Introduction/ Historical Perspective
This article is based on the updated 2016 American Academy of Sleep Medicine Manual for the Scoring of Sleep and Associated Events. [1] This manual represents the evolution and development of the 2007 AASM manual which was itself a restructuring, consolidation, and standardization of the original Rechtshaffen and Kales sleep scoring manual of 1968, commonly known as the "R and K" rules. [2]
Prior to the R and K rules, electroencephalographic (EEG) recording revealed distinct brain rhythms uniquely seen during sleep but were yet to be universally defined and categorized. Loomis and colleagues [3] noted fragmentation and fallout of alpha rhythm with sleep onset, the appearances of sleep spindles, K complexes and high amplitude slow waves. Sleep was divided into five stages (A-E), with later stages possessing more slow-frequency and high-amplitude waves [3] . The discovery of rapid eye movement (REM) sleep by Kleitman and Dement in 1957 [4] led to a classification of sleep stages that included REM sleep.
In 1968, Rechtschaffen and Kales convened a panel of experts to agree on a standardized manual for the scoring of sleep stages, which were then divided into wakefulness, stage 1-4 (non-REM), and REM. At least one EEG lead was recommended (C3 or C4 referenced to the opposite ear or mastoid) as well as two electrooculogram (EOG) leads and a submental electromyography (EMG) lead. The R and K rules recommended dividing the polysomnographic record of sleep into thirty second epochs, commencing at the start of the study. Historically, the 30-second interval was used because at a paper speed of 10 mm/s, ideal for viewing alpha and spindles, one page equates to thirty seconds. Each epoch was assigned a stage and if two or more stages coexist during a single epoch the stage comprising the majority of the thirty seconds was scored.
In 2004, the American Academy of Sleep Medicine (AASM) commissioned a steering committee to assemble a new sleep scoring manual that would address sleep staging as well as the scoring of arousals, respiratory, cardiac, and movement events. Eight separate task forces were assembled to address the various issues. The establishment of rules was guided by the following principles: the rules should be compatible with published evidence, they should be based on biologic principles, they should be applicable to both normal and abnormal sleep, and they should be easy to use by clinicians, technologists, and scientists.
In 2007, after three years of study, the AASM released their update which introduced key changes to the R and K system. The main revisions to sleep scoring from that manual included placement of a frontal EEG derivation in addition to the commonly used central and occipital leads. Previously, the R and K system required that the central lead always be used if only one derivation was possible, however, the AASM’s approach called for the utilization of frontal, central and occipital leads in all studies. Another major change was a reclassification of sleep stages to stage W (wake), stages N1-N3 (non-REM), and stage R (REM) from the previously described R and K stages of Wakefulness, 1-4, and REM. [5] The change in abbreviations is to avoid confusion between the two classification systems, where Stage 3 and 4 in the old R and K rules were combined to form stage N3 in the new rules since no physiologic or clinical basis has been found for a difference between Stages 3 and 4.
In the years following the transition from R and K to the adoption of the AASM scoring system of 2007 there have been some notable changes to polysomnographic data analysis with potential clinical effects. Outlined in a review from 2012, these include, but may not be limited to, large variances in adult apnea-hypopnea indexes when scored using the recommended versus alternative rules, decreases in N2 sleep with increases in N1 sleep and sleep transitions due to a rule governing transition from N2 to N1 sleep, increased N3 sleep in adults with the addition of frontal EEG lead tracings and improved slow wave detection, and improved interscorer reliability [6] . This article focuses on sleep stage scoring criteria from the 2015 AASM Manual [1] .
In April 2016, minor clarifications were made to the sleep scoring manual. The two changes that pertain to sleep staging are: 1) how to score epochs when multiple stages are present and 2) how to better capture arousals.
Polysomnographic Leads and Recommended Technical Requirements for Sleep Scoring
Sleep stage scoring is a rule-based neurophysiological characterization requiring an understanding of the basic mechanisms underlying the generation of cephalic electric potentials coupled with eye movements and muscle signals. Signals of interest are generated from the brain (ie, cortex and deeper structures), facial muscles as noted by the submental EMG, and eye movement as detected by the EOG.
