indicates malignancy. [20]
Amelanotic Conjunctival Melanoma
Not all conjunctival melanomas are pigmented; melanomas with little or no pigment can look like squamous and sebaceous gland carcinomas, papillomas, lymphoid hyperplasia, and even pterygia. Staining with the S-100 protein stain and the more specific homatropine methylbromide (HMB-45) antibody stain can assist in diagnosis. [21]
The Callender classification for melanoma does not apply to conjunctival melanomas.
Classification
This classification applies only to melanoma. Histologic verification of the melanocytic lesion should occur.
The assessment of the cancer is based on inspection, slit lamp examination, palpation of the regional lymph nodes, and, when indicated, radiologic (including computed tomography) and ultrasonographic examination of the orbit, paranasal sinuses, and chest.
Complete resection of the primary site is indicated. Histologic study of the margins and the deep aspect of resected tissues is necessary. Resection or needle biopsy of enlarged regional lymph nodes or orbital masses is desirable. [22, 23, 24]
Clinical Tumor Category and Classification (TNM)
The 2017 AJCC tumor (T), node (N), metastasis (M) classification system offers a classification for conjunctival melanoma based on tumor location and size (T), lymph node status (N), and presence of metastasis (M). [19, 25]
Clinical tumor (c) category and criteria
-
TX – Primary tumor cannot be assessed
-
T0 - No evidence of primary tumor
-
T1 - Tumor of the bulbar conjunctiva
-
T1a - < 1 quadrant
-
T1b - ≥1 to < 2 quadrants
-
T1c – ≥2 to < 3 quadrants
-
T1d - ≥3 quadrants
-
T2 - Tumor of the nonbulbar (forniceal, palpebral, tarsal) conjunctiva, and tumor involving the caruncle
-
T2a - Non-caruncular, and ≤1 quadrant of the non-bulbar conjunctiva involved
-
T2b - Non-caruncular, and >1 quadrant of the non-bulbar conjunctiva involved
-
T2c - Caruncular, and ≤1 quadrant of the non-bulbar conjunctiva involved
-
T2d - Caruncular, and >1 quadrant of the non-bulbar conjunctiva involved
-
T3 - Tumor of any size with local invasion
-
T3a - Globe
-
T3d - Nasolacrimal duct and/or lacrimal sac and/or paranasal sinuses
-
T4 - Tumor of any size with invasion of the central nervous system
Regional lymph nodes (N) category and criteria
-
NX - Regional lymph nodes cannot be assessed
-
N0 - No regional lymph node metastasis
-
N1 - Regional lymph node metastasis
Metastasis (M) category and criteria
-
M0 - No distant metastasis
-
M1 - Distant metastasis
Pathological Tumor (p) category and criteria
-
Tx - Primary tumor cannot be assessed
-
T0 - No evidence of primary tumor
-
Tis - Melanoma confined to conjunctival epithelium
-
T1 - Tumor of the bulbar conjunctiva
-
T1a - Tumor of the bulbar conjunctiva with invasion of the substantia propria, not more than 2.0 mm in thickness
-
T1b - Tumor of the bulbar conjunctiva with invasion of the substantia propria, more than 2.0 mm in thickness
-
T2 - Tumor of the non-bulbar (forniceal, palpebral, tarsal) conjunctiva. and tumor involving the caruncle
-
T2a - Tumor of the non-bulbar conjunctiva with invasion of the substantia propria, not more than 2.0 mm in thickness
-
T2b - Tumor of the non-bulbar conjunctiva with invasion of the substantia propria, more than 2.0 mm in thickness
-
T3 - Tumor of any size with local invasion
-
T3a - Globe
-
T3b - Eyelid
-
T3c - Orbit
-
T3d - Nasolacrimal duct and/or lacrimal sac and/or paranasal sinuses
-
T4 - Tumor of any size with invasion of the paranasal sinuses and/or central nervous system
Stage group
No stage grouping is recommended at this time.
Histopathologic type
This categorization applies only to melanoma of the conjunctiva.
Histopathologic grade
The histopathologic grade, as follows, represents the origin of the primary tumor:
-
GX - Origin cannot be assessed
-
G0 - Primary acquired melanosis
-
G1 - Malignant melanoma arises from a nevus
-
G2 - Malignant melanoma arises from a primary acquired melanosis
-
G3 - Malignant melanoma arises de novo
Medical and Radiologic Care
Tebentafusp (Kimmtrak) is the first drug approved for the treatment of HLA-A*02:01-positive adults with unresectable or metastatic uveal melanoma (mUM). It is a first-in-class bispecific protein comprised of a soluble T-cell receptor (TCR) fused to an anti-CD3 immune-effector function that targets gp100, a lineage antigen expressed in melanocytes and melanoma. Immune-mobilizing monoclonal TCRs against cancer (ImmTAC) molecules bind cells with a peptide derived from an antigen of interest and recruit T-cells to lyse the target cells.
