Overview
The International Classification of Epileptic Syndromes and Epilepsies [1] classifies the epilepsies along 2 dichotomies: (1) partial (ie, focal, localization-related) versus generalized and (2) genetic (idiopathic) versus unknown or symptomatic. This double dichotomy conveniently allows the epilepsy classification system to be presented in a simple and clear manner (see the Table below).
Table. Classification of the Epilepsies (Adapted from Tich and Pereon, 1999 [2] ) (Open Table in a new window)
|
Generalized |
Localization-related |
Idiopathic (genetic) |
Childhood absence epilepsy Juvenile absence epilepsy Juvenile myoclonic epilepsy Epilepsy with grand-mal seizures on awakening Other idiopathic generalized epilepsies |
Benign focal epilepsy of childhood (2 types) ADNFLE* Primary reading epilepsy |
Symptomatic or unknown |
West syndrome Lennox-Gastaut syndrome Other symptomatic generalized epilepsies |
Mesiotemporal lobe epilepsy Neocortical focal epilepsy |
*ADNFLE - Autosomal dominant nocturnal frontal lobe epilepsy |
||
The term idiopathic was often misunderstood in this setting, and the term "genetic is more informative." Whereas the term idiopathic in medicine usually means “of unknown cause,” idiopathic epilepsies are not truly of unknown cause; this confusing terminology will most likely be corrected in the upcoming International League Against Epilepsy (ILAE) classification system. [3]
In epilepsy, idiopathic seizures are genetically determined and have no apparent structural cause, with seizures as the only manifestation of the condition. Findings of the neurologic examination and neuroimaging studies are normal, and electroencephalographic (EEG) findings also are normal, aside from the epileptiform abnormalities. In some syndromes, the genetic substrate has even been identified. Most idiopathic epilepsies are generalized, but a few genetic epilepsies are focal.
Nonidiopathic epilepsies, by definition, are not genetic (though some may be associated with a minor genetic predisposition) but are the result of a brain insult or lesion. If the damage is focal, it results in a localization-related epilepsy; if it is diffuse, it results in a generalized epilepsy.
The term cryptogenic was abandoned and replaced by unknown cause.
This review discusses EEG findings in the generalized epilepsies. [4, 5, 6] Go to Epilepsy and Seizures for an overview of this topic.
For patient education resources, see the Brain and Nervous System Center.
Types of Waveforms Associated With Generalized Epilepsies
Spikes and sharp waves
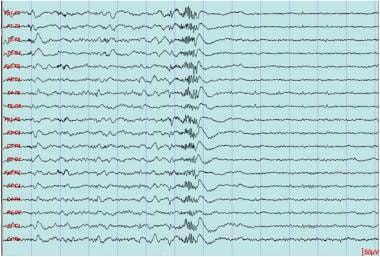
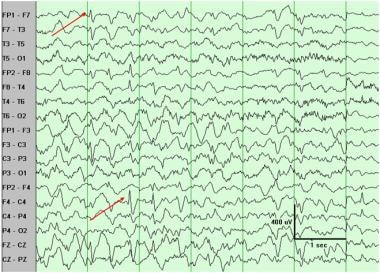
Spikes and sharp waves are sharp transients that have a strong association with epilepsy. They can be distinguished by their duration (spikes, < 70 ms; sharp waves, 70–200 ms) but have essentially the same clinical significance. Several characteristics distinguish these from benign epileptiform variants, including a high amplitude, which makes them stand out from ongoing background activity, and aftergoing slow waves, which give the appearance of disrupting or disturbing background activity (see the images below).
 Spike, generalized. Significant spikes usually are followed by a slow wave, as shown here. This example also illustrates that generalized spikes are typically maximal frontally. This is typical of primary (ie, idiopathic, genetic) epilepsies. If burst lasted 3 seconds or more, it could be classified as spike-wave complexes.
Spike, generalized. Significant spikes usually are followed by a slow wave, as shown here. This example also illustrates that generalized spikes are typically maximal frontally. This is typical of primary (ie, idiopathic, genetic) epilepsies. If burst lasted 3 seconds or more, it could be classified as spike-wave complexes.