Interference with the signals of interest is encountered through many mechanisms, including physiological attenuation of the cerebral electric potentials by scalp muscle and bone, intrusion into the signal by slow cyclic respiration, movement, ECG signal, external electric fields, and impaired contacts between the recording electrodes and the skin surface. Discriminating true signal from artifact can be one of the most challenging aspects of scoring sleep stages.
Cortical Signals
The EEG signal is of primary importance in interpreting polysomnographic studies. [7, 8, 9] It records electric potentials generated by the interaction between the cortex and the deeper brain structures, especially the thalamus. Two frontocortical (F3, F4), two centrocephalic (C3, C4), and two occipital (O1, O2) channels are recorded in accordance with the international 10/20 placement system. The left channels are ascribed odd numbers and the right channels are ascribed even numbers. Measurement of EEG signals is possible because of the relative difference in potential between two recording electrodes. Negative potentials, by convention, are represented by an upwardly deflecting wave. [10, 11]
These EEG sites reference all left and right electrodes to the contralateral mastoid process lead (M2 or M1). For example, C3 is referenced to M2. Common practice is to read from the right hemispheric channels, however, when a channel develops artifact or the validity of the signal is unclear comparison is made to the corresponding contralateral channel. For instance, if C4-M1 develops artifact, C3-M2 can be used for channel interpretation.
EEG tracings are classified by their frequency with Delta waves having the slowest activity at < 4 Hz, Theta waves ranging from 4-7 Hz, Alpha waves more rapid at 8-12 Hz, and Beta waves exceeding 12 Hz. Electrode placement is specific to capture specific wave types with slow waves best represented in frontal leads, spindles seen more clearly centrally, and Alpha rhythms more pronounced in the occipital region.
Muscle Signals
The EMG signals are muscle twitch potentials that may offer additional assistance in defining a sleep stage. Their use is based on the finding that muscle activity decreases during sleep, with muscle activity at its nadir during REM sleep. In many cases, however, appreciating a decreasing muscle tone can be difficult and the relative silence during REM sleep may not be of help in distinguishing it from the preceding or subsequent sleep stages.
Compounding the problem of interpreting EMG channels is intrusion of artifact into the signal. Some examples include cyclic jaw movements, teeth grinding (bruxism), or steady high-amplitude noise generated by increased pressure on an electrode (eg, as caused by lying on the chin). Additionally, muscle artifact spilling over into cortical leads is not an unusual finding. ECG signal is a specific type of cardiac artifact that can appear in all or several channels and can be recognized by tracking the repeating QRS complex throughout the other leads.
Recommended EMG technical requirements include 3 chin EMG electrodes, 2 of which are used throughout the study with an additional lead as a backup.
Eye Movements
The EOG tracks eye motion via changes in electric potential when the positive anterior aspect of the eye changes position relative to the negative posterior aspect. Recommended lead placement includes one lead placed 1cm below the left outer canthus and 1cm above the right outer canthus. During any eye movement, the cornea (positive) moves toward an electrode, while the fundus (negative) moves away from the same electrode. When the eye is not moving there is no net change in potential and the eye leads do not record a signal.
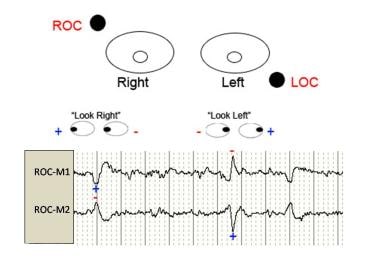 Electro-oculogram. During any eye movement, the cornea (positive) moves toward one electrode, while the fundus (negative) moves away from the same electrode. When the eye is not moving, the change in relative position is zero, and the eye leads do not record a signal. Conjugate eye movements thus cause out-of-phase EOG deflections.
Electro-oculogram. During any eye movement, the cornea (positive) moves toward one electrode, while the fundus (negative) moves away from the same electrode. When the eye is not moving, the change in relative position is zero, and the eye leads do not record a signal. Conjugate eye movements thus cause out-of-phase EOG deflections.
