Overview
Vertebroplasty is an image-guided therapy in which a cement, a fast-setting polymer, is injected into a pathologic vertebral body. The purpose of this procedure is to relieve pain and disability. It can be used in the setting of painful osteoporotic compression fractures, pathologic fractures from underlying neoplasms, or structurally compromised vertebrae. It has been used for osteoporotic or malignant fractures. The procedure was first described by Galibert et al [1] who found that the “internal casting” provided by polymethyl methacrylate (PMMA) injected into a symptomatic vertebral hemangioma provided substantial pain relief.
With clinical experience and landmark innovation, other indications have emerged. Vertebroplasty can increase patient mobility, decrease narcotic needs, prevent further vertebral collapse resulting in altered forces on intervertebral discs, and avoid the complications associated with prolonged immobility.
Percutaneous vertebroplasty (PVP) usually involves percutaneous injection of PMMA into the vertebral bodies. Occasionally, PMMA has also been placed manually into vertebral lesions during open surgical operations.
Kyphoplasty is often mentioned alongside vertebroplasty. Kyphoplasty differs from vertebroplasty by adding an important additional step: insertion and inflation of a balloon before cement delivery, which also serves to restore vertebral body height and spine alignment. [2] Kyphoplasty is often used interchangeably with vertebroplasty and is considered a subset of vertebroplasty. Spine jack is a new system that corrects vertebral height, reduces the incidence of endplate damage by inserting an implant that mechanically augments the height of the vertebral body to better restore alignment followed by injection of cement.
Relevant anatomy
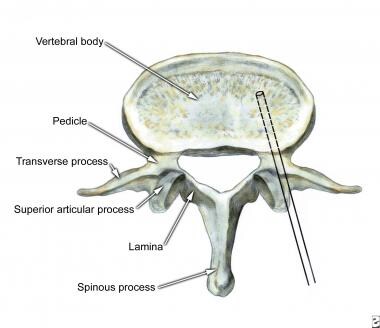
A normal thoracic spine is immobile and consists of 12 vertebrae. There are important anatomic landmarks to consider including a body, pedicles, laminae, spinous processes, and facet joints. Importantly, thoracic vertebrae have prominent lateral processes that form the articulation with the paired 12 ribs on either side. The 12 vertebrae, 24 ribs, and sternum together form the chest cavity, allowing negative-pressure respiration and providing protection of the chest wall.
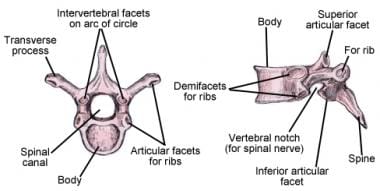 Illustration of thoracic vertebrae showing vertebral body, pedicles, facets, transverse process, rib joints, spinous process, and lamina.
Illustration of thoracic vertebrae showing vertebral body, pedicles, facets, transverse process, rib joints, spinous process, and lamina.
The lumbar spine is the next segment of the spine and is more mobile than the thoracic. The lumbar spine typically consists of 5 large vertebrae and important landmarks, including the body, pedicles, lamina, spinous processes, facet joints, and lateral processes. The lumbar spine is mobile with all articulations, contributing to flexion-extension, bending, and rotation allowing for truncal mobility.
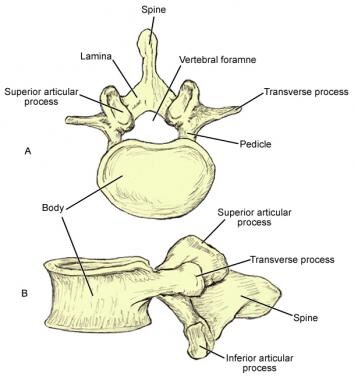 Lumbar vertebrae are characterized by massive bodies and robust spinous and transverse processes. Their articular facets are oriented somewhat parasagittally, which is thought to contribute the large range of anteroposterior bending possible between lumbar vertebrae. Lumbar vertebrae also contain small mammillary and accessory processes on their bodies. These bony protuberances are sites of attachment of deep lumbosacral muscles.
