Overview
Somatosensory evoked potentials (SEPs) are generated by stimulation of afferent peripheral nerve fibers by either physiological or electrical means. SEPs were first recorded more than 50 years ago. For an explanation of their physiologic and anatomic basis and description of techniques, see Somatosensory Evoked Potentials: General Principles. In this article, the focus is on the clinical applications of SEPs.
SEPs can be recorded after physiological stimuli (eg, muscle stretch). However, electrical stimulation usually is administered to elicit the potential. Typically, a square wave of 0.2- to 2-millisecond duration is delivered to a peripheral nerve by electrodes, usually surface electrodes. For intraoperative monitoring, needle electrodes are used for stimulation since they require smaller currents, which reduce the stimulus artifact. The usual sites for SEP stimulation are the median nerve at the wrist, the common peroneal nerve at the knee, and the posterior tibial nerve. [1] A SEP also may be recorded by stimulating the skin in various dermatomal areas, but the response is much weaker.
In mixed peripheral nerves, the threshold for sensory perception is lower than the threshold to elicit movement. For stimulation of mixed peripheral nerves, the stimulating current is adjusted to produce a minimal movement of the joint involved. This stimulation intensity typically is well tolerated by patients. Recording electrodes are placed on the scalp and over the cervical spine. For recording upper extremity SEPs, electrodes are placed over the Erb point. For recording lower extremity SEPs, electrodes are placed over the lumbosacral spine.
Waveforms are described in terms of morphology, amplitude, and dispersion. Each laboratory should establish reference values for latencies and interpeak latencies that are based on a patient's age and height. Because limb cooling affects peripheral nerve conduction velocity, minimum skin temperature norms should be established for each laboratory.
Responses recorded are classified according to specific latencies. Short-latency SEPs refer to the portion of the SEP waveform that occurs within 25 milliseconds after stimulation of the upper extremity nerves, 40 milliseconds after stimulation of the peroneal nerve, or 50 milliseconds after stimulation of the tibial nerve. Long-latency SEPs refer to the waveforms recorded more than 100 milliseconds following stimulation of these nerves. Middle-latency SEP refers to waveforms that occur between these 2 periods.
Mixed nerve stimulation has become the standard for clinical use. Other methods include cutaneous nerve stimulation, dermatomal stimulation (which is more specific than cutaneous nerve stimulation), motor point stimulation, and paraspinal stimulation.
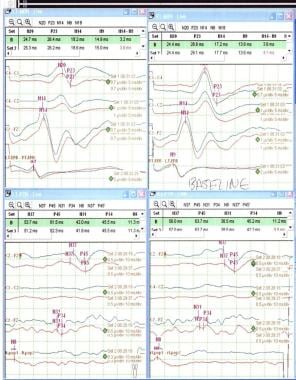 Normal baseline SEPs. Left median on upper left corner, right median on upper right corner, left tibial on lower left corner and right tibial on lower right corner.
Normal baseline SEPs. Left median on upper left corner, right median on upper right corner, left tibial on lower left corner and right tibial on lower right corner.
 Effects of reduced temperatures from 36º to 34.5º, resulting in increase in latency throughout evoked potentials from N9-P20.
Effects of reduced temperatures from 36º to 34.5º, resulting in increase in latency throughout evoked potentials from N9-P20.
Animal studies
Madhok et al concluded that in the absence of brain injury in a rodent model, hypothermia induces significant increases to the SEP amplitude while increasing SEP latency. [2] Hypothermia also suppressed EEGs at different regions of the brain by different degrees. The changes to SEPs and EEG are both reversible with subsequent rewarming.
Clinical Interpretation
The SEP stimulus preferentially excites only the largest myelinated fibers in the peripheral nerve. These include cutaneous and subcutaneous fibers, somesthetic and proprioceptive fibers, and motor axons of equivalent diameter. The stimulus activates predominantly the large-diameter, fast-conducting group in muscles and group II cutaneous fibers. Stimulation produces an action potential that travels up the axon toward the spinal cord and past the cell bodies of the sensory axons of the large-fiber sensory system in the dorsal root ganglia to the ipsilateral posterior columns of the spinal cord. These signals then traverse a synapse in the dorsal column nuclei at the cervicomedullary junction.