Slow rolling eye movements are recorded as long gentle waves, while rapid jerking movements are represented by sharply contoured fast waves. Blinking of the eyes produces rapid vertical movements. Eye movements during drowsiness and stage N1 sleep may be irregular or gently rolling. In deeper stages of sleep macro eye movements cease altogether but regain activity during periods of REM.
Sleep Stages
Initially, the clinician should scroll through the entire record to evaluate the quality of the recording and the usefulness of specific channels. The major stages should be identified and variability associated with the patient should be noted. Initial review of the biocalibration channels may also be helpful in highlighting general awake waveforms.
General scoring of sleep stages
Sleep will be scored using different stages: Stage W (wakefulness), Stage N1 (NonREM 1), Stage N2 (NonREM 2), Stage N3 (NonREM 3), and Stage R (Rapid Eye Movement).
Sleep is scored using 30-second epochs, starting with the first epoch acquired. Each epoch is scored based on the greatest sleep stage amount comprising that time period. [12] If three or more stages are present, the first step is to determine if there is more wake or sleep. If more sleep is present, then the epoch is assigned the sleep stage that occurs in the majority of that epoch.
Stage W
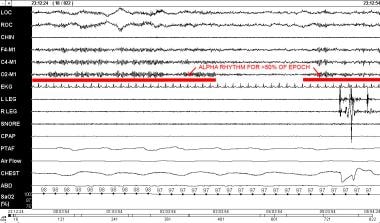
Stage W is scored when there is alpha rhythm in greater than 50% of the epoch (regardless of the epoch’s position in the PSG).
Prior to 2007, Stage W was the equivalent to R and K Stage Wake. The first several epochs of the record will usually be stage W although occasionally a patient is so sleepy that sleep onset may have occurred prior to the recording having been started. In general, during normal wakefulness with closed eyes, Alpha rhythms are detected over the occipital leads with a frequency of 8-13 Hz.
Other features associated with stage W include Beta activity while eyes are open and Alpha activity while eyes are closed on EEG, high-amplitude muscle contractions and movement artifacts on EMG, and eye blinking on EOG.
Up to 20% of normal patients will not have a detectable alpha rhythm on EEG [1] }. In such cases, Stage W may still be scored if one of the three following markers of alertness are detected: eye blinks with the eyes open or closed (with a frequency of 0.5 to 2 Hz); reading eye movements (consisting of a slow phase followed by a rapid movement in the opposite direction); or the presence of irregular conjugate eye movements with normal or high chin muscle tone suggesting that the subject is awake and looking around.
Stage N1
Stage N1 is scored when alpha rhythm is attenuated and replaced by low amplitude, mixed frequency signal of 4-7 Hz for more than 50% of the epoch.
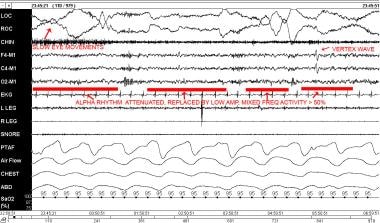 Stage N1. Alpha rhythm is attenuated and replaced by low-amplitude, mixed-frequency for more than 50% of the epoch.
Stage N1. Alpha rhythm is attenuated and replaced by low-amplitude, mixed-frequency for more than 50% of the epoch.
Stage N1 is also usually characterized by a decrease in muscle tone as detected by chin EMG when compared with Stage W. Other features of Stage N1 include slow eye movements (SEMs; conjugate, sinusoidal eye movements with an initial deflection usually lasting more than 0.5 seconds); vertex sharp waves (which are prominent sharply contoured waves lasting < 0.5 seconds and maximal over the central region), and a low-amplitude mixed frequency EEG signal. Some patients may not generate an Alpha rhythm, even when their eyes are closed while awake. In such patients distinguishing the onset of sleep is more difficult (see below).
Prior to 2007, Stage N1 was the equivalent to R and K stage I, and embodies the transition from the waking to sleeping state. Sleep onset is defined as the first epoch scored as any stage other than Stage W.