Approval of tebentafusp was based on phase 3 IMCgp100-202 clinical trial results that evaluated overall survival (OS) of tebentafusp compared with the investigator's choice (either pembrolizumab, ipilimumab, or dacarbazine) in patients with previously untreated mUM. The trial randomized 378 patients in a 2:1 ratio to either tebentafusp or the investigator's choice. Results demonstrated OS was 73% in the tebentafusp group compared with 59% in the investigator's choice group (82% pembrolizumab; 13% ipilimumab; 6% dacarbazine) at one year (p< 0.001). Progression-free survival was also significantly higher in the tebentafusp group than in the control group (31% vs 19% at 6 months; P = 0.01). [26]
Mitomycin is an off-label drug that is used in ophthalmology. It is a potent chemotherapeutic agent that inhibits fibroblasts and diminishes scarring after glaucoma filtering surgery. It has been used as an adjunct in pterygium surgery, photorefractive keratoplasty haze management, and conjunctival melanoma management. (Applied topically, however, mitomycin-C has reportedly resulted in an intumescent lens requiring surgical intervention.) [27, 28]
Outpatient radiotherapy is indicated as needed in patients with conjunctival melanoma. [29]
Future Application
BRAF appeared in 35% of reported cases of conjunctival melanoma in Denmark. [7] Ongoing clinical trials evaluate targeted therapies' role as adjuvant and metastatic treatment in conjunctival melanoma. This is potentially useful for advanced nonresectable cases. [30]
Surgical Care
In an adult, all elevated or enlarged pigmented lesions with a history of change should be excised as suspected malignant melanoma.
Note that metastatic melanomas from anywhere in the body and extensions from ciliary body melanomas may first become apparent in the conjunctiva.
The treatment of conjunctival melanoma is surgical, with complete removal of the tumor, if possible. Cryotherapy to the normal-appearing conjunctiva surrounding the lesion is usually performed.
Damato and Coupland reported that high local tumor control rates, with minor ocular morbidity, resulted from the excision of invasive melanoma with adjunctive brachytherapy and topical chemotherapy. [31] This audit also noted that when no caruncular involvement had occurred, disease-specific mortality was rare, except in patients who were referred after a surgical procedure. The investigators' results suggested that inadequate surgical intervention increases local recurrence and metastatic death risks.
The suggestions of Shields in the surgical management of circumscribed conjunctival melanomas are advocated.
The "no touch" technique is essential throughout the procedure. No surgical instrument is used more than once in any area (addressing the concern of microscopically seeding tumor cells).
Treatment of primary conjunctival melanomas in the limbal region of the bulbar conjunctiva can usually be accomplished with initial, localized absolute alcohol epitheliectomy.
This treatment is followed by wide (2- to 3-mm clear zone), local excision by a partial lamellar scleroconjunctivectomy.
Treat the entire area of the lesion because untreated regions may lead to spread through local lymphatic channels. The bed of excision and the adjacent conjunctiva or cornea away from the nodule are treated with supplemental double freeze-thaw cryotherapy using a specific technique (lifting the conjunctiva). Laser therapy after excision has also been used.
Nodal involvement indicates extensive metastatic disease, but occasionally, cases in which lesions were limited to regional nodes and cured by node resection have occurred.
If the tumors are located in the fornical or palpebral conjunctiva, wide surgical resection with alcohol treatment to the scleral base and cryotherapy to the surrounding conjunctiva is performed.
Exenteration of the orbit
Exenteration of the orbit sometimes is necessary for large melanomas that have invaded the orbit, but this procedure does not improve the prognosis. It may be performed for patients to do local debulking of a tumor because this procedure is not linked to increased patient survival. The use of radical neck dissection during the period of exenteration is not without controversy. [32]
The poor survival rate, despite orbital exenteration, suggests that metastasis has already occurred at the time of treatment and confirms that the extent of the disease at diagnosis is the most critical factor in determining the outcome. Considerable orbital invasion indicates the necessity for exenteration; however, subtotal exenteration can be carried out if there is no evidence of the lesion's radial extension to the anterior lid's skin.
Consultations
Consultation with a radiation oncologist is appropriate. [29] As previously stated, Damato and Coupland reported that high rates of local tumor control, with minor ocular morbidity, resulted from the excision of invasive melanoma with adjunctive brachytherapy and topical chemotherapy. [31]
Prognosis
The overall tumor-related mortality rate for conjunctival melanoma is 25% to 26%. This rate increases from 40% to 44% if the tumor has arisen from primary acquired melanosis with an intraepithelial pagetoid growth pattern. This tumor tends to spread first to the parotid or submandibular nodes. [33]
In several studies, the 5-year survival rate for patients with conjunctival melanoma after surgery and/or radiotherapy was 83% to 84%, and the 10-year survival rate was 69% to 80%. The 5-year recurrence rate was 39%.