Lumbar vertebrae are characterized by massive bodies and robust spinous and transverse processes. Their articular facets are oriented somewhat parasagittally, which is thought to contribute the large range of anteroposterior bending possible between lumbar vertebrae. Lumbar vertebrae also contain small mammillary and accessory processes on their bodies. These bony protuberances are sites of attachment of deep lumbosacral muscles.
This anatomy is important to consider in three-dimensional space and be easily identifiable on X-rays in order to facilitate optimal placement of the needle under fluoroscopic guidance. An important step in understanding these procedures is to have a grasp of radiographic anatomy. (See Technique.)
Indications
Indications for percutaneous vertebroplasty include painful, non-healing osteoporotic or neoplastic vertebral compression fractures refractory to medical therapy. When these conditions result in loss of normal vertebral body height, balloon kyphoplasty or vertebral augmentation with implants such as Stryker’s SpineJack system can be utilized in order restore normal vertebral alignment while also treating pain.
For patients that may not be candidates for vertebroplasty (see Contraindications) or choose to not pursue invasive treatment, medical management options are available. Medical treatment of compression fractures consists of bed rest, pain control with non-steroidal anti-inflammatory medications, calcitonin, narcotics, and external bracing. Patients whose compression fractures fail to heal after completion of the aforementioned conservative regimen over a course of 3–6 weeks should be considered for vertebroplasty.
Patients without fractures but pain resulting from lytic metastatic neoplasm or rare symptomatic hemangioma are also candidates for vertebroplasty.
Vertebroplasty can also be performed prophylactically to stabilize a weakened vertebra before a planned surgery.
Osteoporotic vertebral fracture
One of the most common complications of osteoporosis is vertebral fracture that can occur spontaneously or more frequently as a result of minor trauma. In the United States, the incidence of compression fractures is more than 500,000 patients per year with a 16% lifetime risk in women and 5% lifetime risk in men. [4]
These vertebral fractures are often highly painful and can lead to pain-limited immobility, which leads to demineralization and propagation of a vicious cycle of continued demineralization and increased predisposition to fracture. Although the initial symptoms tend to disappear in 4–6 weeks, in many cases some patients have severe, persistent, incapacitating pain despite medical therapy. Consequences of untreated fracture include reduced height, reduction of normal thoracic kyphosis, and chronic back pain.
An important consideration in the discussion of vertebroplasty is the VERTOS study, which directly compared vertebroplasty to medical management. The VERTOS study prospectively compared osteoporotic compression fracture treatment of 18 patients with vertebroplasty to 16 patients with optimal medical management and found improvement in pain relief for the vertebroplasty group. [7] These results were confirmed with the VERTOS II study, a larger prospective randomized trial consisting of 101 patients treated with vertebroplasty and 101 treated with conservative management). [8, 9]
Two important studies to consider are those by Buchbinder et al. and Kallmes et al., each of which compared vertebroplasty to sham procedures and importantly demonstrated no significant improvement with vertebroplasty. [10, 11] This mixed evidence has sparked considerable debate as to the appropriate role of this procedure.
The VERTOS IV study, a randomized control trial published in four community hospitals in the Netherlands, looked at 180 patients comparing vertebroplasty vs sham procedure and did not show any statistically significant greater pain relief than sham procedure during 12 month follow up in patients with osteoporotic compression fractures. [12]
Titanium-implantable vertebral augmentation devices versus vertebroplasty or kyphoplasty
Even after balloon kyphoplasty, osteoporotic compression fractures have a high rate of continued collapse with subsequent loss of height and the development of angulation and deformity. This appears to increase the risk for adjacent level fractures. The SpineJack system (Stryker Corp, Kalamazoo, MI) consists of bilateral expandable titanium implants supplemented with bone cement. This system provides more symmetric and balanced lateral and anterior support, and requires lower volumes of bone cement compared to balloon kyphoplasty. Using this system, clinicians can now achieve better pain control, restore vertebral body height, restore spinal alignment, and reduce the risk of adjacent level fractures.