Spike-wave complexes
Spike-wave complexes (SWCs) are the repetitive occurrence of a spike followed by a slow wave. Since any significant spike or sharp wave usually is followed by a slow wave (see above), a run of 3 seconds is required to classify a record as SWC, as opposed to the categories already mentioned (spike or sharp wave). SWCs can be divided further into 2 more specific types: 3-Hz SWCs and slow SWCs.
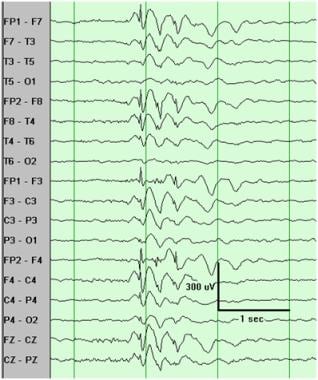
The 3-Hz SWC pattern is characterized by a frequency of 2.5–4 Hz and a very monomorphic (perfectly regular) morphology. It occurs in very discrete bursts, and between bursts the EEG is normal (see the image below).
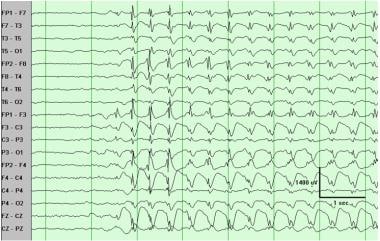
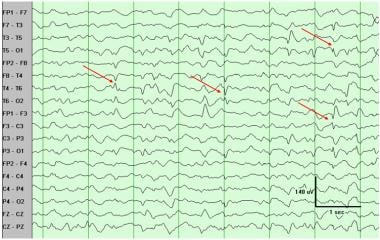 Sharp waves, multifocal. Sharp waves are seen at T4, T6, T5, and F3 on this 9-second segment. With other findings, this often is seen in generalized epilepsies of Lennox-Gastaut type.
Sharp waves, multifocal. Sharp waves are seen at T4, T6, T5, and F3 on this 9-second segment. With other findings, this often is seen in generalized epilepsies of Lennox-Gastaut type.
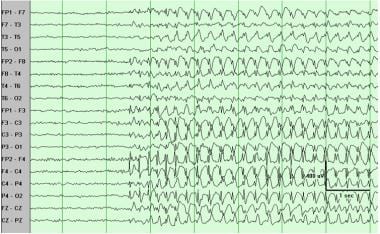
Slow SWCs are not only slower than 3-Hz SWCs (< 2.5 Hz) but also more irregular—that is, less monomorphic (see the images below). Bursts are less discrete than with 3-Hz SWCs, and between bursts, other abnormalities are seen in generalized epilepsies of the Lennox-Gastaut type.
 Slow spike-wave complexes. In addition to being slower, they are also less monomorphic than 3-Hz spike-wave complexes. With other findings, this often is seen in generalized epilepsies of Lennox-Gastaut type.
Slow spike-wave complexes. In addition to being slower, they are also less monomorphic than 3-Hz spike-wave complexes. With other findings, this often is seen in generalized epilepsies of Lennox-Gastaut type.
 Slow spike-wave complexes. In addition to being slower, they are also less monomorphic than 3-Hz spike-wave complexes. With other findings, this often is seen in generalized epilepsies of Lennox-Gastaut type.
Slow spike-wave complexes. In addition to being slower, they are also less monomorphic than 3-Hz spike-wave complexes. With other findings, this often is seen in generalized epilepsies of Lennox-Gastaut type.
Generalized epileptiform discharges (ie, spikes, sharp waves, SWCs) are usually maximal in the frontal regions, with typical phase reversals at the F3 and F4 electrodes (see the image below).
 Generalized 3-Hz spike-wave complexes (SWCs). This pattern is very monomorphic, with maximum (shown here by phase reversal) frontally, typically at F3/F4. This is typical of idiopathic (ie, genetic) generalized epilepsies, such as absence epilepsy. 3-Hz SWC is often faster at onset (4-5 Hz), as shown here.
Generalized 3-Hz spike-wave complexes (SWCs). This pattern is very monomorphic, with maximum (shown here by phase reversal) frontally, typically at F3/F4. This is typical of idiopathic (ie, genetic) generalized epilepsies, such as absence epilepsy. 3-Hz SWC is often faster at onset (4-5 Hz), as shown here.
