Overview
Background
Cavernous sinus syndrome describes symptoms comprising ophthalmoplegia, chemosis, proptosis, Horner syndrome, and/or trigeminal sensory loss evoked by vascular, inflammatory, traumatic, congenital, or neoplastic processes affecting the cavernous sinus near the midline of the frontotemporal part at the base of the skull. There are numerous diseases evoking cavernous sinus syndrome. The most often reported are: intra- and extracavernous or metastatic neoplasms, intra-cavernous carotid artery aneurysms, carotid-cavernous fistulas (see image below), infections, thrombosis, and Tolosa-Hunt syndrome.
Clinical Presentation
History
The signs and symptoms frequently found in patients with cavernous sinus lesions include visual loss, proptosis, ocular and conjunctival congestion, elevation of ocular pressure, ophthalmoplegia, and pain. Various combinations of these symptoms may occur, which generally are unilateral but may be bilateral with neoplastic processes. Symptoms may be acute or slowly progressive. Primary tumors are the most frequent neoplasm responsible for a cavernous sinus syndrome.
Cavernous sinus tumors
Acute or slowly progressive ophthalmoplegia is the dominant presentation, with diplopia being the most common symptom. At times, painful diplopia is present.
Usually the patient has a preceding history of cancer. Occasionally, cavernous sinus syndrome is the first manifestation of a systemic neoplasm (leukemia, lymphoma).
Exophthalmos can be observed.
If the tumor is a pituitary macroadenoma, endocrine symptoms and/or visual field deficits may be present.
Carotid-cavernous aneurysms
Patients frequently are elderly and present with subacute or chronic ophthalmoplegia. Rarely, they may have pain similar to that of trigeminal neuralgia.
Spontaneous rupture of a carotid-cavernous aneurysm leads to an abrupt onset of a direct C-C fistula. This results in acute onset of massive exophthalmos with orbital, ocular, and conjunctival chemosis, binocular diplopia, and visual loss.
There are two types of C-C fistulas. Direct fistulas present with prominent acute symptoms. Indirect fistulas are characterized by mild proptosis, chronic diplopia, drooping of the lid, a red eye, arterialization of the conjunctival vessels, and visual loss. The patient may report subjective "noises" in his or her head.
Cavernous sinus thrombosis
This is infrequent in the antibiotic era.
It may occur as a complication of spreading infection from the ethmoid, sphenoid, or frontal sinuses or from midfacial, dental, or orbital infections.
Patients may present with sepsis or metastatic spread of septic emboli, most commonly occurring in the lung. This presentation may appear as acute respiratory distress syndrome (ARDS).
Retrobulbar pain, drooping of the upper eyelid, and diplopia may be the first symptoms indicating the lesion's extension to the cavernous sinus.
Miscellaneous inflammatory lesions
These may involve the cavernous sinuses or the walls of the sinus.
Herpes zoster in its acute or chronic stage rarely causes pain, diplopia, and a droopy eyelid in addition to the typical zoster blisters. In the chronic stage, a scar from the acute lesion usually is found.
An idiopathic inflammation of the walls of the cavernous sinuses is referred to as Tolosa-Hunt syndrome.
Sarcoid or Wegener granulomatosis may also predispose to cavernous sinus syndrome.
