Infective Endocarditis and the CNS
Endocarditis can have profound and devastating neurologic consequences. [1, 2] The incidence of central nervous system (CNS) complications in infective endocarditis is approximately 30% and these manifestations are often the first sign of illness (47% of the time in one series).
In most cases, the neurologic sequelae are present before the initiation of antimicrobial therapy (76%). Even amnesia can herald a diagnosis of infective endocarditis.
The Massachusetts General Hospital experience from 1964-1973 yielded 218 patients with bacterial endocarditis, 84 of whom had neurologic complications (38%). [3]
Another series (133 patients) demonstrated a similar proportion (41%) of patients with infective endocarditis with neurologic problems. [4]
Etiology of CNS Sequelae
The incidence of CNS complications in infective endocarditis varies by organism (Staphylococcus species, 54%; Enterococcus species or Streptococcus viridans, ≥19%) and by location (mitral valve with Staphylococcus aureus, 87%).
The risk of CNS embolization also varies according to the location of the endocarditis, with mitral valve endocarditis carrying a higher risk of CNS embolization than does aortic valve involvement (17% vs 9% for mitral valve endocarditis and aortic valve endocarditis, respectively). [5] (Mental status changes in infective endocarditis, without focal findings, have been attributed to microemboli [11% in the Massachusetts General Hospital series]. [3] )
Differences in opinion remain as to whether patients with native valve endocarditis (NVE) or prosthetic valve endocarditis (PVE) are at greater risk for neurologic complications.
Staphylococcus species classically lead to embolization earlier than do other organisms (ie, < 2 wk) and often cause hemorrhage within the first 48 hours or even prior to other symptomatic presentation. S viridans subacute bacterial endocarditis (SBE) is more indolent, usually with a clinical course of 1-3 months.
Partially treated bacterial endocarditis usually has a slower time course as well. Pseudomonas species and other coliform bacteria, including Haemophilus influenzae and group B streptococci, produce large vegetations. Aspergillus and Candida species endocarditis also have a high incidence of embolic phenomena as a result of large valvular vegetations.
Stroke
A 0.5% risk of stroke occurrence per day exists in patients with infective endocarditis. Strokes in these patients can be subtle or even subclinical.
One series showed that in patients with infective endocarditis who had CNS involvement, four fifths had ischemic strokes and one fifth had hemorrhages, which is a distribution similar to that of strokes in general.
Approximately 15-50% of the CNS manifestations of infective endocarditis are due to embolic occlusion and/or stroke.
In 1965, McDevitt reported that SBE accounted for 3% of all cerebral emboli. A later study showed that there was CNS involvement in 71% of all embolic events in patients with infective endocarditis.
The rate of major embolic events was 17% in one series (reported range, 6-31%). Of 38 events in 37 patients, 34 involved the middle cerebral artery (MCA) or its branches.
If stroke recurs, it usually indicates that the infection is not controlled or has recurred. Embolization occurring greater than 2 months after presentation is uncommon.
One series showed 23 patients with multiple microscopic infarcts at autopsy that had been clinically silent. Microorganisms rarely were confirmed in the emboli.
Approximately one half of patients with cerebral emboli also have systemic emboli.
Infectious aneurysms
Aneurysms of arteries supplying the brain make up approximately 15% of the aneurysms occurring in infective endocarditis.
Osler coined the term “mycotic aneurysm” to describe a mushroom-shaped aneurysm associated with SBE. Originally referring to any infectious etiology, mycotic aneurysm still is used as a general term and is not specific for fungal etiology. Mycotic aneurysms occur in as many as 15% of patients with infective endocarditis.
The incidence of clinically diagnosed intracranial mycotic aneurysms in patients with infective endocarditis is approximately 2% (compared with a 5-10% prevalence postmortem, as determined at autopsy). Mycotic aneurysms involve the MCA territory 4 times more often than they do the anterior or posterior cerebral arteries. In contrast to berry aneurysms, which occur in or near the circle of Willis, mycotic aneurysms occur at secondary branches and bifurcations, usually in the lateral fissure near the trifurcation of the MCA.
When aneurysms form, the most likely mechanism is bacterially induced weakening (originating from the adventitial side of the vessel wall and apparently after organisms traverse the vasa vasorum). According to animal studies, the pathology is not via direct endoluminal damage to the intima.
Controversy exists as to whether the more virulent organisms are associated more commonly with aneurysms.
Mycotic aneurysms are less common with acute bacterial endocarditis (ABE) than with SBE. When present, however, mycotic aneurysms become symptomatic earlier in the disease course of ABE than in SBE. Intracardiac tumors (eg, left atrial myxomas, metastatic choriocarcinoma) also can embolize fragments, causing aneurysms resembling mycotic aneurysms.
Case reports exist of at least 26 extracranial and 19 intracavernous carotid artery aneurysms associated with endocarditis.
