Overview
Management of voiding dysfunction in neurologic disorders can substantially improve not only patients’ health but also their quality of life. A systematic review of the pattern of voiding dysfunction leads to an understanding of the underlying mechanism, which, in turn, allows the treating physician to develop a strategy for managing it. [1] Neurourology, although a relatively new field of study, has revolutionized the management of a vexing problem that affects millions of patients.
Neuroanatomy of Pelvic Floor
The striated muscle forming the urethral rhabdosphincter and the periurethral striated muscle (part of the pelvic diaphragm) together make up the external urethral sphincter mechanism in humans. In women, the rhabdosphincter forms a 1.5-cm long circular ring around the middle third of the urethra, extending cranially as far as the posterior bladder base. [2] In men, the rhabdosphincter has 3 sections extending over a greater length of urethra. On cystoscopy, this striated muscle can be seen to contract with electrical stimulation of the pudendal nerve.
Spinal cord nuclei supplying the vesicourethral smooth muscle and rhabdosphincter are in the lumbosacral region. The sympathetic autonomic nucleus is in the anteromediolateral gray matter at T10-T12, and the parasympathetic nucleus is at S2-S4. Motor neurons of the urethral rhabdosphincter are in the nucleus of Onufrowicz (Onuf) in the sacral ventral horns. The neurons are smaller, more spherical, and more closely packed than other anterior horn cells.
The nucleus of Onuf and the sacral parasympathetic nucleus are at slightly different levels. This can be of clinical significance in lesions of the conus. The neurons of the Onuf nucleus are relatively spared in many neuromuscular disorders.
The somatomotor supply to the rhabdosphincter is via the pudendal nerves. This has been documented by direct stimulation studies and in horseradish peroxidase tracings; however, some studies have shown contributions from some branches of the pelvic plexus. The role of these branches is in question; an autonomic function has been postulated.
In dogs, complete silence of the rhabdosphincter is seen only if the pudendal and pelvic efferents are sectioned. The Onuf nucleus shows changes after injection of horseradish peroxidase into either the pudendal or the pelvic nerve. Some evidence suggests that the rhabdosphincter in cats has triple innervation, with cholinergic, adrenergic, possibly copeptidergic, and traditional motor endplates.
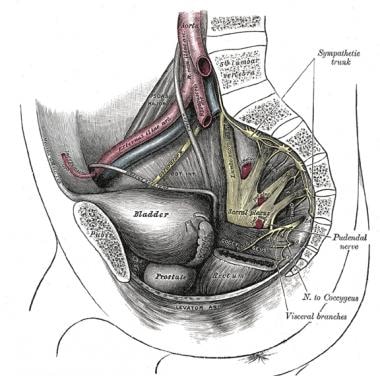
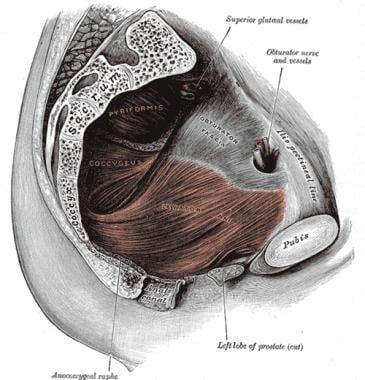
The pudendal nerve leaves the pelvis through the lower part of the greater sciatic notch beneath the lower border of the piriformis (see the images below). It bifurcates just before the sacrospinal ligament, with one branch going to the anal sphincter and the other to the urethral sphincter. Studies on children with meningomyelocele have suggested that different sacral levels supply the 2 sphincters, so that absence of activity in one is not invariably accompanied by a deficit in the other.