The signals travel in second-order neurons to the ventroposterolateral nucleus of the thalamus (VPL) via the medial lemniscus. In the VPL, a synapse is made with a third-order neuron that travels to area 3b of the parietal sensory cortex. SEPs provide information concerning the integrity of the pathway through the brain, brain stem, spinal cord, dorsal roots, and peripheral nerves.
Although SEPs may reveal or localize a lesion involving the somatosensory pathways, they should be interpreted as extended neurologic examination. They do not indicate the underlying disease process and normal findings do not exclude an organic basis for symptoms. Despite these limitations, SEP studies may be helpful diagnostically as well as prognostically to determine the extent of pathologic involvement in different disorders.
Clinical Uses
Clinical uses of SEPs include the following:
-
Evaluation of the peripheral nervous system and the large-fiber sensory tracts in the CNS
-
Localization of the anatomic site of somatosensory pathway lesions [3]
-
Identification of impaired conduction caused by axonal loss or demyelination
-
Confirmation of a nonorganic cause of sensory loss
Although SEP findings are not disease specific, they can confirm afferent conduction impairment associated with certain disorders.
Other disorders
SEPs have been used to confirm the presence of normal conduction pathways in patients with conversion disorder, malingering, or other psychological disturbances. Findings must be interpreted carefully, because normal SEPs can be seen in patients with organic sensory loss. For example, some patients with pure sensory strokes due to lacunar infarcts may have normal SEPs.
Peripheral Nervous System
SEPs may be used in evaluation of the peripheral nervous system when traditional nerve conduction studies (NCSs) are not possible (for any reason) or are not reliable (eg, technical problems, or artifacts).
Peripheral neuropathy
SEPs are rarely used to assess peripheral neuropathy since standard NCSs are the test of choice. The stimulation is applied at 2 or more sites and the responses are recorded over the scalp. In the presence of polyneuropathies and mononeuropathies, SEP waveforms recorded over the scalp may be absent or show delayed latencies with normal central conduction velocities. In this way, SEPs can be used to measure the afferent fiber conduction velocities of proximal segments. Higher stimulation currents are typically required in patients with peripheral neuropathies.
SSEP studies disclosed poorly formed and delayed cortical potentials with absent lumbar (N20) potentials, thereby suggesting the presence of proximal demyelination. SSEPs were normal in the patients with pure motor CIDP and multifocal motor neuropathy (MMN) and can thus help differentiate asymmetric forms of CIDP from MMN. These findings suggest that SSEPs may be an important complementary investigation to conventional NCSs in the diagnosis of chronic acquired demyelinating polyneuropathies (CADP).
Use of SEPs has been reported for the following peripheral nerve disorders:
-
Hereditary neuropathies (eg, Charcot-Marie-Tooth disease, Friedreich ataxia)
-
Inflammatory polyradiculopathies, such as Guillain-Barré syndrome, particularly early in the course of the disease, when distal conduction and F-wave studies may be normal
-
Chronic acquired demyelinating neuropathies
-
Infectious causes (eg, HIV)
-
Toxic neuropathies
Focal neuropathy
The test of choice in focal neuropathy is standard NCSs. Entrapment neuropathies, such as carpal tunnel syndrome, may be found incidentally when SEPs are recorded. The use of SEP for detection of saphenous neuropathy, intercostal neuropathy, and trigeminal neuropathy has been reported. However, standard NCSs are the preferred diagnostic test for these conditions.
Plexopathy
SEPs are useful for evaluation of brachial plexopathy and traumatic plexopathies. [4] In thoracic outlet syndrome, SEPs are of limited value with regard to the neurogenic variety of plexopathy and have no established value in diagnosis of the nonneurogenic (ie, vascular) variety. The value of SEPs in preventing or minimizing intraoperative damage of the peripheral nervous system is unproven.
Ventral rootlets and roots
Studies suggest that SEPs may have some use in the evaluation of rootlet and root dysfunction. However, needle electromyography (EMG) provides superior information in these disorders and remains the test of choice.
Lumbosacral root disease
SEPs may have some utility in the evaluation of acute lumbosacral root disease or in lumbosacral spinal stenosis.
Thoracic root disease
No data are available.
Cervical root disease
EMG is the best neurophysiological tool for evaluation of this condition. SEPs may or may not have a limited role in these conditions.
Spinal Cord
Trauma
Scalp-recorded potentials are absent in complete lesions of the cervical spinal cord. However, incomplete lesions yield varying abnormalities on SEPs. SEPs can help localize the sensory level in trauma and also may help in determining prognosis for functional outcome. Latencies and amplitudes of tibial SSEPs can change over time after spinal cord injury (SCI). The early recordability of a tibial SSEP is associated with a favorable functional and neurological status and outcome after SCI.