For patients who do not generate Alpha rhythms Stage N1 may be scored based on the presence of the following: vertex sharp waves, slow eye movements, or EEG activity in the range of 4-7 Hz with slowing of the background frequencies of the EEG by 1 Hz or more when compared with stage W. SEMs may begin even in wakefulness, thus, stage N1 may be scored earlier in patients without a discernible alpha rhythm.
Stage N2
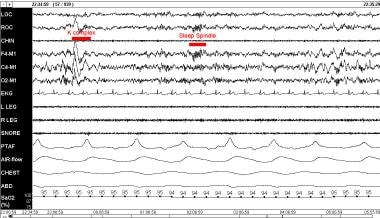
Stage N2 sleep is scored when either one or more K complexes is noted (and unassociated with an arousal) or one or more trains of sleep spindles appear.
Stage N2 sleep should continue to be scored in subsequent epochs of mixed frequency, low-amplitude activity even if K complexes or sleep spindles are absent. Stage N2 sleep should no longer be scored when one of the following five morphological changes occur: (1) there is a transition to Stage W; (2) an arousal (see “special considerations” below; (3) a major body movement followed by slow eye movements and low-amplitude mixed EEG without nonarousal associated K complexes or sleep spindles; (4) transition to stage N3; (5) transition to stage R.
Stage N2 is the equivalent to the R and K stage II. It is characterized by the presence of sleep spindles and K complexes on a background of low-amplitude, mixed frequency EEG activity.
Sleep spindles are trains of higher frequency bursts that were named according to their shapes, which tend to have tapering ends. They are seen maximally over the central leads, have a frequency of 11-16 Hz, and last 0.5 seconds or longer. K complexes are well-delineated, negative, sharp waves followed by a positive deflection and tend to stand out from the background signal. Their duration is 0.5 seconds or longer and are more commonly encountered over the frontal derivations.
K complexes can also be associated with arousals but are only counted as such when the arousal is concurrent with the K complex or commences within one second of the end of the K complex.
Stage N3
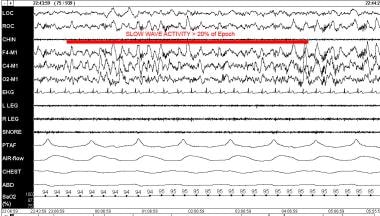
Stage N3 sleep is scored when there is slow wave activity in at least 20% of the epoch, irrespective of age. If slow waves represent less than 20% of the epoch it will be scored under the rules for a different stage.
Stage N3 is the combination of R and K Stage II and IV, and often referred to as slow wave sleep. It is characterized by waves with a frequency of 0.5 to 2 Hz that have amplitudes of 75 microvolts peak to peak. These waves are usually best detected over the frontal leads, which were added in the 2007 AASM recommendations, and helps explain the increase in N3 sleep seen in AASM Manual versus R and K scored studies.
Although not required for scoring, sleep spindles may persist in stage N3 sleep. Also, K complexes may also be present but would be considered as slow waves if they meet the above definition of slow wave activity.
Eye movements are unusual in this stage and are typically not seen. EMG tone is variable but tends to be low, even approaching levels as low as Stage R.
Stage R
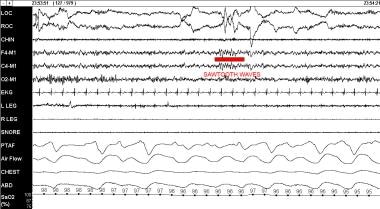
Stage R is scored in epochs that contain all of the following characteristics: the demonstration of rapid eye movements (REMs; irregular, conjugate, sharply peaked eye movements with an initial phase lasting less than 500msec detected in the EOG); EEG signals comprised of relatively low-amplitude and mixed-frequency activity; and muscle tone at the lowest of any stage in the polysomnogram as detected by EMG. [13]
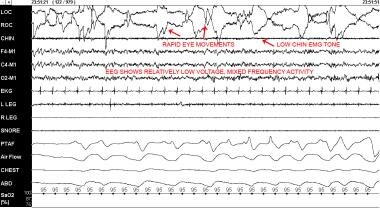 Stage R. This demonstrates rapid eye movements, relatively low EMG tone, and low-voltage, mixed-frequency EEG activity.