Neurophysiology of Pelvic Floor
Sphincter electromyography
Electromyographic (EMG) recordings from the urethral and anal sphincters were first made in the 1930s by Beck, [3] who recorded from the anal sphincter using fine wires. Petersen and Franksson performed studies of the urethral sphincter in 1955. [4]
Since then, measurements of sphincter activity using conventional electrodes, wires, surface electrodes, and catheter-mounted electrodes have become an important part of the evaluation of patients with voiding dysfunction. [5] The procedure is not done routinely unless a neurologic abnormality is suspected as the cause of voiding dysfunction. Some indications would be voiding dysfunction after pelvic or spinal cord trauma and spinal stenosis potentially affecting the cauda equina or conus.
Occasionally, needle EMG may be used to evaluate pelvic pain syndromes. EMG is usually not performed in cases of stress urinary incontinence or cases in which a central nervous system (CNS) lesion is producing the incontinence.
Muscle fibers in the periurethral striated muscle are predominantly type Ia, the slow-twitch, fatigue-resistant fibers. The rhabdosphincter fibers are generally smaller than those of other striated muscle. No stretch receptors have been found in the striated muscle immediately related to the urethra. A curious property of the urethral sphincter is that it has a tonic firing pattern that silences only during voiding.
Positioning of electrodes for recording from the urethral sphincter is performed most easily with the patient in the lithotomy position. The periurethral tissue may be made analgesic with ethyl chloride spray or lidocaine ointment.
The electrode is inserted just lateral to the urethral meatus in women. Sphincter muscle is encountered at a depth of about 15 mm. In the male, the electrode is inserted in the perineum between the scrotum and the anal verge. It may be positioned by feeling for the prostate gland with a finger in the rectum and directing the electrode toward the apex of the gland. The EMG activity should be monitored with a speaker during the positioning.
In females, a 25-mm electrode is used; in adult males, a 75-mm electrode is necessary. If a shorter electrode is used, EMG activity in the more superficial bulbocavernosus muscle is recorded. Other techniques of needle insertion include placement under cystoscopic control and placement via a vaginal approach in women. Although some discomfort is associated with insertion, it is short-lived. Most patients tolerate the procedure if well prepared. The author prefers to use monopolar needle electrodes.
At rest, continuous baseline activity consists of motor unit potentials of 100-500 µV firing at rates of 1-4/sec. This activity is at its lowest when the patient’s bladder is empty. As the bladder fills, the firing rate increases slowly until bladder fullness is perceived. At that point, the type II fibers are contracted voluntarily in a graded way. When bladder capacity is reached, some voluntary units as large as 3 mV are seen.
The motor units of the sphincters are of shorter duration than those of skeletal muscles and resemble the units of facial muscles. Individual motor unit analysis using a delay line showed that 93% of the motor units in the sphincter are less than 6 msec in duration and less than 2 mV in amplitude. [6]
Generally, about 10-15% of units are polyphasic. The presence of fibrillations and positive sharp waves may be difficult to determine. If present, these potentials are best seen during voiding, when the sphincter motor units are silent. Fasciculation potentials are extremely difficult to appreciate when tonic muscles are active. Complex repetitive discharges are more common in the sphincters than in other striated muscles. Their presence has been associated with urinary retention in women [6] and enuresis in children. [7]
Reflex responses
Baseline electrical activity in the sphincters can be modified by a number of maneuvers. The Credé maneuver (ie, pressing on the bladder suprapubically), the Valsalva maneuver, and stimulation of perianal or perineal skin all can produce reflex activation of the sphincters. Manual stimulation of the clitoris or the glans penis produces an increase in activity referred to as the bulbocavernosus reflex. This response has been quantified by using electrical stimulation to trigger the oscilloscope sweep and to activate the reflex.
Rushworth, in 1967, was the first to observe an EMG response to electrical stimulation of the pudendal nerve. [8] Since then, this response has been reported by several groups. The pudendal nerve can be stimulated by using ring electrodes around the penis in men or a bipolar stimulating probe on the clitoris in women. The stimulus is usually a square wave pulse with a duration of 0.05-0.2 msec and an amplitude of up to 300 V. Sensory threshold in healthy adults is 60-80 V. Stimulation is carried out at twice the sensory threshold.