Physical
Cavernous sinus lesions are characterized by the following signs:
-
Unilateral and isolated third, fourth, or sixth cranial nerve palsy
-
Variety of combination nerve palsies resulting in partial or complete ophthalmoplegia
-
Painful ophthalmoplegia
-
Proptosis (pulsating exophthalmos suggests a direct C-C fistula)
-
Ocular and cranial bruits
-
Conjunctival congestion; arterialization of conjunctival veins
-
Ocular hypertension
-
Optic disc edema or pallor; retinal hemorrhages
-
Anesthesia in the ophthalmic division of the trigeminal nerve (V1) and/or decreased or absent corneal reflex and possibly anesthesia in the maxillary or V2 branch
-
Pupil in mid-position and nonreactive if both sympathetic and parasympathetic fibers of the third nerve are affected
Cavernous sinus tumors
Metastatic lesions: Isolated or combined ophthalmoplegia, painful ophthalmoplegia, anesthesia in the ophthalmic nerve
Pituitary tumors: Isolated or combined ophthalmoplegia (lateral extension); endocrine signs such as acromegaly, gigantism, galactorrhea, Cushing’s disease, and temporal or bitemporal visual field defects
Primary intracranial tumors: Isolated or combined ophthalmoplegia and/or primary aberrant regeneration of the third cranial nerve
Cavernous sinus aneurysms
Isolated or combined ophthalmoplegia
Painful ophthalmoplegia
Decreased pain sensation in the V1 ophthalmic division
Carotid-cavernous fistulas
Direct: Unilateral massive proptosis, pulsating exophthalmos, lid congestion, conjunctival chemosis, orbital congestion, ocular hypertension, visual loss, optic neuropathy, optic disc edema, retinal hemorrhages, retinal venous congestion, and loud ocular and cranial bruit
Indirect: Similar signs and symptoms of lesser severity; occasionally, isolated ophthalmoplegia, particularly if the fistula drains posteriorly
Cavernous sinus thrombosis
Generally speaking, primary infectious process involving paranasal sinuses and/or orbital cellulitis
In addition to local and systemic signs of infection, the following may be seen:
-
Isolated or combined ophthalmoplegia
-
Painful ophthalmoplegia
-
Orbital congestion, lid chemosis, proptosis
-
Visual loss, optic disc edema (unilateral)
-
Signs of meningeal irritation
Miscellaneous cavernous sinus lesions
Tolosa-Hunt syndrome: Isolated or combined, painful ophthalmoplegia
Herpes zoster: Acute zoster ophthalmicus, typical skin lesion, and keratitis
Sarcoidosis: Systemic signs, uveitis, ophthalmoplegia, facial diplegia
Causes
Metastatic tumors
-
Breast
-
Prostate
-
Lung
Localized spread of tumor
-
Nasopharyngeal
-
Pituitary
Primary intracranial tumors
-
Meningiomas
-
Neurofibromas
-
Chondromas (less common)
-
Lymphomas
Trauma (including postsurgical)
-
Carotid-cavernous aneurysms
-
Carotid-cavernous fistulas
-
Cavernous sinus thrombosis
Miscellaneous inflammatory syndromes
-
Herpes zoster
-
Tolosa-Hunt syndrome
-
Sarcoidosis
-
Tuberculosis
-
Wegener granulomatosis
Diagnostic Workup
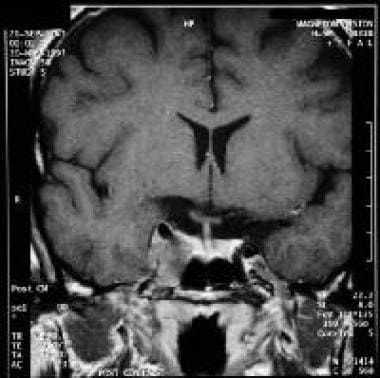
Patients in whom cavernous sinus lesions are suspected should undergo thin-section multiplanar imaging studies of the orbit and the sellar/parasellar region. Pre-contrast and postcontrast scans are advisable. CT scan offers better visualization of bone structures. However, MRI using T2, fluid-attenuated inversion recovery (FLAIR), pre-contrast and post-contrast T1-weighted with a fat saturated protocol images provide better detail of all soft tissues contained in the sinuses, the expected signal void of the carotid artery (image below), and its relation to the surrounding structures as well as individual nerves if the thin-section 3D are acquired.
Orbital views are necessary to exclude a disease process primarily involving the cavernous sinuses with concomitant compromise of the orbital apex. Conversely, primary orbit and paranasal sinus disorders frequently may involve the cavernous sinuses. Visualization of the superior and inferior orbital veins is helpful to diagnose increased venous pressure. Once imaging is obtained and reviewed in light of clinical findings, further investigation can be pursued to determine a specific diagnosis.
Cavernous sinus tumors
In the case of metastatic tumors, diagnosis of the primary neoplasm generally precedes the cavernous sinus syndrome.
A lumbar puncture with cytologic examination can be helpful.
If a primary neoplasm of the nasopharynx is suspected, a biopsy may be needed.
In the case of pituitary tumors with lateral extension, tumor resection may be necessary.
Rarely, a biopsy of the cavernous sinus tumor is needed for diagnosis.
Cavernous sinus aneurysms
As MRI and/or magnetic resonance angiography (MRA) are often specific, cerebral angiography generally is not required to make a diagnosis.
Perform arteriography if endovascular occlusion of the aneurysm or fistula is planned.
Carotid-cavernous fistulas
The dramatic clinical presentation and MRI and/or MRA of direct fistulas leave little doubt regarding the diagnosis.
