Practice Essentials
As the name implies, brainstem gliomas occur in the region of the brain stem. Approximately 60% of the time they are centered within the pons, but can arise from the midbrain or medulla, and can infiltrate beyond the brainstem. They account for about 20% of all pediatric primary brain tumors, but constitute less than 2% of all adult gliomas.
Signs and symptoms
Common presenting signs and symptoms include the following:
-
Double vision
-
Weakness
-
Unsteady gait
-
Difficulty in swallowing
-
Dysarthria
-
Headache (most common presenting symptom in adults)
-
Drowsiness
-
Nausea
-
Vomiting
-
Behavioral changes or seizures in children (rare)
-
Deterioration of handwriting and speech, in older children
Common clinical findings on physical examination can be summarized as constituting a triad of cranial nerve deficits, long tract signs, and ataxia (of trunk and limbs). Papilledema may be seen. Sixth and seventh cranial nerves are involved commonly. Facial sensory loss and a primary-position, upbeating nystagmus may be seen. Crossed deficits (facial signs and symptoms contralateral to arm/leg signs and symptoms) are also characteristic of brainstem gliomas.
Certain manifestations suggest specific tumor locations, as follows:
-
Infants and children with failure to thrive – Pontine gliomas
-
Involvement of cranial nerve III or IV – A mesencephalic component
-
Hydrocephalus – Tumors in periaqueductal or fourth ventricle outflow locations
Patients with tectal lesions may present with the following:
-
Headache, nausea, and vomiting
-
Diplopia
-
Parinaud syndrome
Patients with cervicomedullary lesions may present with the following:
-
Dysphagia, unsteadiness, nasal speech, vomiting, and weakness
-
Sensory loss in the face (involvement of the trigeminal nucleus)
-
Dysphagia and/or dysphonia from lower cranial nerve involvement (commonly IX and X)
-
Long tract signs
-
Ataxia
-
Downbeating nystagmus and oculomyoclonus (medullary involvement)
See Clinical Presentation for more detail.
Diagnosis
The workup for brainstem gliomas may include the following:
-
MRI of the head – Diagnostic test of choice
-
CT scan – Less accurate than MRI, but appropriate when MRI is not available
-
CSF examination – Often used to evaluate for other diagnoses affecting the brainstem
-
Arteriography – Occasionally useful in differentiating vascular lesions, including tumors, from gliomas
Lab studies of blood chemistry and related body fluids are not helpful as a rule. Tissue confirmation is recommended, but sometimes not feasible.
See Workup for more detail.
Management
Treatment of brainstem gliomas may comprise the following:
-
Focal radiotherapy [1]
-
Chemotherapy
-
Surgical resection/biopsy
Observation alone may be considered for some adult patients with the following:
-
A tectal lesion
-
A cervicomedullary lesion
-
Mild symptoms of long duration
Focal radiotherapy
-
Remains the cornerstone of treatment for brainstem gliomas
-
Can improve or stabilize the patient's condition
-
Should be administered to any patient with significant and progressive neurologic symptoms
-
Conventional doses of radiotherapy ranges from 54 to 60 Gy
-
Reported survival rates with radiation therapy are better in patients with exophytic tumors
Chemotherapy
-
Chemotherapy with agents such as temozolomide may benefit some patients with high-grade histology (glioblastoma) [2]
-
Chemotherapy at relapse may benefit some patients
-
Chemotherapy may include conventional agents such as temozolomide and carboplatin/vincristine
-
Antiangiogenesis agents (eg, thalidomide, bevacizumab) have been used with success in supratentorial gliomas, but with variable success in brainstem gliomas
-
Patients should be encouraged to enroll in clinical trials (if available)
Surgical resection
Surgical therapy is performed in conjunction with radiation therapy, chemotherapy, or both. While it is not required for diagnosis or treatment of brainstem glioma, judicious use of biopsy/resection is recommended when safe. Surgery may improve symptomatic control and provide tissue for molecular testing for both prognosis and potential therapeutic implications. It should particularly be considered in the following situations:
-
Tumors of the cervicomedullary junction
-
Dorsal exophytic tumors protruding into the fourth ventricle
-
Cystic tumors
-
Enhancing tumors with clear margins that exert a space-occupying effect
-
Benign tumors (ie, those with slow clinical progression)
See Treatment and Medication for more detail.