When stimulation is applied in this way, a complex EMG response is recorded from the external urethral sphincter, with clear-cut components appearing and increasing in duration with increasing voltage. The first component to appear, R1, has a latency as long as 45 msec and a duration of 10-30 msec. This component decreases in latency as the voltage increases. A second component, R2, may occur at 50-120 msec at higher stimulating voltages. Some observers are able to distinguish a third component at about 140 msec in patients with intact spinal cords.
The first component of the sacral reflex is thought to represent an oligosynaptic or monosynaptic response at the level of 1 sacral segment. [9] The second component may be polysynaptic and involve several sacral segments. The third component probably represents a nociceptive response mediated centrally.
Attempts have been made to measure conduction velocities in the sensory and motor nerves.
Chantraine determined motor conduction velocities in the pudendal nerve using a technique quite difficult to apply in conventional EMG. [10] Pudendal motor latency is easier to measure by stimulating the pudendal nerve with a finger-mounted electrode placed against the ischial spine rectally. The sacral roots may be stimulated magnetically or by placing needle electrodes in the foramina. Somatosensory evoked potentials may be obtained by stimulating the perineum or the bladder neck and recording cortically.
Yilmaz et al have described a dartos reflex that is a sympathetically mediated scrotal reflex similar to the more commonly used cremasteric reflex. This evaluates the integrity of the T12-L2 sympathetics and the genitofemoral nerve. [11]
Bladder and Pelvic Floor Function in Neuromuscular Disorders
Bladder and sphincter dysfunction are seldom seen, even in advanced neuromuscular disease. The sparing of cells in the Onuf nucleus appears to limit the loss of fibers in the external urethral sphincter and the pelvic floor in general. [12]
Sphincter muscle abnormalities can usually be explained by other factors. This was the case in a group of children with neuromuscular disorders studied by Dyro and Bauer: a child with myotonic dystrophy had no myotonic discharges in the sphincter. [13] They also studied 3 boys with Duchenne muscular dystrophy (DMD), 2 girls with congenital myopathy, a girl with Charcot-Marie-Tooth disease type II, and a boy with Kugelberg-Welander syndrome (KWS).
Motor units in the sphincter of 1 of the girls with congenital myopathy were of low amplitude; another had evidence of denervation after scoliosis surgery. [13] The boy with KWS had some increased-amplitude motor units and uninhibited detrusor contractions attributed to coexisting thoracolumbar syringomyelia. Two of the boys with DMD had detrusor-sphincter dyssynergia, but one had concomitant cerebral palsy and the other had a T10 paraplegia following scoliosis surgery.
Sporadic reports of pelvic floor involvement in neuromuscular disorders have been published, suggesting again that these abnormalities are the exception rather than the rule. Dixon et al reported a 48-year-old woman with limb-girdle muscular dystrophy who had had stress incontinence since the age of 12 years. [14] She was aged 33 years when she developed lower limb weakness and was diagnosed with dystrophy.
Results of EMG in the patient’s limbs were consistent with myopathy. [14] Although she was nulliparous, she had pelvic floor descent. The results of external urethral sphincter electromyography (EMG) were normal, and she had no detrusor hyperactivity. Biopsy of pelvic floor muscles showed combined hypertrophy and atrophy of fibers, with 40% containing 1 or more internal nuclei. Type I fibers predominated.
Bernstein et al studied 10 patients with myotonic dystrophy, with inconsistent results. [15] The investigators used surface electrodes to study the pelvic floor. Four of the patients were infrequent voiders, 1 had urge and stress incontinence, 2 had only urgency, 1 had urinary obstruction, and 2 had “normal” voiding. Sphincter EMG findings were reported as normal in the 9 patients who underwent the test.
In the anterior horn cell disorders—amyotrophic lateral sclerosis, KWS, and polio—little or no compromise of the sphincter is noted, and autopsy evidence indicates that the cells of the Onuf nucleus are spared.