Intracranial hemorrhage
The overall prevalence of hemorrhage in CNS involvement of infective endocarditis is 3-7%. One series showed that nearly 30% of these cases are due to staphylococci. The etiology of CNS hemorrhage in infective endocarditis is not completely clear. It once was believed to be due exclusively to aneurysmal rupture. However, angiographic and autopsy studies did not reveal a consistent aneurysmal source of bleeding in all cases.
In a series that included 14 patients with CNS hemorrhage, 4 definite mycotic aneurysms were identified; aneurysms in 6 more patients were presumptive, and the other 4 CNS hemorrhages were not felt to be aneurysm related. [6] In another series, the source of subarachnoid hemorrhage in 6 out of 8 patients with infective endocarditis could not be identified by cerebral angiography.
Other etiologies include nonaneurysmal vascular wall necrosis and hemorrhagic transformation of ischemic strokes. Intraventricular hemorrhage from a mycotic aneurysm rupture is usually fatal. Subarachnoid hemorrhage in infective endocarditis is often focal; it was shown in one series to occur more frequently in the perisylvian and/or perirolandic regions.
Meningeal processes
A leak of a mycotic aneurysm or an underlying focal lesion can produce meningeal irritation and cause secondary aseptic meningitis. Cases of true meningeal infection can occur with infective endocarditis, but pneumococci are the usual culprits in these cases.
Of all patients with infective endocarditis and concurrent bacterial meningitis, 70% have pneumococci as the infecting organisms (although pneumococci account for only 1-2% of infective endocarditis cases). In patients without a history of trauma, neurosurgery, or cerebrospinal fluid (CSF) leak who have staphylococcal meningitis, a 33% chance exists that they have concurrent staphylococcal endocarditis.
Spinal epidural abscess is also an important complication to recognize in infective endocarditis, and it most commonly presents with motor deficits or back pain. One study found that infective endocarditis was the cause in 10 out of 48 patients admitted with spinal epidural abscess (only slightly behind intravenous drug use as a leading cause). [7]
Seizures
Seizures were part of the presenting complex in 5 of 218 patients in the Massachusetts General Hospital series and were present at some time in the course in 11% (24/218). [3] Focal seizures may indicate an embolic etiology, whereas generalized seizures can result from meningitis, pharmacologic adverse effects, or systemic conditions, such as uremia or hypoxia.
Nonfocal symptoms and/or encephalopathy
Nonfocal symptoms or encephalopathy can be the result of microscopic emboli and subsequent ischemia. This scenario is present in as many as 25% of patients with infective endocarditis. Approximately one half of these cases are due to evident metabolic derangements. The other one half was believed to be related to the infective endocarditis, since no other etiology could be identified.
Most of the nonfocal symptoms, such as headache or encephalopathy, usually resolve shortly after instituting antibiotics.
Immune phenomena
Late proliferative endarteritis in cerebral blood vessels with thrombotic occlusion and subsequent stroke can be due to immune phenomena. In one case report of streptococcal endocarditis with immune complex vasculitis, episodes of neurologic deterioration improved after dexamethasone therapy after a lack of prior improvement with antibiotic therapy.
Epidemiology of CNS Sequelae
Incidence of neurologic sequelae
As previously mentioned, the Massachusetts General Hospital experience from 1964-1973 yielded 218 patients with bacterial endocarditis, 84 of whom had neurologic complications (38%). [3]
Another series (133 patients) demonstrated a similar proportion (41%) of patients with infective endocarditis with neurologic problems. [4]
Mortality associated with neurologic sequelae
Studies have shown that the mortality of patients with bacterial endocarditis with CNS involvement is much greater (58-74%) than that of patients who do not have CNS involvement (20-56%). In one study, during the acute phase of infective endocarditis, 24% of patients with neurologic complications died, while only 10% of those without neurologic complications died. Among the patients with neurologic involvement, mortality was 25% in those treated medically and 20% in those treated surgically.
In one series, 38 major embolic events occurred in 37 patients. Thirty of these 37 patients died (81% mortality).
Differential Diagnosis for CNS Sequelae
Cancer patients who appear to have reactive or behavioral (psychiatric) symptoms actually may have organic embolic disease. If fever, seizures, and/or DIC are present in a patient with cancer, culture-negative bacterial endocarditis may be misdiagnosed as psychiatric disease.
A presentation like that of a transient ischemic attack (TIA) can occur with fluctuating focal neurologic signs. Presumably, the transient nature (resolution) results from the disintegration and dislodgement of small emboli.
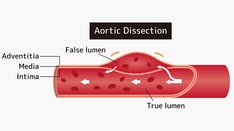
Other conditions to consider in the differential diagnosis include the following:
Depression, psychosis, aseptic meningitis, cavernous sinus syndromes, dissection syndromes, metastatic brain disease, herpes simplex encephalitis, orbital cellulitis, and carotid disease and stroke should also be considered in the differential diagnosis.