Background
Brainstem gliomas are tumors that occur in the region of the brain referred to as the brain stem, which is the area between the aqueduct of Sylvius and the fourth ventricle. Although various systems are used to classify these tumors, many have divided brainstem gliomas into 3 distinct anatomic locations—diffuse intrinsic pontine, [3] tectal, and cervicomedullary. Intrinsic pontine gliomas carry a grave prognosis. Longer survival is associated with the tectal and cervicomedullary gliomas. Tumors also are characterized on the basis of site of origin, focality, direction and extent of tumor growth, degree of brainstem enlargement, degree of exophytic growth, and presence or absence of cysts, necrosis, hemorrhage, and hydrocephalus. [4]
Pathophysiology
Approximately 60% of brainstem gliomas are centered within the pons, but can originate in the medulla or midbrain and may extend beyond the brainstem. Brainstem gliomas are highly aggressive brain tumors. Anatomic location determines the pathophysiological manifestation of the tumor. With tectal lesions, hydrocephalus may occur as a result of fourth ventricular compression. With pontine and cervicomedullary lesions, cranial nerve or long tract signs are observed commonly.
Histopathologically, brainstem gliomas can range from WHO Grade 1 to 4. Grade 1 is classified as juvenile pilocytic astrocytoma, Grade 2 is diffuse astrocytoma, Grade 3 is anaplastic astrocytoma, and grade 4 is glioblastoma. The grading is based on the presence of nuclear atypia, vascular proliferation, mitoses, and necrosis. Typically, necrosis is seen in Grade 4 (glioblastoma multiforme). Increasing tumor grade is associated with poorer prognosis.
Molecular profiling is now an important part of glioma classification. An IDH1 mutation carries a significantly improved prognosis over the IDH1 wildtype, no matter the tumor grade. Codeletions of chromosome 1p and 19q along with an IDH1 mutation indicates an oligodendroglioma, and is rarely found in brainstem gliomas. For pediatric diffuse gliomas, a newly defined entity termed diffuse midline glioma, H3 K27M-mutant is characterized by K27M mutations in the histone H3 gene, a diffuse growth pattern and a midline location. This newly defined entity occurs primarilty in children, but can be seen in adults, and includes tumors previously referred to as diffuse intrinsic pontine glioma (DIPG). [5] MGMT promoter methylation has not been well studied in brainstem gliomas, however, one series suggested that more than 60% of brainstem gliomas are unmethylated. [6]
Mutations in the histone H3 gene suggest epigenetic dysregulation as an important contributor to the pathogenesis of diffuse intrinsic pontine glioma, particularly in children. Notably, histone H3 mutations rarely occur in adult patients with supratentorial glioblastoma.
Mortality/Morbidity
Morbidity from brainstem gliomas occur due to the location of the space-occupying lesion and compression of surrounding structures; because these structures regulate basic body functions of blood pressure, respiration, and swallowing as well as motor and sensory functions, compression can produce substantial neurological disability. Sudden death can result from increased intracranial pressure and subsequent cerebral herniation. This may be a consequence either of edema induced by the tumor or of hemorrhage into the neoplasm.
Pediatric diffuse intrinsic pontine glioma (DIPG) is associated with a dismal prognosis of approximately 10 months with only 10% of patients living > 2 years beyond initial diagnosis. However, median survival for adult patients with brainstem gliomas is in the range of 30–40 months. [2] Because presentation in adults varies widely, prognostication can be difficult. Other factors that have been shown to negatively influence survival include contrast enhancement within the tumor on MRI, location within the brainstem (pons > medulla > midbrain), and advanced age (> 60 years). [2, 7]
Epidemiology
Frequency
Brainstem gliomas represent < 2% of all intracranial tumors in adults and approximately 20% of brain tumors in children, with a slight male predominance. Median age at diagnosis in adults is in the mid-30s, but can present at any age. Brainstem gliomas are uncommon in adults and account for only 1%–2% of intracranial gliomas. [8]
Race-, sex-, and age-related demographics
CNS tumors vary in incidence by age, sex, ethnic group, and country, and also over time. How much of this variation is due to artifactual influences or etiologic differences has been the subject of many debates.