Myasthenia gravis apparently has little effect on the sphincteric mechanism. Greene et al [16] and Wise et al [17] investigated patients with postprostatectomy incontinence and myasthenia gravis and found no influence on the cholinergic receptors of the detrusor by the myasthenia.
Christmas et al described a 59-year-old woman with a 35-year history of myasthenia who had difficulty voiding, a feeling of incomplete emptying, and frequency but whose symptoms improved when she increased her dose of pyridostigmine. [18] A urodynamic study showed normal bladder volume and normal sensation but poor detrusor contractions.
Neuropathies, in particular metabolic neuropathies (eg, those due to diabetes or uremia), do affect sphincter and pelvic floor function. This can be simply a denervation of the motor efferents to the sphincter and pelvic floor, or it can be a combined somatic and autonomic neuropathy. Measurement of the sacral reflex arcs of patients with diabetes or other neuropathies, including hereditary sensorimotor neuropathies, has shown denervation of the sphincters and prolongation of pudendal nerve latencies and latencies of the sacral reflex arc.
Urologic Symptoms of Neurodegenerative Disorders
The urologic manifestations of neurodegenerative disorders, including Parkinson disease (PD), [19, 20, 21] multisystem atrophy, and Huntington chorea, have been studied by several groups. [22, 23, 24, 25, 26]
Galloway, [22] Murnaghan, [23] Eardley et al, [24] and Mathers et al [25] studied the urethral and anal sphincters in addition to performing cystometrography in patients with PD. (About 90% of patients with late-stage PD have voiding dysfunction.) The patients all had detrusor hyperactivity or instability. The actual electromyographic (EMG) patterns were normal with no denervation, but a sphincteric “tremor” and failure to relax while voiding were noted.
Brusa et al showed that initiation of L-dopa therapy worsened bladder overactivity and reduced capacity, but long-term use improved sensation of bladder filling and capacity. [27]
Constipation is a common complaint in parkinsonism and is thought by some to be a result of autonomic dysfunction and lack of activity. Bowel biopsies have shown autonomic involvement, but a contributing factor may be a phenomenon observed by Mathers et al, [25] who reported paradoxical anal sphincter contraction during simulated defecation, with straining producing a sort of anismus obstruction.
These investigators also reported impaired relaxation of the external urethral sphincter and the presence of Lewy bodies in the colonic mesenteric plexus. [25] The degree of sphincteric involvement appears to be a function of autonomic involvement.
Patients with multisystem atrophy and autonomic failure have considerable difficulty with incontinence. Sphincter EMG of these patients has shown abnormal motor units and increased motor unit durations. Patients with multisystem atrophy and Shy-Drager syndrome are known to have cell loss in the motor nuclei at S2-S4; this finding has led to increased speculation concerning the autonomic properties of these neurons. [28]
Paviour et al reviewed 37 patients with multisystem atrophy who underwent sphincter EMG and concluded that the changes seen were not specific. [29]
Huntington chorea is a neurodegenerative disorder of autosomal-dominant inheritance characterized by progressive neuronal loss in the caudate nuclei, the basal ganglia, and the cortex. Wheeler et al studied 6 patients with Huntington chorea and incontinence; 2 had normal study results, and 4 had detrusor hyperreflexia but normal motor units in the sphincter. [30] “Choreiform” contractions of the pelvic floor muscles were noted during bladder filling but were suppressed by voiding contractions. The patients were not dyssynergic.
The incontinence in Huntington chorea and in other dementing illnesses is synergic loss of urine caused by the loss of central inhibitory pathways. Normal or near-normal sphincter activity is preserved in most disorders of muscle or anterior horn cells.
The findings of degenerative changes in the presence of autonomic dysfunction give some credence to speculations that the cells of the Onuf nucleus may be a sort of unique transitional neuron with autonomic properties. The myopathies, which mostly affect type II muscle fibers, are likely to have little effect on the type I fibers of the sphincters.