Stage R. This demonstrates rapid eye movements, relatively low EMG tone, and low-voltage, mixed-frequency EEG activity.
Epochs following stage R continue to be scored as stage R unless (1) there is a clear change to another sleep stage, (2) an arousal or major body movement followed by slow eye movements take place, or (3) K complexes or sleep spindles, hallmarks of stage N2 sleep, occur in the absence of REMs.
Stage R is the equivalent to the R and K Stage REM and is characterized by muscle atonia with rapid eye movements. Polysomnographic features that are supportive of but not required in stage R include sawtooth waves and phasic muscle twitches. Sawtooth waves are 2-6 Hz serrated bursts of activity, maximal centrally, that often, but not always, precede rapid eye movements. Phasic muscle twitches are brief bursts of irregular EMG activity lasting less than 0.25 msec, superimposed on a persistently low EMG tone, which may be detected on chin EMG, anterior tibialis EMG, or EOG-EEG leads. Muscle activity detected as EEG and EOG signals indicate activity of cranial nerve innervated muscles of the face and scalp.
There is special consideration given to the transition between N2 and REM stages. In a single epoch, if REMs are present with low chin EMG, the epoch is scored as Stage R even if sleep spindles and K complexes are present (this situation is more common in the first REM period of the night). If REMs are absent, chin tone is low, and K complexes/spindles are present, the epoch is Stage R when the K complex/spindle occurs in the second half of the epoch and N2 if they occur in the first half. The epoch following a Stage R epoch with a K complex/spindle in the second half is scored as N2 unless all three Stage R criteria are present. Any increase in muscle tone in conjunction with a K complex and/or spindle results in the epoch scored as N2. The epoch following a sleep spindle remains REM unless there is an associated muscle tone increase and development of slow eye movements.
Special Considerations
Arousals
Arousals are paroxysms of activity (Alpha, Theta or frequency > 16 Hz, but no sleep spindles) lasting 3 seconds or longer with at least 10 seconds of sleep preceding the change. Arousals are used for computation of the arousal index (number of arousals per hour from lights off to lights on. The minimum arousal is simply a paroxysmal burst in the EEG channel, usually to alpha or theta activity. Arousals can be scored during any stage.
If the burst results in alpha activity for greater than 50% of the record, then the epoch is scored as wake. In addition to being recorded as a transition to wakefulness, an arousal is still scored. In this case both an arousal and a transition are scored. Arousals are scored in epochs of wake when 10 seconds of continuous sleep are present.
Arousal from stage N1 is common and usually represented by a burst of activity on the EEG, EOG, and EMG. For an arousal to be scored during REM, there also must be an increase in the submental EEG for at least 1 second.
Major body movements
At times, movement and muscle artifact obscures the EEG for more than half the epoch such that the stage cannot be determined. In such cases, the epoch is scored as Stage W when alpha rhythm is present for any part of the epoch. Epochs with a major body movement, but no discernable alpha rhythm, that precede or follow an epoch of stage W are scored as stage W. If neither criteria can be met the epoch is scored as the same stage as the epoch that follows it.
Normative Sleep Stage Data
Normative values have been constructed based on sleep staging results to help quantify the composition and quality of sleep. Normative data change with age and vary from center to center. In addition, most were collected using the R and K rules.
The AASM manual has recommended recording the values listed below.
For the purposes of illustration, normative data for different age groups is presented (see Table 1 below). It is important to note that “normal” sleep varies greatly by age with a large decrease in the amount of REM sleep from infancy to young adulthood and other significant decreases in slow wave sleep, sleep efficiency, and total sleep time with advancing age.
Total Sleep Time (TST) = Total minutes of sleep = Stage N1 + N2 + N3 + stage R.
Time in Bed (TIB) or total recording time = Monitoring period = Lights out to lights on.
Sleep Latency (SL) = Total number of minutes from lights out to sleep onset.