One important advantage of SpineJack kyphoplasty over standard balloon kyphoplasty or vertebroplasty is the ability to perform kyphoplasty safely in patients with mild–moderate retropulsion of the posterior endplate without neurological compromise. In certain situations, the SpineJack device has been used to elevate the fractured endplates serving to reduce the retropulsed bone fragment. In circumstances where patients have a retropulsed bone fragment, SpineJack is superior for the aforementioned reason. Retropulsed bone fragments are a relative contraindication to balloon kyphoplasty.
This finding was noted in the SAKOS study, which directly compared SpineJack kyphoplasty versus balloon kyphoplasty and showed that SpineJack patients had better pain reduction at 1 month and 6 months post treatment. The SAKOS study also showed that SpineJack is associated with a reduced incidence of adjacent level fractures. [13]
See Technique for further detail.
Spinal tumors
The role of vertebroplasty in spinal tumors is palliative. Generally, in previously untreated painful vertebral metastasis, radiotherapy is used in 70% of cases to alleviate spinal pain. However, this effect is delayed and often can take up to 2–6 weeks to provide relief. Vertebroplasty can achieve the same goal of pain relief with an almost immediate analgesic effect. [14]
Vertebral hemangioma
Vertebroplasty has successfully treated severe focal spinal pain with radiologically unaggressive vertebral (body) hemangioma as originally described by Galibert in 1984.
Contraindications
Absolute contraindications: [15]
-
Fractures that are asymptomatic
-
Active osteomyelitis of the target vertebra
-
Coagulopathy that is not amenable to correction
-
Allergy to cement or opacifying agent used in procedure
-
Fractures that cause compromise of the spinal canal and subsequent myelopathy or radiculopathy
Relative contraindications: [15]
-
Significant central canal narrowing from retropulsion of bony fragment or epidural tumor
-
Ongoing systemic infection
-
Disruption of the posterior cortex of the vertebral body
Technique
Equipment
Multiple vertebroplasty kits are available. Each manufacturer has their own specific subsets with unique names for the devices, but the basic components are the same: access needle, syringe, cement, and cement mixing apparatus. See individual manufacturers’ guidelines for further information on individual kits.
Preprocedure patient evaluation
The most important aspect of planning this procedure is an accurate history and physical exam. It has been shown that localizing tenderness on palpation is not associated with superior vertebroplasty response. [16]
Important information can be obtained from a good history taken on a patient with an acute vertebral compression fracture.
-
deep pain with sudden onset
-
midline location
-
exacerbation by motion and standing
Imaging
Studies to consider in the evaluation of patients for vertebroplasty include plain film X-ray, CT scan, and MRI of the spine. These three modalities will help determine which vertebra is to be injected.
MRI will allow for evaluation of canal narrowing or osteomyelitis. CT will allow for evaluation of lytic or blastic bone lesion and plain films can be useful for procedural planning.
Obtaining informed consent and a thorough discussion of the risks, benefits, and alternatives is an important aspect of any procedure.
Setup and positioning
Procedure time can vary but ultimately lasts anywhere from 40 to 120 minutes.
-
Conscious sedation and local anesthesia are used in the majority of cases. Use of MAC anesthesia has also been described.
-
Prophylactic antibiotics such as cefazolinshould be considered.
-
Place the patient in the prone position.
-
Align posterior ribs to obtain a good lateral view.
-
On the anteroposterior (AP) view, find the obliquity that projects the pedicle over the upper outer third of the vertebral body. Mark this point.
Radiation exposure
Radiation exposure is an important consideration when performing these procedures. In a study analyzing 11 cases of vertebroplasty, patient effective doses were estimated at 34mGy with average fluoroscopy times of 28 minutes (in comparison, a typical CT abdomen and pelvis effective dose is 8–14 mGy). Operator exposures were highest to the hands and chest, although there was a decrease in occupational dose by 76% with the use of mobile shielding. It was estimated that an operator could perform 150 procedures annually before exceeding annual dose constraints. [17]
Needle placement
Lidocaine with epinephrine is commonly used for local anesthetic and a spinal needle to anesthetize the periosteum. Proper trajectory may be confirmed with AP and lateral fluoroscopic views. Depending on the size of the pedicle, different gauge needles can be used. 11-gauge is recommended for lumbar and lower thoracic pedicles; but a 13-gauge will suffice midthoracic pedicles.