Cerebrovascular disease can result in voiding dysfunction, usually in the context of bilateral hemispheric lesions. During the acute phase, urinary retention is typical. Later, during recovery, symptoms such as frequency, urgency, urge incontinence, or inappropriate voiding are more common. The loss of frontal connections results in a pattern of bladder function resembling that seen in non–toilet-trained children. Incontinence is a common occurrence in normal pressure hydrocephalus, usually resolving after shunting.
Pontine lesions or lesions below the level of the pontine micturition center result in the loss of coordinated (synergic) voiding. Incontinence has been reported in bilateral putaminal lesions, [31] but the type of incontinence was not specified.
Children with cerebral palsy frequently have small bladder capacity and urge incontinence. Enuresis with uninhibited detrusor contractions or inappropriate relaxation of the sphincter with loss of small amounts of urine may be the presenting complaint in a child with very subtle cerebral palsy.
Spinal cord infarction is a serious complication of surgery on the thoracic aorta. Acute occlusion of the artery of Adamkiewicz by thrombus, embolus, or dissection of the aorta produces a devastating picture of paraparesis with loss of bladder function accompanied by denervation of the urethral and anal sphincters from involvement of the conus medullaris. The net result is a large, atonic, painless bladder that empties by overflow.
Urologic Symptoms of Multiple Sclerosis
Multiple sclerosis (MS) is a disorder that affects patients in many different ways, depending on the part of the neuraxis involved in the demyelinating process. About 10% of patients present with bladder or sexual symptoms, and 65-90% have genital involvement at some time in the course of their disease. These complaints may involve incontinence, urgency, retention, or impotence.
Electromyography (EMG) of the urethral sphincter seldom shows a significant abnormality. Eardley et al studied 24 patients and found only minor abnormalities (eg, abnormalities in central sensory and motor conduction) in 88%. [32]
Mathers et al studied 23 patients with MS and bladder or rectal dysfunction using cortical and lumbar transcutaneous electrical stimulation, pudendal nerve stimulation, single-fiber EMG, and manometry; they found central conduction times to be abnormal in 10 and absent in 8. [25] Peripheral conduction was decreased, and fiber density was increased in 3.
Mayo and Chetner studied 46 women and 43 men with MS aged 22-71 years and found that detrusor abnormalities were extremely common, with 63% failing to empty completely because of hypocontractile bladders and 6% with complete areflexia. [33]
Urologic Symptoms of Spinal Cord Disorders
Spinal cord lesions produce various types of voiding dysfunction, depending on the level of the neuraxis involved. Acute herniation of a central disk at L5-S1 is a neurosurgical emergency when the patient comes in with sudden onset of painful urinary retention. The nerve roots of the cauda equina that supply the detrusor travel medially. The sensory inputs from the bladder are not affected. In central herniation, patients usually experience no sciatic radiation of pain.
Spinal stenosis in the lumbosacral region, as it begins producing symptoms, usually results in intermittent episodes of urinary retention as a manifestation of intermittent claudication of the conus or cauda equina. Stenosis in the cervical region is more likely to produce long-tract involvement with bladder sphincter dyssynergia; that is, contraction of the bladder is accompanied by abnormal contraction of the sphincteric mechanism.
Spinal cord injury above the sacral segments but below the pontine micturition center results, in the acute phase, in a state of so-called spinal shock. The detrusor is areflexic and insensate. Sphincteric activity continues. The patient may retain a large volume of urine. An indwelling catheter is usually placed to avoid overdistention, which in itself can render the bladder unresponsive.
As spinal shock resolves and reflexes are regained, tapping over the bladder often elicits a bladder contraction. The coordinated voiding regulated by the pontine micturition center is lost because of the disconnection of pathways traveling through the area of spinal cord damage.
Dyssynergic voiding occurs and, if untreated, can result in very low bladder capacity with frequent contractions, poor emptying, high bladder pressures with trabecular formation, and eventually renal failure from hydroureter and hydronephrosis. [34] Before treatment strategies were developed for managing the bladder in spinal cord injury, renal failure was the most common cause of death.