Polyspikes
Polyspikes are multiple repetitive spikes occurring at about 20 Hz (see the image below). They are associated with idiopathic generalized epilepsies, most typically juvenile myoclonic epilepsy.
 Polyspikes, generalized. Note aftergoing slow wave. This is associated with idiopathic (genetic) generalized epilepsies, most typically juvenile myoclonic epilepsy.
Polyspikes, generalized. Note aftergoing slow wave. This is associated with idiopathic (genetic) generalized epilepsies, most typically juvenile myoclonic epilepsy.
Hypsarrhythmia
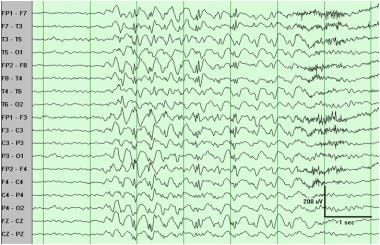
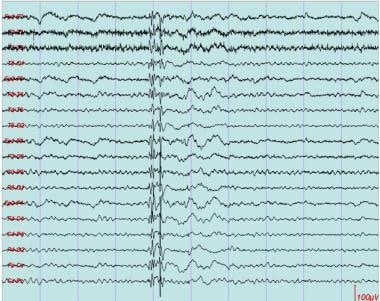
Hypsarrhythmia is defined as continuous (during wakefulness), high-amplitude (>200 μV), generalized polymorphic slowing with no organized background and multifocal spikes (see the images below). [7] It is commonly associated with West syndrome.
 Hypsarrhythmia. High-amplitude slowing with no organized background and multifocal spikes (left and right frontal in this sample). This is phenotype of first year of life and is associated with West syndrome (ie, infantile spasms).
Hypsarrhythmia. High-amplitude slowing with no organized background and multifocal spikes (left and right frontal in this sample). This is phenotype of first year of life and is associated with West syndrome (ie, infantile spasms).
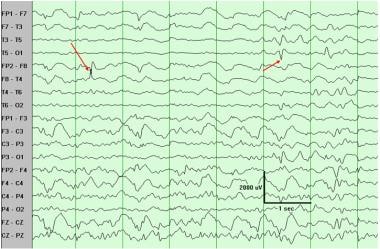 Hypsarrhythmia. High-amplitude slowing (note scale) with no organized background and multifocal spikes (right frontal and left occipital in this sample). This is phenotype of first year of life and is associated with West syndrome (ie, infantile spasms).
Hypsarrhythmia. High-amplitude slowing (note scale) with no organized background and multifocal spikes (right frontal and left occipital in this sample). This is phenotype of first year of life and is associated with West syndrome (ie, infantile spasms).
Electrographic seizure patterns
Generalized paroxysmal fast activity (GPFA) consists of bursts of fast (10 Hz) activity and typically is associated with tonic seizures. [8] Electrodecrement consists of abrupt attenuation (flattening) of background activity, often preceded by a high-amplitude transient (see the image below). This typically is associated with infantile spasms or atonic seizures, but can also be asymptomatic and thus considered interictal discharges. Also note that GPFA qualifies as Brief Ictal Rhythmic Discharges (BIRDS), according to the 2020 American Clinical Neurophysiology Society (ACNS) terminology. [9]
Clinical Presentation
Idiopathic (genetic) generalized epilepsies
Idiopathic generalized epilepsies, formerly called primary generalized epilepsies, are the best-known group of idiopathic epilepsies. [10, 11] They epitomize the meaning of the term “idiopathic”: genetic basis, normal neurologic examination findings, and normal intelligence.
Electroencephalography (EEG) shows generalized epileptiform discharges and may show photosensitivity. Seizure types include generalized tonic-clonic (GTC), absence, and myoclonic. Accordingly, EEG typically shows generalized spikes or sharp waves, 3-Hz or faster spike-wave complexes (SWCs; clinically associated with absence seizures), and polyspikes (clinically associated with myoclonic seizures). The EEG is normal (ie, no abnormal slowing) except for the epileptiform abnormalities.