Some reports have suggested a slight male preponderance, whereas others have failed to observe any sex predilection.
Bimodal age distribution has been noted, with a peak incidence in the latter half of the first decade of life and a second peak in the fourth decade. Approximately three fourths of patients are younger than 20 years.
Prognosis
Pontine tumors are the most common variety of brainstem tumor. They also carry the worst prognosis; in children, the median survival duration is 9-12 months even with treatment. Kaplan et al reported a 37% survival rate at 1 year, 20% at 2 years, and 13% at 3 years, with a median survival of 10 months. Only 9 of 119 patients in their study were alive for more than 3 years after diagnosis. [9]
Squires et al, in a study of 12 children with midbrain tectal tumors, reported a median survival duration of more than 50 months. [10]
Favorable prognostic factors include (1) neurofibromatosis, (2) symptoms of at least 12 months' duration before diagnosis, (3) exophytic location, (4) pathology suggestive of low-grade tumor histology, (5) focal tectal and cervicomedullary tumors, and (6) calcification on CT scan.
Poor prognostic indicators include (1) age younger than 2 years, (2) multiple brainstem signs, (3) cranial nerve palsies, (4) diffuse intrinsic lesions of the pons, (5) short duration of signs and symptoms prior to the time of diagnosis, and (6) high-grade histology on tumor biopsy.
Hydrocephalus and tumor necrosis do not affect survival.
Race and gender do not affect survival.
The limited available data suggest that adults fare better than children with brainstem gliomas.
-
Grigsby et al reported a 10-year disease-free survival rate of 15.4% for adult patients with gliomas involving the midbrain, thalamus, or hypothalamus, and 29.6% for adults with pontine or medullary tumors. However, thalamic/hypothalamic neoplasms are not included historically in the classification of brainstem tumors. [11]
-
Landolfi et al studied 19 adults with brainstem gliomas, which included 13 diffuse intrinsic pontine, 4 cervicomedullary, and 2 tectal gliomas. They noted a trend that higher Karnofsky performance status conferred a better prognosis. Other factors did not affect survival. Median survival duration of patients in this study was 54 months, with a 5-year survival rate of 45%. [12]
-
Hamilton et al studied 16 adults with focal midbrain gliomas; they reported a median survival of 84 months. This indolent growth pattern is in marked contradistinction to the natural history of this disease in children. This is also the reverse of the usual behavior of hemispheric gliomas in which children typically fare better than older patients. [13]
-
Kesari et al reported on 101 adult patients with brainstem glioma. The overall survival for all patients at 5 and 10 years was 58% and 41%, respectively. The median survival was 85 months. They identified 4 factors that were significantly associated with survival in adults with brainstem gliomas. These factors included ethnicity, tumor location, age at diagnosis, and tumor grade. [14]
-
No explanation has been identified for the better outcome in adults; however, the possibility of prolonged survival with limited neurologic impairment must be recognized when counseling adults with brainstem gliomas.
Patient Education
Patients and families of patients acquire information from multiple sources, including, but not limited to, physician, patients, support groups, pharmaceutical companies, and the Internet. Physicians should be aware of this and have an open, informative relationship with their patients, empowering patients to become active members of the team with regard to the decision-making process involving their care.
-
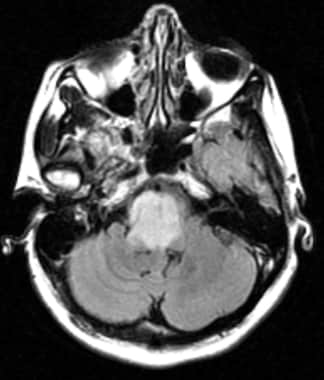
T2-weighted image of a diffuse intrinsic pontine glioma.
-
T2-weighted image of a right tectal glioma.
-
Axial T2 FLAIR MRI image showing a mass in the brainstem consistent with brainstem glioma.
-
Axial T2 FLAIR image showing a pontine-centered lesion consistent with a brainstem glioma.
-
Axial T2 image showing a pontine mass consistent with brainstem glioma.