The spinal dysraphisms often lead to voiding dysfunction, [35, 36] the nature of which depends on the spinal level of the abnormality. Meningomyelocele is now diagnosed in utero, and the infant, usually delivered by cesarean section, undergoes neurosurgery in the newborn period. Urodynamic studies and sphincter electromyography (EMG) done shortly after corrective surgery dictate management. With very low lesions, lower-extremity function may be normal while the sphincter is totally denervated. These children should simply wear diapers.
When the dysraphism affects supraspinal segments, the patient may experience inappropriate sphincter contraction with or without bladder contractions. In such patients, intermittent catheterization is instituted in the newborn nursery and continued at home. Repeat studies are done at the ages of 6 months and 1 year. Some children develop innervation of the sphincter and convert from voiding at low pressure to dyssynergic voiding. Management requires intermittent catheterization and usually anticholinergic drugs to reduce bladder contractions.
Late complications are seen during the adolescent growth spurt if tethering of the filum terminale occurs. Late deterioration of bladder function also may be seen in diastematomyelia. In both cases, traction on the conus can compromise voiding function.
Careful examination of the lower back may reveal a hair patch or a sacral dimple as evidence of underlying pathology. One of the author’s patients had no dysfunction until his spinal cord was compromised further by arthritic changes. He was 73 years old and had had no bowel or bladder dysfunction or lower-extremity dysfunction until that time.
Syringomyelia or hydromyelia can occur as a late complication of spinal cord injury or as a congenital lesion. Intramedullary spinal cord tumors, gliomas, or ependymomas are sometimes associated with the development of a syrinx. Because most patients who develop a posttraumatic syrinx have spastic, dyssynergic bladders as a result of their injury, little change is seen.
Syringes of other etiologies, in the author’s experience, seldom cause bowel or bladder dysfunction. Intramedullary cord tumors usually do not cause bladder dysfunction until they become large enough to cause compression of cord substance within the spinal canal.
Iatrogenic Voiding Dysfunction
Whereas a painless atonic neurogenic or motor paralytic bladder can be caused by peripheral neuropathy of diabetes or alcoholism, it can also be the result of trauma or pelvic surgery. In rare cases, pudendal nerves are injured after orthopedic surgery for femoral fractures. Amarenco et al reported 6 cases of pudendal nerve traction after orthopedic surgery in which bladder function was not involved, but the patients did experience genital sensory deficit and erectile dysfunction. [37]
A flaccid, unresponsive bladder can be seen in patients who are overmedicated with tricyclic antidepressants or antiparkinson medications or who have electrolyte imbalances.
Tricyclic antidepressants have anticholinergic properties and tend to decrease detrusor contractility. This property of drugs such as imipramine and amitriptyline has led to their being frequently used for the treatment of detrusor instability. When used in higher dose ranges or in patients with previously asymptomatic outlet obstruction, they may produce urinary retention.
The calcium channel blockers used in migraine or cardiovascular disorders also may produce urinary retention by decreasing bladder contractility. Some beta-adrenergic blockers can increase urethral pressure. Propranolol has been used therapeutically for this reason; however, in a hypertensive patient with prostatic enlargement, it may produce an unwanted increase in outlet resistance.
Pseudoephedrine and phenylpropanolamine (recalled from the US market), which are found in cough remedies, have a similar tendency to increase outlet resistance and may cause a man with benign prostatic hypertrophy (BPH) to retain urine. Alpha-blockers have been used to decrease outlet resistance in patients with BPH but may aggravate stress incontinence.
Donepezil, an anticholinesterase that is highly selective for the central nervous system, has been used for the treatment of cognitive impairment in patients with Alzheimer disease. Hashimoto et al have reported a 7% incidence of urinary incontinence in previously continent patients treated with donepezil. [38]
Galantamine also has incontinence and frequency as potential adverse effects. This is a concern because urinary incontinence in patients with dementia has a considerable effect on potential placement.
