Background
Peripheral neuropathy is common in many vasculitic syndromes and may be the only manifestation of the underlying vasculitic disease.
Vasculitic neuropathy can be a part of systemic vasculitis. It also can present as a nonsystemic vasculitic neuropathy, without any constitutional symptoms or serologic abnormalities. The clinical and pathologic features are those of an ischemic neuropathy caused by a necrotizing vasculitis of small arterioles. [1, 2]
Patients with vasculitic neuropathy may present with either mononeuritis multiplex or asymmetric sensorimotor neuropathy. Symmetric neuropathy is rare. It can present as acute/subacute relapsing, progressive, or relapsing progressive neuropathy.
Asymmetric or multifocal painful sensorimotor neuropathy is the most common presentation.
Asymmetry and length-independent involvement are the hallmarks of mononeuritis multiplex, which is the most common presenting feature of vasculitic neuropathy.
Peripheral neuropathy due to vasculitis without manifestations of disorders in other systems was first reported by Kernohan and Woltman in 1938. [3] In 1987, Dyck et al described characteristic features of 20 cases of vasculitic neuropathy with no or few clinical symptoms of systemic disease or serological abnormalities. They proposed the term of nonsystemic vasculitic neuropathy (NSVN). [4] In 1996, Davies et al reported 25 patients with vasculitis confined to peripheral nerves using the term isolated peripheral nervous system vasculitis (IPNSV). [5] A few reports describe patients with vasculitis selectively affecting the peripheral nervous system. [6, 7, 8, 9, 10, 11, 12] The largest study (48 patients) was reported by Collins et al in 2003. [13]
Pathophysiology
Wallerian degeneration of nerves results from ischemic infarction caused by inflammatory occlusion of the blood vessels. Segmental fibrinoid necrosis of a vessel wall and transmural inflammatory cell infiltration are the main pathologic features of vasculitis. Leukocytoclastic reaction traditionally has been considered the primary mechanism of vessel injury in these diseases, although more recent evidence suggests that cellular-mediated mechanisms may be more important in the peripheral nerve.
Immune complexes are formed as a result of antibodies reacting with antigen found within the blood vessel walls. These immune complexes within the circulation activate the complement cascade, generating chemotactic factors responsible for recruitment of polymorphonuclear leukocytes at the local site of deposition of the complex. Degranulation of the polymorphonuclear leukocytes releases proteolytic enzymes, which, along with free radicals, disrupt cell membranes and damage blood vessels. T cell–mediated processes against epineurial and endoneurial vessels likely are also important in the pathogenesis of vasculitic neuropathies.
Necrotizing vasculitis causes neuropathy through ischemic injury to the vessels supplying the nerve. Poor collateral circulation in the nerves makes them susceptible to ischemic injuries. Commonly involved nerves with these features tend to be in the mid upper arm and mid thigh in the "watershed zone."
Vasculitic neuropathy most often presents as mononeuropathy multiplex (ie, in more than 60% of patients), with the peroneal nerve most commonly affected (89% of patients), followed by the sural nerve (84%), tibial nerve (68%), ulnar nerve (42%), and median nerve (26%).
Distal symmetric polyneuropathy is the second most common presentation, seen in less than one third of patients. The nerves most often affected clinically are a diffuse mix of distal more than proximal lower limb nerves, arising either from the lumbosacral plexus or from widespread multifocal nerve involvement (ie, summation of existing patchy lesions).
Cranial nerve involvement also has been reported in systemic vasculitis. Facial nerve neuropathy is observed most commonly, occasionally accompanied by abnormalities in cranial nerve III, VI, or X.
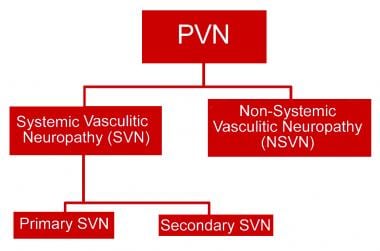
Diagnostic classification of peripheral vasculitic neuropathy
Systemic vasculitic neuropathy (85%) [14]
Primary systemic vasculitis (60%) [14]
Medium vessel:
-
Polyarteritis nodosa (17.9%)
Small vessel:
Secondary vasculitis (22%) [14]
Connective tissue disease (15%)
Infection-related (3%)
-
Hepatitis C – associated cryoglobulinemia
Paraneoplastic (3.5%)
Unclassified (5%) [14]
Nonsystemic vasculitic neuropathy 10–15% [14]
Epidemiology
Frequency
Peripheral neuropathy occurs in 60–70% of patients with some systemic vasculitic syndromes. Several reports have noted that approximately 34% of patients with vasculitis have disease restricted to the peripheral nervous system, termed nonsystemic vasculitic neuropathy. [3, 15, 4, 5, 13, 16]
Relapse rates observed in systemic vasculitides range from 11-60% [17] when all manifestations are included (neurologic and systemic). Relapse occurred almost exclusively in patients treated with prednisolone alone. Aggressive early treatment with cyclophosphamide may prevent relapse.
Peripheral nervous system involvement is an American College of Rheumatology (ACR) diagnostic criterion for polyarteritis nodosa and Churg-Strauss syndrome; it occurs in 50–78% of patients. [18, 19, 20, 21] The reported incidence of vasculitic peripheral neuropathy in primary vasculitides has varied from 20–80% [22] , reflecting the clinicopathological overlap between individual syndromes and associated nosological uncertainty.
Mortality/Morbidity
No controlled studies document mortality rate, but death generally is secondary to systemic complications of the vasculitis. Chance of recovery is better in nonsystemic vasculitic neuropathy, with good recovery for most patients.
Mathew et al found that 1-year survival was 90.3%, with death occurring predominantly in older patients with severe multisystem disease. [14]
Studies have shown that morbidity and mortality rates tend to be very high if the condition is untreated and systemic or if the condition is misdiagnosed.
In one study, final disability in those who survived more than 24 month was no sign or symptoms in 17%, mild-to-moderate disability in 65%, moderately severe disability in 13%, and severe disability in 4%. Chronic pain was persistent in more than 60% of patient in this study.
One cohort study showed a 5-year survival rate of 87%.
Race-, sex-, and age-related demographics
The racial distribution of vasculitic neuropathy is unknown.
Both genders are represented equally.
Mean age at presentation is 62 years.
Prognosis
Vasculitic neuropathy requires prompt diagnosis and treatment to promote good outcome. In patients whose neuropathy is part of a systemic vasculitis, the neuropathy can be expected to improve, leaving only mild or moderately severe functional disability. Nevertheless, the long-term outlook for such patients is poor, with a 5-year survival rate of approximately 50%; most excess deaths are due to vascular disease. The prognosis in nonsystemic vasculitic neuropathy is substantially better than in systemic vasculitis.
-
Diagnostic classification of peripheral vasculitic neuropathy (PVN).