Stage R Latency = Time from sleep onset to first epoch of REM sleep.
Wake After Sleep Onset (WASO) = Minutes of Stage W that occur throughout the night after initial sleep onset and before the final awakening.
Sleep Efficiency (%) = (TST/TIB) x100%.
Total Time in Each Stage = Separate values for stage N1, N2, N3, and R.
Percent of TST in Each Stage = (Time in each stage/TST) x 100%
Table 1. Normative Sleep Stage Data Across Age Groups.* (Open Table in a new window)
Age (y) |
20-29 |
30-39 |
40-49 |
50-59 |
>60 |
TST (min) |
374.9 |
375.8 |
370.2 |
366.6 |
348.8 |
Sleep Efficiency (%) |
94.4 |
94.4 |
90.2 |
90.4 |
85.8 |
Sleep Latency (min) |
6.3 |
10.0 |
8.4 |
6.1 |
8.2 |
Number of Awakenings |
6.3 |
4.7 |
8.4 |
9.7 |
12.3 |
Stage R (%TIB) |
22.2 |
23.1 |
20.4 |
20.9 |
16.4 |
Stage N1 (%TIB) |
3.0 |
2.5 |
4.3 |
4.7 |
4.0 |
Stage N2 (%TIB) |
50.5 |
52.8 |
54.6 |
56.7 |
57.6 |
Stage N3 (%TIB) |
18.8 |
16.1 |
10.9 |
8.1 |
7.7 |
Adapted from Hirshkowitz M. Normal human sleep: an overview. Med Clin North Am. May 2004;88(3):551-65. [14] |
|||||
These values are useful in the diagnosis and management of sleep disorders. For example, increased sleep latency may be increased in primary insomnia and decreased in obstructive sleep apnea, whereas Stage R latency may be decreased in narcolepsy.
Sleep architecture changes with advancing age. The percentage of stage R is greatest in neonates, where it may encompass 50% of total sleep time. This proportion decreases gradually to 20-25% at adolescence, with further slight decrease after age 65.
Greater sleep fragmentation also occurs with aging, such that wakefulness is intermixed with sleep. The percentage of Stage N3 sleep decreases with age while percentages of time spent in N1, N2, and WASO increase. To some degree, N3 sleep may decrease in advancing age because of lesser EEG amplitudes resulting in sub-threshold, values that will not be scored during analysis. Due to this combination of factors, some elderly individuals may have significantly decreased N3 sleep, however, some degree will be due to lack of detection.
Questions & Answers
Overview
How has the AASM manual for sleep stage scoring evolved?
What is the role of cortical signals in sleep stage scoring?
What is the role of muscle signals in sleep stage scoring?
What is the role of eye movements in sleep state scoring?
What is the first step in sleep stage scoring?
What is included in general scoring of sleep stages?
How is stage W scored in sleep stage scoring?
How is stage N1 scored in sleep stage scoring?
How is stage N2 scored in sleep stage scoring?
How is stage N3 scored in sleep stage scoring?
How is stage R scored in sleep stage scoring?
What are arousals and how do they affect sleep stage scoring?
How do major body movements affect sleep stage scoring?
What is the role of normative sleep stage data in sleep stage scoring?
-
Electro-oculogram. During any eye movement, the cornea (positive) moves toward one electrode, while the fundus (negative) moves away from the same electrode. When the eye is not moving, the change in relative position is zero, and the eye leads do not record a signal. Conjugate eye movements thus cause out-of-phase EOG deflections.
-
Stage W. Alpha activity is present for greater than 50% of the epoch.
-
Stage N1. Alpha rhythm is attenuated and replaced by low-amplitude, mixed-frequency for more than 50% of the epoch.
-
Stage N2. Note K complexes unassociated with arousal and trains of sleep spindles.
-
Stage N3. There is slow wave activity in greater than 20% of the epoch.
-
Stage R. This demonstrates rapid eye movements, relatively low EMG tone, and low-voltage, mixed-frequency EEG activity.
-
Stage R. This demonstrates sawtooth waves.