A large clamp will allow for maintenance of tension along the back to allow for easier placement of the needle. A sterile hammer can be used to gently tap the needle. Direct the needle into the vertebral body, using AP and lateral views for verification.
 Percutaneous vertebroplasty, transpedicular approach under fluoroscopic guidance, anteroposterior view.
Percutaneous vertebroplasty, transpedicular approach under fluoroscopic guidance, anteroposterior view.
Transpedicular approaches:
-
For a unipedicular approach, advance needle into the anterior third of the central vertebral body.
-
For a bipedicular approach, advance needles into the midportion of the hemivertebrae.
-
A parapedicular approach may be considered as well.
Polymethylmethacrylate mixing and injection procedure
Depending on the manufacturer, there can be different methods to make the cement. Depending on the agent of choice, both polymethylmethacrylate (PMMA) and barium sulfate (opacifying agent) should be made as per the manufacturer's instructions. Slowly inject this mixture until the vertebral body is well filled, making certain to stop before PMMA leaks posteriorly into the epidural area or significantly fills a vein.
An important consideration is the volume of cement used to fill the vertebral body. Pain relief is not associated with cement volume, thus attempting to fill the vertebral body as completely as possible is not necessary. [19]
Stryker SpineJack System
One of the shortcomings of percutaneous vertebroplasty and even balloon kyphoplasty is a continued rate of collapse. Osteoporotic compression fractures have a high rate of continued collapse with subsequent loss of height and the development of angulation and deformity after these procedures, which increases the risk for adjacent level fractures. The SpineJack system (Stryker Corp, Kalamazoo, MI) consists of bilateral expandable titanium implants supplemented with bone cement. This system provides more symmetric and balanced lateral and anterior support, and requires lower volumes of bone cement compared to balloon kyphoplasty. Using this system, clinicians can now achieve better pain control, restore vertebral body height, restore spinal alignment, and reduce the risk of adjacent level fractures. [20]
The SpineJack system offers three implant kit sizes: 4.2 mm, 5.0 mm, and 5.8 mm. Each kit contains the appropriate instrumentation for the procedure, first for preparation, then for expansion and fracture reduction. The range of sizes accommodates various anatomies and fracture types. The implant expands in a craniocaudal direction and combat compression forces up to 1000N of expansion force.
A pedicle width of 0.8 mm larger than the desired implant size is recommended for safe placement. (e.g. 4.2 mm implant +0.8mm = 5mm minimum pedicle width).
Table. (Open Table in a new window)
| Pedicle diameter | Recommended kit |
|---|---|
| 5.0–5.8 mm | 4.2 mm |
| 5.8–6.6 mm | 5.0 mm |
| 6.6 mm or greater | 5.8 mm |
Like a vertebroplasty, the Stryker SpineJack system utilizes a bipedicular approach to advance the access cannula to the posterior one third of the vertebral body. Then a guidewire is advanced to the midpoint of the vertebral body, then removal of the access cannula. Then following the path of the guidewire, the reamer is advanced until it is entirely within the vertebral body. Then the template is inserted to clean the implant site and verify the length of the implant. Then the spine jacks are expanded to reduce the fracture and restore anatomy. Then PMMA is advanced and good closure is obtained with adequate hemostasis.
Postprocedural care
Generally, patients are kept on bed rest for 1–2 hours and given analgesics for postoperative pain with muscle relaxants for spasm. Patients with osteoporosis should be managed medically and closely followed after the procedure. Without systemic osteoporosis therapy, 20% of patients with a fracture develop a second fracture.