Diagnosis of CNS Sequelae
Cerebrospinal fluid examination
In the Massachusetts General Hospital series of 218 patients, 33 had meningeal symptoms (15%). [3] Of patients with CNS involvement from infective endocarditis, one third had completely normal cerebrospinal fluid (CSF), one fourth had a slightly abnormal CSF but an aseptic culture, and one fourth had frankly purulent CSF. Noteworthy as well is that one sixth had hemorrhagic fluid.
When abscess occurs, the CSF can be nearly normal with a mildly increased protein, modest number of cells, normal glucose, and negative Gram stain. Conversely, S aureus abscesses usually are associated with purulent CSF containing polymorphonuclear neutrophilic leucocytes. If the CSF is abnormal, it usually represents an inflammatory consequence (meningeal reaction) rather than a primary infection. This is especially true in patients with acute staphylococcal bacterial endocarditis.
Angiography
For patients with infective endocarditis and focal neurologic deficits, the Cleveland Clinic has recommended 4-vessel angiography at a point between 2 days and 2 weeks from the onset of symptoms.
Others do not pursue routine angiography to search for occult aneurysms but reserve it for patients with established subarachnoid hemorrhage or persistent headache after the infection is controlled.
Brain imaging and echocardiography
Computed tomography (CT) scanning of the brain may be normal in infective endocarditis with CNS involvement, but magnetic resonance imaging (MRI) usually reveals multiple focal areas of ischemia, even in the absence of clinical manifestations of a CNS disorder (in 33 out of 35 patients in one study). [8]
Diffusion-weighted MRI imaging is very sensitive in revealing evidence of ischemic cerebral lesions in patients with infective endocarditis. In one study, diffusion-weighted images revealed ischemic lesions in 33 of 35 patients with infective endocarditis and neurologic symptoms.
Histologic assessment
Macroscopic brain abscesses are rare in patients with SBE (0.5%). Microscopic abscesses (also termed focal cerebritis) are more common (4%) and often are discovered at autopsy. For mass lesions (abscess and/or focal cerebritis), surgery is rarely necessary, since these lesions usually improve and occasionally resolve after antibiotic therapy.
In one series, 9 abscesses were found, with staphylococci the predominant organisms (8 of 9 abscesses were < 1 cm). Abscesses larger than 1 cm usually are not associated with endocarditis. Epidural abscesses can occur in patients with infective endocarditis. One such case in the Massachusetts General Hospital series was unsuspected and was discovered at lumbar puncture. [3]
Pharmacologic Considerations
All medical care should be directed by an infectious disease specialist and the primary care physician.
Antibiotics
Embolization primarily occurs prior to the initiation of antibiotics or within the first week of starting antibiotic therapy. One study found that embolic events decreased from 13 per 1000 patient-days in the first week of antibiotic therapy to 1.2 per 1000 patient-days after 2 weeks of antibiotic therapy.
Antibiotics resolve 50% of formed mycotic aneurysms. They also decrease the risk of bleeding and delay bleeding from mycotic aneurysms from approximately 2-10 days.
Anticoagulants
Anticoagulants are contraindicated in individuals with NVE because of the increased risk of CNS hemorrhage. Some studies have shown that, even after an embolic event, anticoagulants should not be administered. They often are not warranted, because with adequate control of infection within the first week, the risk of CNS embolization declines sharply.
If not anticoagulated, patients with PVE are more likely to have embolic phenomena (50-70% risk).
The risk of neurologic complications is not increased in patients with infective endocarditis who are on anticoagulants at the time of onset of infective endocarditis. Therefore, unless neurologic complications exist, anticoagulation therapy is continued in patients with prosthetic valves but with a lower goal international normalized ratio (INR) of 1.5.
Anticoagulation increases the risk of bleeding from mycotic aneurysms. Early angiography should be performed to guide therapy if aneurysms are present or suspected.
Surgical Considerations
Forty percent of patients with infective endocarditis will need cardiac surgery, primarily for valve repair or replacement. If cardiac valve replacement is planned, an accessible cerebral aneurysm is often clipped or occluded endovascularly prior to surgery, to avoid the risk of hemorrhage from the subsequent cardiac surgery and its inherent anticoagulation perioperatively.
Timing of surgery in patients with infective endocarditis and embolic stroke remains controversial, but a report suggested that surgery can be performed relatively safely within 3 days of stroke if heart failure is severe; otherwise, a delay of 2-4 weeks is preferable. In patients with associated hemorrhage, a delay of at least 4-6 weeks is preferred.
Operative mortality is variable but has been reported as 7.6%, with risk factors for death being cardiogenic shock, insidious illness, and increased age. The 9-year survival rate has been reported to be 71%; risk factors for death include preoperative neurologic complications.
The risk of neurologic deterioration after valve replacement for infective endocarditis is 20% in the first 72 hours, 20-50% 4-14 days postoperatively, less than 10% beyond 14 days postoperatively, and less than 1% after 4 weeks. [9]
Specialist Consultations
The following specialists should be consulted:
-
Infectious disease specialist, internist
-
Neurologist, neurosurgeon
-
Cardiologist, cardiothoracic surgeon
-
Psychiatrist, drug rehabilitation specialist, social services counselor