Practice Essentials
Raeder paratrigeminal syndrome (ie, paratrigeminal neuralgia) is characterized by severe, unilateral facial pain and headache in the distribution of the ophthalmic division of the trigeminal nerve in combination with ipsilateral oculosympathetic palsy or Horner syndrome.
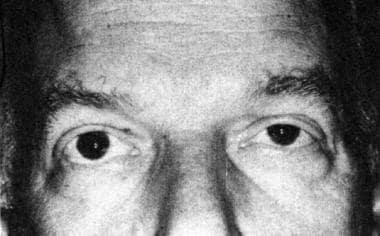 Evident in this patient are the mild ptosis of the left upper eyelid, the slight elevation of the left lower eyelid, and the miosis of the left eye. Reprinted with permission (Copyright American Society of Contemporary Ophthalmology. Annals of Ophthalmology 1978; 10(9); 1181-1187.)
Evident in this patient are the mild ptosis of the left upper eyelid, the slight elevation of the left lower eyelid, and the miosis of the left eye. Reprinted with permission (Copyright American Society of Contemporary Ophthalmology. Annals of Ophthalmology 1978; 10(9); 1181-1187.)
Signs and symptoms
History for Raeder paratrigeminal syndrome suggests trigeminal nerve involvement with pain, sensory or motor deficits, and/or ipsilateral oculosympathetic paresis. It resembles Horner syndrome and manifests as oculosympathetic paresis with ptosis and miosis.
The pain associated with Raeder syndrome is deep and boring and is localized in or around the eye. Intermittent, lancinating pain also may occur. Typically self-limited, the pain usually remits in 2-3 months. [17]
Diagnosis
Because painful Horner syndrome can occur with other diseases, such as cluster headache and carotid dissection or aneurysm, a diagnosis of Raeder paratrigeminal syndrome should be made on clinical and radiologic grounds.
Management
Unless intracranial pathology exists, treatment of Raeder paratrigeminal syndrome remains predominantly symptomatic. Avoidance of vasodilators and alcohol is recommended due to the potential for exacerbation of pain.
When parasellar involvement is absent, steroids (either oral or intravenous) may be beneficial.
Background
Raeder paratrigeminal syndrome (ie, paratrigeminal neuralgia) is characterized by severe, unilateral facial pain and headache in the distribution of the ophthalmic division of the trigeminal nerve in combination with ipsilateral oculosympathetic palsy or Horner syndrome. (See Etiology and Pathophysiology and Presentation.)
The first patient described by Raeder, in 1918, had an incomplete Horner syndrome with preserved sweating on the side of the lesion. Raeder originally described absent facial anhidrosis in the paratrigeminal syndrome, although the literature suggests no definite consensus concerning the facial sweating pattern.
Subtypes (Boniuk and Schlezinger)
In 1962, Boniuk and Schlezinger described 2 subtypes of Raeder paratrigeminal syndrome. [1] Group I included patients with neuralgia, oculosympathetic paralysis, and parasellar nerve involvement. The responsible lesions were believed to be localized to the middle cranial fossa, requiring an extensive workup (eg, local or metastatic tumors).
In group II patients, the condition occurred without parasellar involvement but was associated with oculosympathetic paralysis and neuralgia. These cases were felt to be more benign than those of group I.
Some causative conditions in group II included migraine, cluster headache, hypertension, trauma, inflammatory disease, sinusitis, syphilitic osteitis, herpes zoster, otitis, and pneumonitis.
Subcranial aneurysms also have been described as a cause in either subtype. [2] A rare cause includes carotid dissection and should be considered early in the differential diagnosis of Raeder syndrome. [3]
Subtypes (Grimson and Thompson)
Grimson and Thompson described 3 major groups in 1980. [4] While those in group I were felt to require an extensive evaluation, those in the 2 latter groups were felt to have a more benign prognosis. However, obtain a thorough evaluation as indicated, regardless of the subtype, the 3 of which are characterized as follows (see Etiology and Pathophysiology and Presentation):
-
Group I - Includes patients with multiple parasellar cranial involvement or involvement of any or all divisions of the trigeminal nerve
-
Group II - Includes patients with cluster headache with an isolated oculosympathetic paresis
-
Group III - Includes patients with pain atypical for cluster headache, with involvement of the ophthalmic division of the trigeminal nerve
An additional variant
In 1978, 6 patients were described and 31 similar patients reviewed whose symptoms were consistent with a pericarotid syndrome. [5] These patients' conditions were characterized by oculosympathetic paralysis, ipsilateral head pain, and anhidrosis with otherwise intact facial sweating.
In these cases, the site of the lesion of the oculosympathetic fibers was believed to be pericarotid rather than paratrigeminal in distribution.
The syndrome thus was renamed in the absence of intracranial disease. These patients constitute a unique clinical group with findings similar to Raeder syndrome that can be localized to an area in and around the internal carotid artery and affected by diverse pathologic processes.
Etiology and Pathophysiology
Raeder felt that the syndrome was due to a limited space-occupying lesion in the paratrigeminal area of the middle cranial fossa.
Benign forms of Raeder syndrome without paratrigeminal cranial nerve involvement have also been reported. [6] One such case later evolved into an indomethacin-responsive hemicranial headache that fulfilled the diagnostic criteria for hemicrania continua. [7]
The pathophysiologic site of the painful oculosympathetic palsy involves the location at which oculosympathetic fibers exit the internal carotid artery to join the ophthalmic division of the trigeminal nerve. Various combinations of cranial deficiencies (nerves II-VI) also may be involved.