Surgical monitoring
SEP monitoring is used widely to assess integrity of the spinal cord during surgery in which the spinal cord is manipulated. SEPs are used most often during scoliosis correction. Ischemia of ascending somatosensory pathways produces a drop in amplitude or loss of waveforms, thus warning the surgeon in time to take corrective action. Ischemic changes are usually widespread; rarely, motor function is lost when somatosensory pathways have not been affected.
The use of intraoperative neuromonitoring, especially SSEPs, MEPs and EMGs, during pediatric scoliosis repair has become commonplace to reduce the risk of potentially devastating postoperative neurologic deficits. [5]
The increased amplitude, particularly in cortical SSEPs (N20/P25), detected specifically during steady-state hypothermia seems to support the clinical use in monitoring the brain function; this is not only during cardiac surgery with cardiopulmonary bypass but also in other settings, such as therapeutic hypothermia procedures in an ICU. [6]
Other spinal procedures in which SEP monitoring is used include reduction of vertebral fractures and other vertebral injuries and spinal cord tumor surgery. Conduction abnormalities that selectively abolish the silent periods can distinguish between hydromyelia (a physiologically dilated central canal) and space-occupying syringomyelia.
Researchers evaluated the diagnostic accuracy of SSEP monitoring during scoliosis fusion and found SSEP to be a highly sensitive and specific test. Data also showed that iatrogenic spinal cord injury resulting in new neurological deficits was 340 times more likely to have changes in SSEP compared to those without any new deficits. [7]
Conditions for which SEPs might be useful
See the list below:
-
Subacute combined degeneration
-
Cervical spondylosis and myelopathy
-
Syringomyelia, to evaluate the effect of spinal cord compression
-
Hereditary spastic paraplegia
-
Transverse myelitis
-
Multiple sclerosis - Lower-limb SEPs produce a higher yield for detecting abnormalities
-
Vascular lesions
-
Tumors
-
Myelomeningocele
-
Tethered cord syndrome
-
Infectious disorders (eg, human T-lymphocytic virus 1 and HIV)
Brain Stem and Brain
Brain stem lesions and stroke
SEPs are normal in Wallenberg's syndrome but are generally abnormal when medial lemniscus is involved. SEPs are also unaffected and normal in some of the hemispheric (eg, pure motor lacunar infarctions, occipital lobe infarctions). In larger brainstem or hemispheric lesions, N20 and later waveforms may be delayed or absent. In lesions of the thalamocortical radiations, dissociation between the N20 and P22 waveform amplitudes may be observed. Changes in SEPs over time have been explored for their predictive value for recovery from stroke. This area remains investigational.
Multiple sclerosis
SEPs of the upper extremities are abnormal in about 60% of all patients with MS (definite, probable, and possible) and in about 40% of patients with asymptomatic MS. SEPs of the lower extremities have a higher frequency of abnormality, presumably since longer axons are more likely to have an area of demyelination. In clinical practice, SEPs of both the upper and lower extremities usually are performed. The change most frequently seen in MS is prolongation of central latencies. MRI has largely supplanted SEP testing in MS.
Other demyelinating diseases
Abnormalities in SEPs are seen in adrenoleukodystrophy, adrenomyeloneuropathy, metachromatic leukodystrophy, heterozygotes for adrenoleukodystrophy and adrenomyeloneuropathy.
Coma
SEPs are useful in the evaluation of a comatose patient, not only for diagnostic purposes but also for prognosis. In addition to EEG, other neuromonitoring tools, such as SEPs, have a complementary role, surveying the integrity of the neuroaxis as an indicator of prognosis or illness progression in both acute brain and spinal injuries. [8] Central conduction times are not affected significantly by level of consciousness, hypothermia, or sedative-hypnotic medications such as barbiturate anesthesia. Thus, SEPs are often useful in conditions in which clinical examination is of limited value. A favorable outcome is expected in about 53% of comatose patients with hypoxic-ischemic encephalopathy and in 49% of patients with traumatic brain injury coma who have preservation of bilateral cortical SEP responses.
