Overview
The International League Against Epilepsy (ILAE) classifies the epilepsies along 2 dichotomies: [1, 2] partial (ie, focal, localization-related) versus generalized and idiopathic (genetic) versus unknown or symptomatic. This double dichotomy conveniently allows presentation of the epilepsy classification in a simple table, as shown in Table 1, below.
Table. Classification of the Epilepsies (Open Table in a new window)
|
Generalized |
Localization-Related |
Idiopathic (genetic) |
Childhood absence epilepsy Juvenile absence epilepsy Juvenile myoclonic epilepsy Epilepsy with grand mal seizures on awakening Other idiopathic generalized epilepsies |
Benign focal epilepsy of childhood (2 types) ADNFLE Primary reading epilepsy |
Symptomatic or unknown |
West syndrome Lennox-Gastaut syndrome Other symptomatic generalized epilepsies |
Mesial temporal lobe epilepsy Neocortical focal epilepsy |
Adapted from Tich and Pereon, 1999. [3] ADNFLE = Autosomal dominant nocturnal frontal lobe epilepsy |
||
The term idiopathic was often misunderstood in this setting, and the term “genetic is more informative.” Whereas the term idiopathic in medicine usually means “of unknown cause,” idiopathic epilepsies are not truly of unknown cause; this confusing terminology will most likely be corrected in the upcoming ILAE classification system. [4]
In epilepsy, idiopathic seizures are genetically determined and have no apparent structural cause, with seizures as the only manifestation of the condition. Findings of the neurologic examination and neuroimaging studies are normal, and electroencephalographic (EEG) findings also are normal, aside from the epileptiform abnormalities. In some syndromes, the genetic substrate has even been identified. Most idiopathic epilepsies are generalized, but a few genetic epilepsies are focal.
Nonidiopathic epilepsies, by definition, are not genetic (though some may be associated with a minor genetic predisposition) but are the result of a brain insult or lesion. If the damage is focal, it results in a localization-related epilepsy; if it is diffuse, it results in a generalized epilepsy.
The term cryptogenic was abandoned and replaced by unknown cause.
This article briefly discusses EEG findings in the localization-related (also known as focal or partial) epilepsies.
For patient education information, see the Procedures Center and Brain and Nervous System Center, as well as Electroencephalography (EEG) and Epilepsy.
For more information, see the following:
Waveform Descriptions
Spikes and sharp waves as well as electroencephalographic seizures are briefly reviewed in this section. [5]
Spikes and sharp waves
Spikes and sharp waves are sharp transients that have a strong association with epilepsy. The 2 are distinguished only by their duration (spikes, < 70 ms; sharp waves, 70–200 ms), but they have no differences in terms of clinical significance. Several characteristics distinguish these from benign epileptiform variants (see Focal (Nonepileptic) Abnormalities on EEG), including high amplitudes, which make them "stand out" from ongoing background activity, and aftergoing slow waves, which give the appearance of their "disrupting" background activity. See the following images.
Polyspikes are rarely focal, although focal spikes can at times have a multiphasic polyspikelike morphology.
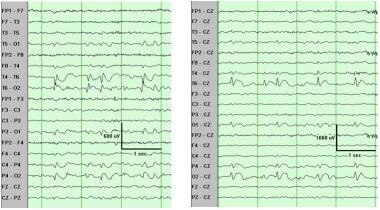 Sharp waves, left temporo-occipital region. The sharp waves are, like any significant epileptiform discharges, followed by slowing and "disruption" of the background. The referential montage (right panel) confirms that the maximum is at T6, closely followed by O2.
Sharp waves, left temporo-occipital region. The sharp waves are, like any significant epileptiform discharges, followed by slowing and "disruption" of the background. The referential montage (right panel) confirms that the maximum is at T6, closely followed by O2.
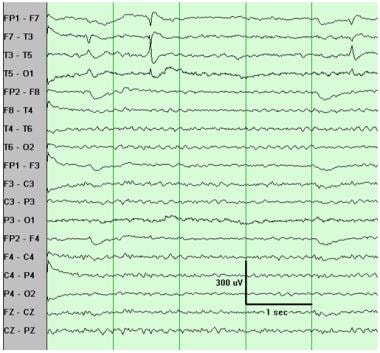 Sharp waves, left temporal region. The maximum (phase reversal) is consistently at T3. Note the associated slow activity and background attenuation.
Sharp waves, left temporal region. The maximum (phase reversal) is consistently at T3. Note the associated slow activity and background attenuation.
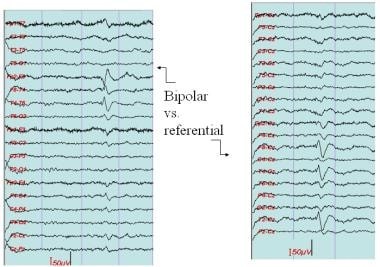 Sharp wave, left temporal region. The sharp wave is, like most significant epileptiform discharges, followed by slowing and "disruption" of the background. The referential montage (right panel) confirms that the maximum is at electrode T2, followed by F8 and T4.
Sharp wave, left temporal region. The sharp wave is, like most significant epileptiform discharges, followed by slowing and "disruption" of the background. The referential montage (right panel) confirms that the maximum is at electrode T2, followed by F8 and T4.
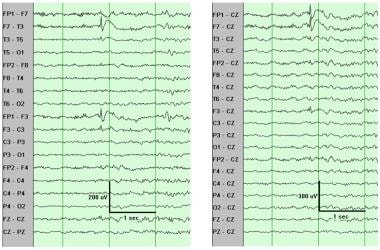 Spike, left frontal region. Note the typical aftergoing slow wave. The referential montage (right panel) shows that the maximum is at Fp1 and F7 about equally, followed by F3.