By contrast, indirect fistulas, particularly those draining into the petrosal sinuses, are associated with subtle findings and possibly a normal MRI and/or MRA (images below).
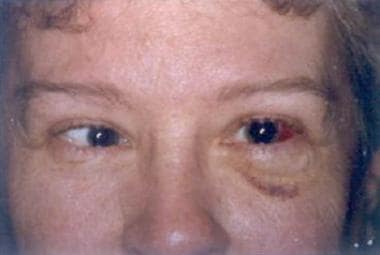 This patient is a 55-year-old woman who originally had symptoms of eye pain and pulse synchronous tinnitus on the left. She was found to have an indirect left carotid cavernous sinus fistula and underwent successful coiling of the fistula. This picture shows her after the procedure, as she had developed left eye chemosis and diplopia. A left lateral rectus paralysis was present on examination. In this case, the probable causes of the ophthalmoplegia could be mass effect or occlusion of the vasa nervorum supplying the sixth cranial nerve, which travels in the adventitia of the carotid artery. Here, the prognosis is excellent, and the authors have seen several cases with improvement within 4-8 weeks after coiling.
This patient is a 55-year-old woman who originally had symptoms of eye pain and pulse synchronous tinnitus on the left. She was found to have an indirect left carotid cavernous sinus fistula and underwent successful coiling of the fistula. This picture shows her after the procedure, as she had developed left eye chemosis and diplopia. A left lateral rectus paralysis was present on examination. In this case, the probable causes of the ophthalmoplegia could be mass effect or occlusion of the vasa nervorum supplying the sixth cranial nerve, which travels in the adventitia of the carotid artery. Here, the prognosis is excellent, and the authors have seen several cases with improvement within 4-8 weeks after coiling.
 Early phase of the post-fistula coiling angiogram of the patient shown above. Coils can be appreciated at the cavernous portion of the carotid artery.
Early phase of the post-fistula coiling angiogram of the patient shown above. Coils can be appreciated at the cavernous portion of the carotid artery.
 Later filling phase of the angiogram for the patient shown above. Note that coiling has prevented anomalous filling of the cavernous sinus fistula.
Later filling phase of the angiogram for the patient shown above. Note that coiling has prevented anomalous filling of the cavernous sinus fistula.
Cerebral angiography is the only way to arrive at the correct diagnosis.
Perform angiography to stage the fistula and document the anterior and posterior drainage routes.
Cavernous sinus thrombosis
Imaging of the orbit and/or nasal sinuses is helpful in the search for an infectious/inflammatory source.
An aseptic thrombosis may be associated with conditions such as hyper-coagulopathy and lymphoproliferative disorders.
A hematologic workup is indicated in these patients.
Miscellaneous inflammatory syndromes
Other systemic inflammatory and granulomatous processes have to be investigated after more common causes have been excluded. These disorders can be screened by additional laboratory tests and chest radiograms.
Tolosa-Hunt syndrome (an uncommon, idiopathic, inflammatory cavernous sinus syndrome) shares a close etiologic link with orbital pseudotumor.
A nonspecific fibrotic inflammatory reaction and rarely a granulomatous inflammation can occur, but biopsy is rarely used to establish the diagnosis.
A positive response to steroids is considered diagnostic, but false-positive responses can occur in lymphoma and other parasellar neoplasms.
Biopsy of the cavernous sinuses entails a craniotomy, which is associated with morbidity. Restrict a craniotomy to patients with a documented, progressive cavernous sinus syndrome.
Treatment & Management
Cavernous sinus tumors
Metastatic lesions
-
Radiotherapy may offer transient improvement
-
Nasopharyngeal carcinomas may be very radiosensitive, with a prolonged remission following treatment
Pituitary tumors
-
Prolactinomas may improve with oral dopamine agonists, or they may require resection
-
Gamma knife may be an adjunctive treatment for postoperative tumor residual or recurrent tumor, and it may have a role as an alternative to open surgical treatment.
Cavernous sinus meningiomas
-
These lesions represent a major challenge for surgical resection, primarily because of poor accessibility and the frequent encasement of the cavernous carotid artery.
-
Since these tumors are slow growing and difficult to resect, elderly patients or those with minor symptoms probably should be observed expectantly without specific treatment.
-
Radiotherapy may be offered to some patients, and some show improvement of cranial nerve function after gamma knife treatment. Partial resection may be attempted in others with disabling symptoms (eg, intractable pain, total ophthalmoplegia in a patient with poor vision in the nonparetic eye).