Rothstein has shown that median SEPs supplement and enhance neurologic examination findings in anoxic-ischemic coma and are useful as an early guide in predicting outcome. Greater use of SSEP in anoxic-ischemic coma has been recommended to identify those patients unlikely to recover and can be cost effective. [9] A pilot study done by Bouwes et al has revealed that bilaterally absent cortical N20 responses of median nerve SEPs performed during mild hypothermia after resuscitation can predict a poor neurologic outcome. A larger multicenter prospective cohort study to confirm these results is in progress by the same authors. [10]
The absence of cortical responses bilaterally is associated with an unfavorable prognosis (ie, an outcome of persistent vegetative state in the vast majority of patients). Unilateral preservation of cortical SEP responses offers hope for a favorable outcome. Determination of presence or absence of the N70 in patients with postanoxic coma gives additional information about the likelihood of poor outcome, but it is not precise enough to base treatment decisions solely on its absence.
Combination of clinical examination, electroencephalography reactivity, and serum neuron-specific enolase offers the best outcome predictive performance for prognostication of early postanoxic coma; somatosensory-evoked potentials do not add any complementary information. Although prognostication of poor outcome seems excellent, future studies are needed to further improve prediction of good prognosis, which still remains inaccurate. [11]
Subarachnoid hemorrhage
Wachter et al recently studied the use of multimodal electrophysiological monitoring to predict the outcome after subarachnoid hemorrhage (SAH). [12] They could not find a correlation between initial and last median, as well as tibial, SEP. Therefore, they concluded that these studies cannot be used as valid predictors for outcome after SAH. [13]
Brain death
In brain death, peripheral SEP components are preserved. However, potentials generated by structures above the lower medulla are absent.
Traumatic brain injury
A study by Bosco et al examined prognostic value of SSEPs and CT scan evaluation in acute traumatic brain injury. The study revealed a highly significant improvement in outcome prediction when the model included a pool of amplitudes and latencies, referred to different early-evoked components pN20, pP25, fP20,cP22, N30, P45, and N60, associated to CT scan hypodensity values, compared with the use of the cortical parietal N20/P25 alone. [14]
Surgical Monitoring Techniques
Intraoperative SEPs are recorded routinely using electrode strips or grids or electrodes applied directly to the exposed cortex during neurosurgical procedures in and around the somatosensory cortex. The N20 response is used to identify the primary somatosensory cortex in the postcentral gyrus. By inference, the motor cortex in the precentral gyrus can be localized as well, and this information is used to guide the surgical procedure. Scalp-recorded SEPs have also been used to monitor cerebral ischemia during vascular surgery, such as carotid endarterectomy; however, EEG monitoring is used more widely for this application. The value of regional cerebral oximetry adds nothing to the information already provided by EEG and SEP in determining when to place a shunt during CEA.
Somatosensory response can be measured by magnetoencephalography (see images below). The generators of the N20m and later waveforms can be modeled as equivalent current dipoles. Usually, individual digits and the lip are stimulated, and the single dipoles of the cortical generators are overlaid on co-registered MRIs to create a map of the somatosensory cortex. SEPs are usually collected in outpatients several days prior to the surgery so that the information can be used by neurosurgeons to help in planning the approach to the anticipated surgery. The information also can be used to provide patients with an idea of the relative risk of neurologic deficits that could result from the surgery.
 Plot of 148-channel magnetoencephalographic recording of somatosensory evoked response to tapping on the tip of the left fifth digit. As magnetic fields enter and exit the skull at different locations, the deflections are upgoing at some magnetometer channels and downgoing at other magnetometer positions. The N20m latency is highlighted.
Plot of 148-channel magnetoencephalographic recording of somatosensory evoked response to tapping on the tip of the left fifth digit. As magnetic fields enter and exit the skull at different locations, the deflections are upgoing at some magnetometer channels and downgoing at other magnetometer positions. The N20m latency is highlighted.
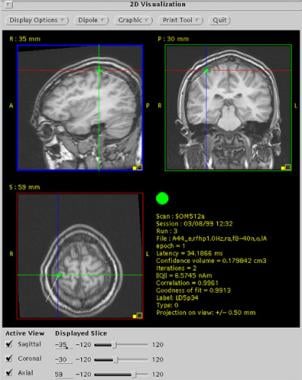
 First cortical somatosensory response (N20m) to left fifth digit stimulation recorded by magnetoencephalography. Localization of the response is co-registered on the patient's MRI. Note that the response localizes to the postcentral gyrus.