Within the group of idiopathic generalized epilepsies, distinct entities are distinguished, primarily on the basis of predominant seizure type(s) and age of onset. Some syndromes are very well individualized, whereas others have less clear boundaries. [12, 13] The major and well-defined types of idiopathic generalized epilepsies include childhood absence epilepsy, [14, 15, 16, 17] juvenile myoclonic epilepsy, [18, 19, 20] and epilepsy with grand mal seizures (sometimes referred to as grand mal on awakening).
Symptomatic (or of unknown cause) generalized epilepsies
Symptomatic or generalized epilepsies are associated with diffuse brain dysfunction. The cause may be known (symptomatic), such as anoxic birth injury or a metabolic or chromosomal defect, or it may be unknown.
Accordingly, clinical evidence of diffuse brain dysfunction is usually present, either intellectual (eg, developmental delay or intellectual disability) or motor (eg, developmental delay or cerebral palsy). Similarly, the EEG shows evidence of diffuse brain dysfunction in addition to the epileptiform abnormalities, in the form of slowing. The clinical and EEG manifestations are not specific as to etiology; they vary tremendously with age and thus are said to be age dependent.
West syndrome is the phenotype of symptomatic generalized epilepsy in the first year of life and is characterized by infantile spasms, hypsarrhythmia, and developmental delay. [21] It is an age-specific response of the immature brain to a nonspecific focal or generalized insult. The age of onset peaks between 3 and 7 months.
Lennox-Gastaut syndrome (LGS) has an early childhood onset (age, 1–8 y) and consists of multiple seizure types, intellectual disability, and typical EEG findings dominated by generalized slow SWCs. [22] Seizure types include atypical absences, tonic, atonic, myoclonic, and GTC seizures. The atonic, myoclonic, tonic, and GTC seizures of LGS frequently result in unprotected falls (referred to as “drop attacks”) with injury.
Besides the classic EEG pattern of generalized slow SWC, other frequent but less specific EEG findings include background slowing, generalized slowing, and multifocal spikes. During sleep, the EEG may show polyspikes and slow waves. Another typical feature of LGS is generalized paroxysmal fast (> 10 Hz) activity (GPFA) during sleep. Many patients with symptomatic generalized epilepsy do not meet all the criteria for LGS.
-
Spike, generalized. Note high amplitude and aftergoing background suppression and slow wave.
-
Spike, generalized. Significant spikes usually are followed by a slow wave, as shown here. This example also illustrates that generalized spikes are typically maximal frontally. This is typical of primary (ie, idiopathic, genetic) epilepsies. If burst lasted 3 seconds or more, it could be classified as spike-wave complexes.
-
Sharp waves, multifocal. Sharp waves are seen at T4, T6, T5, and F3 on this 9-second segment. With other findings, this often is seen in generalized epilepsies of Lennox-Gastaut type.
-
Slow spike-wave complexes. In addition to being slower, they are also less monomorphic than 3-Hz spike-wave complexes. With other findings, this often is seen in generalized epilepsies of Lennox-Gastaut type.
-
Slow spike-wave complexes. In addition to being slower, they are also less monomorphic than 3-Hz spike-wave complexes. With other findings, this often is seen in generalized epilepsies of Lennox-Gastaut type.
-
Polyspikes, generalized. Note aftergoing slow wave. This is associated with idiopathic (genetic) generalized epilepsies, most typically juvenile myoclonic epilepsy.
-
Generalized 3-Hz spike-wave complexes (SWCs). This pattern is very monomorphic, with maximum (shown here by phase reversal) frontally, typically at F3/F4. This is typical of idiopathic (ie, genetic) generalized epilepsies, such as absence epilepsy. 3-Hz SWC is often faster at onset (4-5 Hz), as shown here.
-
Hypsarrhythmia. High-amplitude slowing with no organized background and multifocal spikes (left and right frontal in this sample). This is phenotype of first year of life and is associated with West syndrome (ie, infantile spasms).
-
Hypsarrhythmia. High-amplitude slowing (note scale) with no organized background and multifocal spikes (right frontal and left occipital in this sample). This is phenotype of first year of life and is associated with West syndrome (ie, infantile spasms).
-
Generalized paroxysmal fast activity and electrodecrement. This pattern is characteristic of generalized epilepsies of Lennox-Gastaut type and may be subclinical or associated with tonic or atonic seizures.