Cavernous sinus aneurysms
Treat cavernous sinus aneurysms by endovascular balloon occlusion.
Carotid-cavernous fistulas
Treatment ideally consists of endovascular obliteration of the fistula with coils, although some cavernous sinus dural arterio-venous fistulas may be managed observationally.
Access to the fistula may be intraarterial; however, the transvenous approach has become the mainstay of treatment, in some cases a combined surgical/endovascular approach can be used with surgical exposure of the superior ophthalmic vein followed by fistula embolization. Several venous approaches have been used, including the safest transfemoral approach; however, if this is not feasible, a superior orbital vein or a percutaneous trans-orbital puncture to the cavernous sinus can be used. [4]
Supraorbital vein dissection with placement of a catheter to access the cavernous sinuses has been performed successfully.
Percutaneous trans-orbital access to the cavernous sinus followed by embolization.
Small indirect C-C fistulas may occlude either spontaneously or following diagnostic angiography. If the clinical signs are mild, consider careful monitoring.
If intraocular pressure is elevated, antiglaucoma agents may be required.
Cavernous sinus thrombosis
High-dose antibiotic therapy should be directed against the most common pathogens, such as S. aureus and S. pneumoniae, as well as gram-negative rods and anaerobes.
Anticoagulation in cavernous sinus thrombosis evoked by infection is controversial, but may hasten recovery.
Drainage of any primary site of infection (eg, abscess, sinusitis) is advised.
Corticosteroids are not recommended.
Anticoagulation also may be helpful in aseptic patients.
Miscellaneous inflammatory syndromes
Inflammatory cavernous sinus syndromes may respond to treatment of the specific systemic inflammation or vasculitis.
Tolosa-Hunt syndrome responds well to a 3- to 6-month course of high-dose steroid therapy that can be tapered slowly thereafter.
Pathophysiology
The cavernous sinuses are interconnected, multi-channeled venous structures located on both sides of the sella turcica (ST; see image below) with the pituitary gland inside (PG). Cavernous sinus extends from the orbital apex to the Meckel cave. Each sinus consists of venous channels bordered by dura matter and collects blood from the superior and inferior orbital veins, pterygoid plexus, and the Sylvian vein draining into the superior and inferior petrosal sinuses. Inside the cavernous sinus there is an intra-cavernous part of the carotid artery (ICA) with its sympathetic plexus (SP). Within the lateral wall there are cranial nerves III (oculomotor), IV (trochlear), V1 (ophthalmic branch of trigeminal nerve), and V2 (maxillary branch of trigeminal nerve); the VI nerve (abducens) is in the vicinity of the internal carotid artery (see image below). The presence of those cranial nerves within cavernous sinus is responsible for characteristic cavernous sinus syndrome symptoms of partial or complete ophthalmoplegia a facial sensory losses, which can be accompanied by facial pain and exophthalmos.
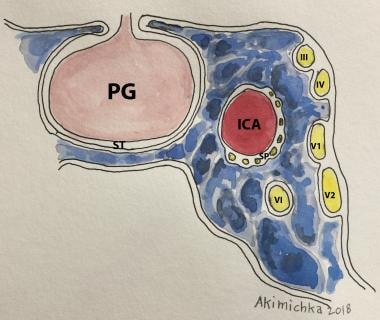 The figure depicts the frontal view of structures in the vicinity of the left cavernous sinus; details are in the text. PG-pituitary gland, ST-sella turcica, ICA-internal carotid artery, SP-sympathetic plexus, III-VI, cranial nerves. Courtesy of Akimichka.
The figure depicts the frontal view of structures in the vicinity of the left cavernous sinus; details are in the text. PG-pituitary gland, ST-sella turcica, ICA-internal carotid artery, SP-sympathetic plexus, III-VI, cranial nerves. Courtesy of Akimichka.