First cortical somatosensory response (N20m) to left fifth digit stimulation recorded by magnetoencephalography. Localization of the response is co-registered on the patient's MRI. Note that the response localizes to the postcentral gyrus.
Use of motor evoked potentials (MEP) and SEP monitoring during thoracic and thoracoabdominal aortic surgery is controversial. Motor and somatosensory evoked potentials during thoracic and thoracoabdominal aortic aneurysm repair were analyzed. Irreversible changes were significantly associated with immediate neurologic deficit, and the findings were identical for SEP and MEP in this variable, indicating that the more complex MEP measures do not add further information to that obtained from SEP. Normal SEP and MEP findings had a strong negative predictive value, indicating that patients without signal loss are unlikely to awake with neurologic deficit.
Combined neurophysiological intraoperative monitoring with EMG and SEP recording and the selective use of MEPs is helpful for predicting and possibly preventing neurologic injury during cervical spine surgery.
Intraoperative SEP monitoring was reliable in ruling out spinal injury in descending thoracic and thoracoabdominal aortic repair, but had a low sensitivity. It did not predict delayed neurologic deficit. Spinal SEP change was an independent predictor of mortality and correlated with low preoperative glomerular filtration rate. Effects of various anesthetics used during surgical monitoring need to be kept in mind. Sloan et al have shown drug synergy when isoflurane is mixed with nitrous oxide. If these agents are used for anesthesia, the combination of these agents may produce more amplitude and latency changes than expected from individual agents. [15]
Eager et al emphasized the importance of the use of multimodality methods, including the use of SEPs in spine cases based upon their study of 2069 cases. [16]
Degenerative Disorders
In Friedreich ataxia, SEPs recorded from the scalp usually show normal peripheral nerve conduction latencies but prolonged central conduction times. Degenerative disorders of the brain stem, such as spinal cerebellar degeneration, usually show a similar SEP pattern. In Huntington disease, latencies are normal but the amplitudes may be low (similar to the low-voltage pattern found in the EEG).
SEPs are normal in many degenerative disorders, including Parkinson disease, [17] Alzheimer disease, and amyotrophic lateral sclerosis (particularly early in the course of the disease). [18] An unusually large amplitude response is seen in the SEPs of patients with progressive myoclonic epilepsy. In cerebrovascular disease or head trauma, abnormal SEPs are recorded when infarction, hemorrhage, or direct injury disrupts the integrity of ascending somatosensory pathways.
Questions & Answers
Overview
What are somatosensory evoked potentials (SEPs)?
What is the clinical interpretation of somatosensory evoked potentials (SEPs)?
What are the clinical uses of somatosensory evoked potentials (SEPs)?
Which peripheral nerve disorders can be assessed by somatosensory evoked potentials (SEPs)?
What is the role of somatosensory evoked potentials (SEPs) in the evaluation of focal neuropathy?
What is the role of somatosensory evoked potentials (SEPs) in the evaluation of plexopathy?
Which spinal cord conditions can be assessed by somatosensory evoked potentials (SEPs)?
What is the role of somatosensory evoked potentials (SEPs) in the evaluation of multiple sclerosis?
Which demyelinating diseases can be assessed by somatosensory evoked potentials (SEPs)?
What is the role of somatosensory evoked potentials (SEPs) in the evaluation of a comatose patient?
What is the role of somatosensory evoked potentials (SEPs) in the evaluation of brain death?
What is the role of somatosensory evoked potentials (SEPs) in intraoperative monitoring?
Which degenerative disorders can be assessed by somatosensory evoked potentials (SEPs)?
-
Plot of 148-channel magnetoencephalographic recording of somatosensory evoked response to tapping on the tip of the left fifth digit. As magnetic fields enter and exit the skull at different locations, the deflections are upgoing at some magnetometer channels and downgoing at other magnetometer positions. The N20m latency is highlighted.
-
First cortical somatosensory response (N20m) to left fifth digit stimulation recorded by magnetoencephalography. Localization of the response is co-registered on the patient's MRI. Note that the response localizes to the postcentral gyrus.
-
The P34m response to tapping on the tip of the left fifth digit as seen on magnetoencephalography.
-
Localization of the P34m response co-registered onto the patient's MRI.
-
Normal baseline SEPs. Left median on upper left corner, right median on upper right corner, left tibial on lower left corner and right tibial on lower right corner.
-
Effects of reduced temperatures from 36º to 34.5º, resulting in increase in latency throughout evoked potentials from N9-P20.