Concerns have been raised about using anticholinergic medications for detrusor overactivity and potentially worsening dementia in patients with mild cognitive dysfunction. [39, 40]
Incontinence or frequency of urination may be seen as a complication of pelvic irradiation. Radiation cystitis may be present during the course of the radiation or may appear as a late effect.
Medical Management of Voiding Dysfunction
Medical management of voiding dysfunction depends on the nature of the dysfunction. The 2 functions of the bladder-sphincter system are to store urine and then to release it appropriately. Impairment of either function may adversely affect voiding.
Failure to store
Urge incontinence is the involuntary loss of urine associated with a strong urge to void. [41] Motor urge incontinence is associated with increased contractibility of the detrusor during the filling phase. The patient experiences uninhibited bladder contractions that are perceived as an urgent need to void even at low bladder volumes.
These contractions may be associated with outflow obstruction (eg, benign prostatic hyperplasia [BPH]), inflammation (eg, urinary tract infection or radiation cystitis), or neurologic disorders, usually involving suprapontine lesions. Normally, small contractions of the bladder elicit strong contraction of the sphincter, which then suppresses the contraction.
Drugs used to treat bladder overactivity include the following:
-
Anticholinergic drugs, such as propantheline bromide and emepronium bromide
-
Drugs with mixed actions, such as tolterodine, oxybutynin, trospium, solifenacin, darifenacin, and imipramine
-
Beta-adrenergic agonists, such as terbutaline
-
Alpha-adrenergic antagonists, such as phenoxybenzamine and prazosin
-
Prostaglandin inhibitors, such as the nonsteroidal anti-inflammatory drugs (NSAIDS)
Antispasticity drugs, such as diazepam and baclofen, also have been used in upper motor neuron dysfunction. As a rule, calcium channel blockers are not used therapeutically for uninhibited contractions, but in theory, they should be effective. Interest has increased in the use of botulinum toxin to treat the overactive bladder in demyelinating diseases and to address detrusor overactivity after spinal cord injury. [42]
Stress incontinence occurs when intra-abdominal pressure exceeds resistance at the bladder neck. Medical management is focused on increasing pelvic floor function. Estrogen replacement helps restore mucosal function, which in the female plays a large role in maintaining intraurethral pressure.
Drugs that increase outflow resistance include alpha-agonists. Ephedrine and phenylpropanolamine have been used, but their adverse effects, such as palpitations, headache, and tremor, can be troublesome. Imipramine (and other tricyclic antidepressants) decrease bladder activity but also increase outflow resistance.
Failure to empty
Failure to empty occurs in the presence of inadequate detrusor contraction or excessive outflow resistance. Drugs that stimulate bladder contraction include parasympathomimetics, such as carbachol and bethanechol; the latter is more specific for the muscarinic receptors of the bladder. Drugs that act on the urethra to decrease outflow resistance include alpha-adrenoceptor antagonists, such as phenoxybenzamine and prazosin.
Nonmedical Management of Voiding Dysfunction
Nonmedical treatment of incontinence involves the use of pelvic floor muscle training, tibial nerve stimulation, biofeedback, pessaries, bladder retraining, and sometimes intermittent catheterization. [43, 44] For mild stress incontinence, Kegel exercises may increase pelvic muscle tone enough to correct the problem.
Inserts around which the muscles can contract can be placed in the vagina. Stimulators, also placed in the vagina, produce tonic contraction of the sphincter and pelvic floor, which both increases outflow resistance and decreases uninhibited contractions. Intractable cases may be treated with implanted sacral nerve stimulators. [45] Sacral neuromodulation can be successful in patients with voiding dysfunction and a history of spinal surgery; however, those with urge incontinence are less likely to report significant improvement. [46]
Various surgical procedures have been developed for managing incontinence, largely stress incontinence in women. In aging postmenopausal women, pelvic floor laxity complicated by pelvic floor neuromuscular damage incurred during labor and delivery predisposes to descent of the bladder neck, cystocele formation, and decreased outflow resistance. All these factors produce a mechanical type of incontinence that is managed by reestablishing the normal relationship of the bladder neck and trigone to the pelvic floor.