Cavernous sinus neoplasms
Cavernous sinus tumors are the most common cause of cavernous sinus syndrome. Tumors may be primary or arise as either local spread or metastases. Examples of primary tumors include schwannoma, plexiform neurofibroma, malignant peripheral nerve sheath tumor, cavernous hemangioma, meningioma, melanocystoma, chondroma and chondrosarcoma. Examples of locally spreading tumors are nasopharyngeal carcinoma, pituitary adenoma, chordoma, epidermoid and dermoid cyst. Metastatic lesions are most often from the breast, prostate, or the lung. Total resection of these lesions remains very challenging and, in many cases, impossible if the lesion is invasive. [1] Other treatment solutions include radiotherapy, which often offers transient relief, particularly in nasopharyngeal cancer. Lateral extension of pituitary tumors may be treated with surgical resection and dopamine agonists in the case of prolactinoma. [1, 26]
Cavernous sinus aneurysms
Unlike intracranial aneurysms in the extradural locations, carotid-cavernous aneurysms do not involve a major risk of subarachnoid hemorrhage but often are giant (>2.5cm in diameter). Thus they produce symptoms through compression of the adjacent structures and their rupture can result in direct C-C fistulas. These aneurysms, which are more frequent in the elderly, often present with an indolent ophthalmoplegia. Although some patients suffer minor disability and do not require treatment, endovascular coiling is often successful and is attempted in many patients. [2, 26]
Carotid-cavernous fistulas
C-C fistula is an abnormal connection between the carotid artery and the sinus. There are 2 main types of C-C fistulas. Direct fistula (type A) is characterized by a high blood flow communication between the carotid artery and cavernous sinus. It manifests with a sudden onset of pulsating exophthalmos, proptosis, chemosis, visual loss, and usually painful ophthalmoplegia (Figure above). Trauma or aneurysm rupture is a common cause of a direct carotid-cavernous fistula. Dural fistula (types B–D) occurs when communication develops between the cavernous sinus and the meningeal or persistent fetal branches of the internal carotid artery, external carotid artery, or both. This type has a milder and more insidious presentation than a direct fistula, often with spontaneous resolution. Interventional radiologists can successfully treat all fistula types by endovascular occlusion techniques. Occasionally, surgical treatment with carotid ligation is necessary; this sometimes is preceded by a superficial temporal-to-middle cerebral bypass to ensure cerebral circulation after carotid ligation. [26]
Cavernous sinus inflammatory, infectious, and granulomatous lesions
Infection within cavernous sinus or in the adjacent structures can result in sinus thrombosis and/or development of inflammatory changes. The rare but important causes include: aspergillosis, Wegener granulomatosis, tuberculosis, and sarcoidosis. Some of these share symptoms with Tolosa-Hunt syndrome (unilateral ophthalmoplegia, cranial nerve palsies, and a dramatic response to corticosteroids), which describes a retroorbital pseudotumor encroaching the cavernous sinus. [26]
Epidemiology
Frequency
In the United States, approximately 5% of ophthalmoplegias are secondary to involvement of cranial nerves in the cavernous sinuses. This is probably true worldwide.
Cavernous sinus aneurysms represent 5% of giant intracranial aneurysms. [26]
Mortality/Morbidity
Most of the lesions affecting the cavernous sinuses are treatable.
Metastatic cancer is a frequent cause of cavernous sinus syndromes, and the prognosis depends on the specific tumor type.
Cavernous sinus septic thrombophlebitis mortality has decreased from 100% to 20% with the improvement of diagnosis and therapies.
Cavernous sinus aneurysms and C-C fistulas can be treated successfully by endovascular techniques.
Lateral extension of pituitary tumors, a common cause of this syndrome, can be treated by surgical resection, radiation therapy in selected patients, and a dopamine agonist in the case of prolactinoma.
-
Carotid-cavernous fistula.
-
A T1-weighted, coronal MRI.
-
This patient is a 55-year-old woman who originally had symptoms of eye pain and pulse synchronous tinnitus on the left. She was found to have an indirect left carotid cavernous sinus fistula and underwent successful coiling of the fistula. This picture shows her after the procedure, as she had developed left eye chemosis and diplopia. A left lateral rectus paralysis was present on examination. In this case, the probable causes of the ophthalmoplegia could be mass effect or occlusion of the vasa nervorum supplying the sixth cranial nerve, which travels in the adventitia of the carotid artery. Here, the prognosis is excellent, and the authors have seen several cases with improvement within 4-8 weeks after coiling.
-
Early phase of the post-fistula coiling angiogram of the patient shown above. Coils can be appreciated at the cavernous portion of the carotid artery.
-
Later filling phase of the angiogram for the patient shown above. Note that coiling has prevented anomalous filling of the cavernous sinus fistula.
-
The figure depicts the frontal view of structures in the vicinity of the left cavernous sinus; details are in the text. PG-pituitary gland, ST-sella turcica, ICA-internal carotid artery, SP-sympathetic plexus, III-VI, cranial nerves. Courtesy of Akimichka.