Treatment for osteoporosis includes DEXA scans, lifestyle modifications (smoking cessation, alcohol moderation, exercise), dietary supplementation (calcium, vitamin D), and medical management (antiresorptive). [22]
Complications
Complications with percutaneous vertebroplasty are more commonly seen with malignant spinal tumors and hemangiomas than with osteoporotic compression fractures. Chiras et al reported incidents and complications in 274 patients with 10% attributable to spinal tumor cases, 2–5% with vertebral hemangioma cases, and 1–3% seen in osteoporotic compression fractures. [23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43]
It is important to counsel patients on the possibility of the following:
-
Neurologic deficit including paralysis
-
Positioning or needle-placement related fractures including those of the vertebra, rib, or sternum
-
Infection
-
Allergic reaction
-
Pulmonary embolus
-
Hemorrhage
-
Pneumothorax or hemothorax
-
Cement migration
CT scan should be obtained in any patient who experiences new radicular pain post-procedure. CT scan is particularly useful in patients for which there is a concern for polymethylmethacrylate (PMMA) migration, specifically that into the epidural venous plexus.
CT scan is also useful for assessing patients with severe back pain to assess for a fractured pedicle or transverse process.
New onset regional back pain is suggestive of adjacent level fracture and can be better evaluated with non-contrast MRI. Careful review of the STIR sequence on non-contrasted MRI can help determine the acuity of the fracture.
CT pulmonary angiogram or rib series X-ray can be helpful in patients who develop chest pain in the post-procedure period in addition to a standard EKG. The CT pulmonary angiogram can rule out pulmonary embolus.
Paralysis has been reported but is very uncommon. Precautions should be taken while injecting above L1, with attention to the posterior vertebral body wall; do not allow PMMA to flow into the epidural venous plexus.
Reports are mixed as to whether vertebroplasty predisposes patients to develop additional vertebral fractures. Spine Jack has been shown to have reduced incidence of adjacent level fracture when compared to vertebroplasty or balloon kyphoplasty.
Questions & Answers
Overview
What is percutaneous vertebroplasty (PVP)?
What is the difference between kyphoplasty and percutaneous vertebroplasty (PVP)?
Which anatomy is relevant to percutaneous vertebroplasty (PVP)?
When is percutaneous vertebroplasty (PVP) indicated?
What is the role of percutaneous vertebroplasty (PVP) in the treatment of spinal tumors?
What is the role of percutaneous vertebroplasty (PVP) in the treatment of vertebral hemangioma?
What are the contraindications for percutaneous vertebroplasty (PVP)?
What equipment is needed to perform percutaneous vertebroplasty (PVP)?
What is the role of imaging in the preprocedure evaluation for percutaneous vertebroplasty (PVP)?
How is the patient prepped and positioned for percutaneous vertebroplasty (PVP)?
What is the radiation exposure of percutaneous vertebroplasty (PVP)?
What is the approach to needle placement for percutaneous vertebroplasty (PVP)?
What method is used to make the cement in percutaneous vertebroplasty (PVP)?
How is the Stryker SpineJack system utilized?
What is included in postprocedural care following percutaneous vertebroplasty (PVP)?
What are the possible complications of percutaneous vertebroplasty (PVP)?
-
Materials and devices for percutaneous vertebroplasty - Needle (11G, 6" [DBMNJ1106]); polymethylmethacrylate (PMMA) cement (Howmedica Simplex Codman Cranioplastic Kit); barium (opacifying agent, sterile barium sulfate, 6-g packets); syringes (1-cc Luer-Lok syringes).
-
Percutaneous vertebroplasty, transpedicular approach.
-
Percutaneous vertebroplasty, transpedicular approach under fluoroscopic guidance, lateral view.
-
Percutaneous vertebroplasty, transpedicular approach under fluoroscopic guidance, anteroposterior view.
-
Illustration of thoracic vertebrae showing vertebral body, pedicles, facets, transverse process, rib joints, spinous process, and lamina.
-
Lumbar vertebrae are characterized by massive bodies and robust spinous and transverse processes. Their articular facets are oriented somewhat parasagittally, which is thought to contribute the large range of anteroposterior bending possible between lumbar vertebrae. Lumbar vertebrae also contain small mammillary and accessory processes on their bodies. These bony protuberances are sites of attachment of deep lumbosacral muscles.