Spike, left frontal region. Note the typical aftergoing slow wave. The referential montage (right panel) shows that the maximum is at Fp1 and F7 about equally, followed by F3.
EEG seizures
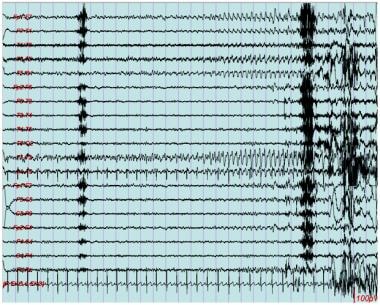
Electroencephalographic seizures are discharges characterized by rhythmicity and evolution ("build-up") in frequency and amplitude (see the image below). The discharge can consist of rhythmic theta or delta activity, or repetitive spikes or sharp waves, but the most characteristic features of electrographic focal seizures are rhythmicity and evolution.
Idiopathic Localization-related Epilepsies
Benign focal epilepsy of childhood is the main localization-related epilepsy that is idiopathic. Two varieties have been well described and are in the 1989 International League Against Epilepsy (ILAE) classification: centrotemporal and occipital. A third type has been described: autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE). [6, 7, 8]
BECTS
Benign childhood epilepsy with centrotemporal spikes (BECTS) is by far the more common. The age of onset is between 4 and 12 years (peak age, 8–9 y). The seizures are simple partial with motor symptoms involving the face, and they tend to occur during sleep or on awakening. Although these focal seizures are the most characteristic seizure types in BECTS, they can be quite subtle and are missed easily, so that the most common mode of presentation is a (secondary) generalized tonic-clonic seizure. As with all idiopathic epilepsy syndromes, neurologic examination findings are normal.
The electroencephalographic (EEG) findings are characteristic, with stereotyped centrotemporal sharp waves that have a characteristic morphology. [9, 10] They are activated markedly by non–rapid eye movement (NREM) sleep, often occur in repetitive bursts, and can be bilateral and independent. Notably, the interictal sharp waves of BECTS often occur in asymptomatic children. In fact, only a minority of children with these discharges may have seizures.
Childhood epilepsy with occipital paroxysms
Childhood epilepsy with occipital paroxysms is less common than BECTS and less consistently benign. It shares all the characteristics of an idiopathic syndrome (ie, normal findings on examination, intelligence quotient [IQ] testing, and neuroimaging studies). The age of onset is 4–8 years. These seizures are rare and primarily nocturnal and often involve visual symptoms. The sharp waves have a maximum occipital negativity, often occur in long bursts of spike-wave complexes, and are activated markedly by eye closure.
ADNFLE
ADNFLE is a genetic localization-related epilepsy. Several mutations of the neuronal nicotinic acetylcholine receptor alpha4 subunit have been identified in association with this epilepsy. It has the expected features of idiopathic (ie, genetic) epilepsies, including onset early in life and normal imaging findings. The seizures are nocturnal and occur in clusters, mimicking parasomnias. They are mostly brief tonic seizures and rare (secondarily) generalized tonic-clonic convulsions, often preceded by a nonspecific aura.
Interictal EEGs may show epileptiform discharges with a frontal predominance, often seen only in sleep. Ictal EEG does not always show definite ictal discharges. Thus, the electroclinical features of ADNFLE are not different from those of symptomatic or cryptogenic frontal lobe epilepsy. Because the genetic findings are variable (ie, locus heterogeneity), its definite diagnosis is largely one of exclusion.
Focal Epilepsies
Focal epilepsy of unknown cause (normal imaging) is by far the most common type of adult-onset epilepsy. By definition, the seizures arise from a localized region of the brain. If the cause is found, they are said to be symptomatic. If imaging study findings are normal, the cause remains unknown.
Clinically, the seizures may be focal aware (previously "simple partial") or focal unaware (previously "complex partial"), with or without focal to bilateral tonic-clonic (previously "secondary generalization"). Interictal electroencephalography (EEG) shows focal spikes or sharp waves, and ictal EEG shows a focal or regional discharge at onset. The main clinical entities are mesial temporal lobe epilepsy, neocortical focal epilepsies, and hemispheric syndromes.
-
Sharp waves, left temporo-occipital region. The sharp waves are, like any significant epileptiform discharges, followed by slowing and "disruption" of the background. The referential montage (right panel) confirms that the maximum is at T6, closely followed by O2.
-
Sharp waves, left temporal region. The maximum (phase reversal) is at T3. The small sharp wave in the 4th second may not be sufficient in itself owing to its small amplitude but, in the context of the definite one, is certainly significant.
-
Sharp waves, left temporal region. The maximum (phase reversal) is consistently at T3. Note the associated slow activity and background attenuation.
-
Sharp waves, left temporal region. The maximum (phase reversal) is at F7 and T1. The small sharp wave that follows would not be sufficient in itself owing to its small amplitude, but in the context of other definite ones, is most likely significant.
-
Sharp wave, left temporal region. The sharp wave is, like most significant epileptiform discharges, followed by slowing and "disruption" of the background. The referential montage (right panel) confirms that the maximum is at electrode T2, followed by F8 and T4.
-
Spike, left frontal region. Note the typical aftergoing slow wave. The referential montage (right panel) shows that the maximum is at Fp1 and F7 about equally, followed by F3.
-
EEG seizure, left temporal region. This is characterized by a rhythmic discharge with "build-up" (ie, evolution in frequency and amplitude).