According to Goadsby, paratrigeminal oculosympathetic syndrome may be a more accurate name than Raeder paratrigeminal syndrome, because an analysis of the anatomy of the oculosympathetic innervation may place the lesion best in the middle cranial fossa, medial to the trigeminal ganglion. [8]
Raeder syndrome localizes to lesions of the middle cranial fossa involving oculopupillary sympathetic fibers originating from the internal carotid artery plexus and traveling with the trigeminal and oculomotor nerves. [9] Therefore, careful imaging of this area is highly recommended.
Sweating is preserved in Raeder paratrigeminal syndrome, in contrast to Horner syndrome, since some third-order sympathetic fibers are spared (see the image below). These particular fibers travel with the external carotid artery and its branches and are involved in the production of facial sweating. The clinical localization is therefore distal to the carotid bifurcation. If additional parasellar cranial nerves are involved, the lesion may localize more specifically to the middle cranial fossa. [10]
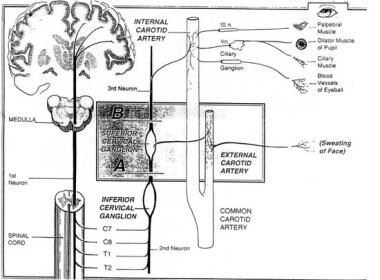 Cervical sympathetic pathway, including oculosympathetic fibers. A lesion at A would produce a complete Horner syndrome with ipsilateral loss of facial sweating; a lesion at B would produce oculosympathetic paresis, but with preserved facial sweating. Reprinted with permission (Hanley and Belfus, Inc. Academic Emergency Medicine 1996; 3(9); 864-867.)
Cervical sympathetic pathway, including oculosympathetic fibers. A lesion at A would produce a complete Horner syndrome with ipsilateral loss of facial sweating; a lesion at B would produce oculosympathetic paresis, but with preserved facial sweating. Reprinted with permission (Hanley and Belfus, Inc. Academic Emergency Medicine 1996; 3(9); 864-867.)
Associated morbidities
Raeder syndrome has been associated with several conditions, including the following:
-
Head trauma
-
Hypertension [11]
-
Vasculitis
-
Migraine headaches
-
Parasellar mass lesions
-
Internal carotid artery dissection or aneurysm
Prognosis
Symptomatic resolution in Raeder paratrigeminal syndrome usually occurs within an interval of 2-3 months. If pain persists or if atypical features are noted, investigate and manage secondary causes.
Morbidity and mortality
As previously mentioned, Raeder syndrome has been associated with several conditions, including head trauma, hypertension, vasculitis, migraine headaches, parasellar mass lesions, and internal carotid artery dissection or aneurysm. [12] Therefore, the morbidity and mortality depend on the underlying etiology, and the diagnosis of the condition warrants a full evaluation to identify an underlying cause.
Epidemiology
Raeder paratrigeminal neuralgia is a rare syndrome. The exact incidence of this disorder in the United States is unknown. [10] It is less common than Horner syndrome.
Raeder paratrigeminal syndrome seems to occur almost exclusively in males. Case reports vary as to the age of onset or diagnosis. The original case reports from Raeder involved patients aged 18–65 years. However, onset appears most prevalent in middle or old age.
Case Reports
A case report in Headache detailed a 27-year-old man presenting with headache, blurred vision, and dizziness that was attributed to lyme disease. [13] The patient was treated with antibiotics with improvement of symptoms. This case illustrates that lyme disease should be considered in patients who may present with Raeder's when no other cause is found.
Raeder syndrome can also present with other disease states in the head or neck region. A case of bacterial sinusitis has been reported in the literature, [14] and while less common, it should be considered in the differential diagnosis.
A case of carotid artery invasion by a malignancy of unknown primary was described in a patient presenting with unilateral headache and incomplete Horner's syndrome in the absence of anhidrosis. [15] Compressive lymphadenopathy affecting the carotid system and creating sympathetic dysfunction was felt to be the underlying mechanism.
Another report details the case of a 52-year-old woman presenting with V1 distribution pain and ptosis and photobia of the left eye. Multiple cranial neuropathies including 2, 3, 5, and 6 were seen and the headache became chronic with exacerbations of autonomic symptoms and a subsequent diagnosis of hemicrania continua was made. This case illustrates a rare presentation of Raeder syndrome evolving into hemicrania continua, treated with oral prednisone and onabotulinumtoxin A. [16]
-
Cervical sympathetic pathway, including oculosympathetic fibers. A lesion at A would produce a complete Horner syndrome with ipsilateral loss of facial sweating; a lesion at B would produce oculosympathetic paresis, but with preserved facial sweating. Reprinted with permission (Hanley and Belfus, Inc. Academic Emergency Medicine 1996; 3(9); 864-867.)
-
Evident in this patient are the mild ptosis of the left upper eyelid, the slight elevation of the left lower eyelid, and the miosis of the left eye. Reprinted with permission (Copyright American Society of Contemporary Ophthalmology. Annals of Ophthalmology 1978; 10(9); 1181-1187.)