Paridaens et al. listed the following prognostic factors in conjunctival melanoma (in increasing order of mortality risk) [32] :
-
Two-fold risk - Tumors in unfavorable locations (eg, palpebral conjunctiva, fornices, plica, caruncle, lid margins)
-
Three-fold risk - Mixed cell types, compared with pure spindle-cell types
-
Four-fold risk - Histologic evidence of lymphatic invasion; initial thickness greater than 4 mm for tumors in unfavorable locations only
-
Five-fold risk - Multifocal tumors in patients with lesions in favorable (epibulbar) locations only
As outlined by Jakobiec and associates, other poor prognostic features include moderate-to-severe atypia, a lack of small polyhedral cells in the tumor, invasion of deeper ocular tissues, greater than five mitotic figures per 10 high-power fields, and lack of tumor-induced inflammatory response.
Sheng reviewed 53 cases involving pathologically confirmed conjunctival melanoma in ethnic Chinese patients. Adjuvant therapy and tumor thickness correlated significantly with recurrence-free survival, and tumor stage significantly predicted overall survival. [34]
Questions & Answers
Overview
What is conjunctival melanoma?
What causes conjunctival melanoma?
What is the role of primary acquired melanosis in the etiology of conjunctival melanoma?
What is the role of nevi in the etiology of conjunctival melanoma?
What is the role of de novo lesions in the etiology of conjunctival melanoma?
What is the US prevalence of conjunctival melanoma?
What is the global prevalence of conjunctival melanoma?
Which patient groups have the highest prevalence of conjunctival melanoma?
Which clinical history findings are characteristic of conjunctival melanoma?
Which physical findings are characteristic of conjunctival melanoma?
How should conjunctival melanoma be monitored over time?
Which conditions are included in the differential diagnoses of conjunctival melanoma?
What is the role of slit-lamp photography in the long-term monitoring of conjunctival melanoma?
What is the role of ultrasonographic biomicroscopy (UBM) in the workup of conjunctival melanoma?
What is the role of biopsy in the workup of conjunctival melanoma?
Which histologic findings are characteristic of conjunctival melanoma?
How is conjunctival melanoma treated?
What is the prevalence of BRAF mutations in patients with conjunctival melanoma?
What is the role of surgery in the treatment of conjunctival melanoma?
When is exenteration of the orbit indicated in the management of conjunctival melanoma?
Which specialist consultations are beneficial to patients with conjunctival melanoma?
What is the prognosis for conjunctival melanoma?
How is conjunctival melanoma staged?
What are the clinical classifications for conjunctival melanoma?
What are the pathological classifications for conjunctival melanoma?
What are the stage groupings for conjunctival melanoma?
What are the histopathologic types of conjunctival melanoma?
What are the histopathologic grades of conjunctival melanoma?
-
Conjunctival melanomas may be associated with primary acquired melanosis (75%) or may arise from a preexisting nevus or de novo. Reprinted from University of Utah, Peter DeBry, Kwok Li, and Nick Mamalis, MD, Ophthalmic Pathology: An Internet Ocular Pathology Archive, with permission from University of Utah Ophthalmic Pathology.
-
Dysplastic melanocytes may invade beyond the epithelium into the substantia propria or into the globe or lids. Reprinted from University of Utah, Peter DeBry, Kwok Li, and Nick Mamalis, MD, Ophthalmic Pathology: An Internet Ocular Pathology Archive, with permission from University of Utah Ophthalmic Pathology.
-
Conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
-
Conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
-
Tarsal conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
-
Conjunctival nevus. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
-
An aggressive conjunctival melanoma with lid involvement. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
-
Large conjunctival melanoma that has invaded the orbit. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
-
Histologic findings of invasive melanoma cells may be small polyhedral, epithelioid, spindled, or ballooned. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
-
Conjunctival melanomas. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
-
Invasive conjunctival melanoma. Courtesy of Peter Rubin, MD, Director, Eye Plastics Service, Massachusetts Eye & Ear Infirmary, Boston, MA.
Tables
What would you like to print?
- Terminology
- Overview
- Etiology
- Epidemiology
- Patient History
- Physical Examination
- Differential Diagnosis
- Slit lamp photography
- Anterior Segment Optical Coherence Tomography
- Ultrasonographic Biomicroscopy
- Conjunctival Excision Biopsy
- Other diagnostic tools
- Histopathology
- Classification
- Medical and Radiologic Care
- Surgical Care
- Consultations
- Prognosis
- Questions & Answers
- Show All
- Media Gallery
- References