Although many women can be treated successfully by inserting a pessary, the highest rate of cure has been reported in those who undergo suprapubic bladder-neck suspension or a pubovaginal sling procedure. Cystoceles are treated with anterior repair of the vagina, often in conjunction with removal of a prolapsed uterus. The use of injectable bulking agents, such as polytetrafluoroethylene (PTFE; Teflon) or collagen, may increase urethral resistance, but long-term results have been poor.
In failure to become dry, especially after pelvic surgery, irradiation, or history of difficult vaginal deliveries, a fistula must be considered.
Stimulators of various sorts have been developed over the past 30 years to attempt to manage voiding dysfunction. These are implanted devices placed on spinal roots.
The incontinence seen in patients with parkinsonism, dementia, cerebrovascular disease, or multiple sclerosis may be a combination of true bladder dysfunction and decreased mobility. About 35% of such patients may have detrusor hyperactivity and decreased bladder capacity. Anticholinergic drugs are helpful, as is timed voiding. When mental function is decreased, behavior modification, frequent toileting, and avoidance of sedatives can decrease the frequency of “accidents.”
Nonneurogenic Neurogenic Bladder
Occasionally, children exhibit what appears to be a neurogenic bladder without any other evidence of neurologic dysfunction. This “nonneurogenic” neurogenic (ie, Hinman) bladder is an acquired dysfunction that is seen most frequently in young girls but may also be seen in women after painful pelvic surgery.
Early toilet training proceeds normally, but at some point, usually at about the time they enter school, these children develop a pattern of holding back and suppressing bladder contractions. This may be from fear of using a toilet away from home or of being bullied at school. Eventually, the bladder becomes distended and insensitive. The sphincters intermittently relax, with resultant leakage. With attempts to void, the stream is slow, and the child cuts it off before emptying completely.
This condition also may affect bowel function and, in extreme cases, may resemble Hirschsprung disorder. Frequent urinary tract infections are the rule in these patients. Urethral dilatations may help transiently. This disorder requires psychological intervention as well as timed voiding, keeping a voiding diary, and often intermittent catheterization until bladder elasticity returns. This is not a neurologic disorder.
Questions & Answers
Overview
Why is the urologic management in neurologic disease important?
What is the neuroanatomy of pelvic floor relevant to the urologic management of neurologic disease?
What is the role of sphincter EMG in urologic management of neurologic disease?
What is the role of reflex responses in the urologic management of neurologic disease?
What is the bladder and pelvic floor function in neuromuscular disorders?
What are the characteristic urologic manifestations of neurodegenerative disorders?
What are the urologic manifestations of multiple sclerosis?
What are the urologic manifestations of spinal cord disorders?
What is iatrogenic voiding dysfunction?
How is voiding dysfunction characterized in neurologic disease?
What is urge incontinence in neurologic disease?
Which drugs are used to treat bladder overactivity in neurologic disease?
What is the role of antispasticity drugs in the urologic management of neurologic disease?
What is stress incontinence in neurologic disease?
How is failure to empty managed in neurologic disease?
How is nonneurogenic neurogenic bladder treated?
-
Pelvic neuroanatomy.
-
Pelvic muscles and fascia.
Tables
What would you like to print?
- Overview
- Neuroanatomy of Pelvic Floor
- Neurophysiology of Pelvic Floor
- Bladder and Pelvic Floor Function in Neuromuscular Disorders
- Urologic Symptoms of Neurodegenerative Disorders
- Urologic Symptoms of Multiple Sclerosis
- Urologic Symptoms of Spinal Cord Disorders
- Iatrogenic Voiding Dysfunction
- Medical Management of Voiding Dysfunction
- Nonmedical Management of Voiding Dysfunction
- Nonneurogenic Neurogenic Bladder
- Questions & Answers
- Show All
- Media Gallery
- References