Practice Essentials
Most patients with meningococcal meningitis, caused by the gram-negative diplococcus Neisseria meningitidis, recover completely if appropriate antibiotic therapy is instituted promptly. Nonetheless, the disease still is associated with a high mortality rate and persistent neurologic defects, particularly among infants and young children.
The image below shows indications of increased intracranial pressure, an early complication of bacterial meningitis.
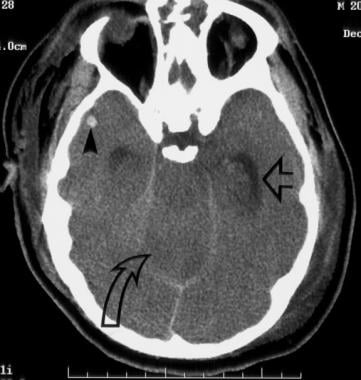 Head CT demonstrates enlargement of the temporal horns indicating increased intracranial pressure (horizontal open large arrow). The closed arrowhead shows small intracerebral hemorrhage foci on the right temporal lobe, and the curved arrow shows the effect of increased intracranial pressure on the cerebellum.
Head CT demonstrates enlargement of the temporal horns indicating increased intracranial pressure (horizontal open large arrow). The closed arrowhead shows small intracerebral hemorrhage foci on the right temporal lobe, and the curved arrow shows the effect of increased intracranial pressure on the cerebellum.
Signs and symptoms
Meningococcal meningitis is characterized by acute onset of the following:
-
Intense headache
-
Fever
-
Nausea
-
Vomiting
-
Photophobia
-
Stiff neck
Lethargy or drowsiness in patients frequently is reported. Stupor or coma is less common. If coma is present, the prognosis is poor.
Patients also may complain of skin rash, which usually points to disease progression. Elderly patients are prone to have an altered mental state and a prolonged course with fever.
Meningococcal septicemia, which is characterized by rapid circulatory collapse and a hemorrhagic rash, is a more severe, but less common, form of meningococcal disease.
Young children
-
In young children, meningococcal meningitis can manifest as follows:
-
Subacute infection that progresses over several days
-
Irritability
-
Projectile vomiting
-
Seizures, usually with a focal onset - Typically during the first few days
-
Waterhouse-Friderichsen syndrome - Characterized by large petechial hemorrhages in the skin and mucous membranes, fever, septic shock, and disseminated intravascular coagulation (DIC)
-
Insidious onset - Can be a feature in infants; stiff neck may be absent
In children, even when the combination of convulsive status epilepticus and fever exists, the classic signs and symptoms of acute bacterial meningitis may not be present. [1]
See Clinical Presentation for more detail.
Diagnosis
Laboratory studies
Laboratory examination of the cerebrospinal fluid (CSF) usually confirms the presence of meningitis. Typical CSF abnormalities in meningitis include the following:
-
Increased opening pressure (>180 mm water)
-
Pleocytosis of polymorphonuclear leukocytes (white blood cell [WBC] counts between 10 and 10,000 cells/µL, predominantly neutrophils)
-
Decreased glucose concentration (< 45 mg/dL)
-
Increased protein concentration (>45 mg/dL)
Other laboratory tests can include the following:
-
Culture of CSF and blood specimens - To identify N meningitidis and the serogroup of meningococci, as well as to determine the bacterium’s susceptibility to antibiotics
-
Polymerase chain reaction (PCR) assay - For confirmation of the diagnosis
Imaging studies
-
Computed tomography (CT) scanning - Indications for performing CT scanning prior to lumbar puncture include an altered level of consciousness, papilledema, focal neurologic deficits, and/or focal or generalized seizure activity
-
Magnetic resonance imaging (MRI) - MRI with contrast is preferred to CT scanning, because MRI better demonstrates meningeal lesions, cerebral edema, and cerebral ischemia
Electroencephalography
An electroencephalogram (EEG) study is sometimes useful to document irritable electrical patterns that may predispose the patient to seizures.
See Workup for more detail.
Management
To prevent serious neurologic morbidity and death, prompt institution of antibiotic therapy is essential when the diagnosis of bacterial meningitis is suspected. Antimicrobial treatment should be administered as soon as possible after a lumbar puncture is performed.
Empiric pharmacologic therapy
Initial empiric therapy until the etiology of the meningitis is established should include the following agents:
-
Dexamethasone
-
A third-generation cephalosporin - Eg, ceftriaxone or cefotaxime
-
Vancomycin
-
Acyclovir - Should be considered according to the results of the initial CSF evaluation
-
Doxycycline - Should also be added during tick season in endemic areas
Postdiagnosis pharmacologic therapy
-
Ceftriaxone (or cefotaxime) - The drug of choice for the treatment of meningococcal meningitis and septicemia
-
Penicillin - Alternative
-
Ampicillin - Alternative
-
Dexamethasone - Controversial in the management of bacterial meningitis in adults
Prophylaxis
Deterrence and prevention of meningococcal meningitis can be achieved by either immunoprophylaxis or chemoprophylaxis. Rifampin, quinolones, and ceftriaxone are the antimicrobials that are used to eradicate meningococci from the nasopharynx.
Several meningococcal vaccines are available in the United States:
-
Meningococcal groups A, B, C, W, and Y (Penbraya)
-
Meningococcal conjugate or MenACWY vaccine (Menactra, Menveo, MenQuadfi)
-
Meningococcal group B vaccine (Bexsero, Trumenba)
See Treatment and Medication for more detail.
Background
Meningococcal meningitis (International Classification of Disease-9 [ICD-9] code: 036.0) has been recognized as a serious problem for almost 200 years. It was first identified definitely by Vieusseux in Geneva in 1805.
The causative organism, Neisseria meningitidis, is a gram-negative, aerobic, encapsulated diplococcus that grows best on enriched media, such as Mueller-Hinton or chocolate agar, at 37°C and in an atmosphere of 5-10% carbon dioxide.
Meningococcal disease still is associated with a high mortality rate and persistent neurologic defects, particularly among infants and young children.
The first successful treatment of meningitis with intravenous and intrathecal penicillin was reported in 1944, and the first clinical trials using high doses of intravenous penicillin as monotherapy for the treatment of meningitis were reported in 1950. Since then, penicillin has remained the drug of choice for the treatment of meningococcal meningitis. [2] However, current IDSA guidelines list ceftriaxone or cefotaxime as the drugs of choice.
The image below shows indications of increased intracranial pressure, an early complication of bacterial meningitis.
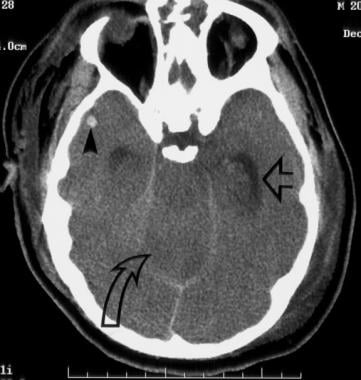 Head CT demonstrates enlargement of the temporal horns indicating increased intracranial pressure (horizontal open large arrow). The closed arrowhead shows small intracerebral hemorrhage foci on the right temporal lobe, and the curved arrow shows the effect of increased intracranial pressure on the cerebellum.
Head CT demonstrates enlargement of the temporal horns indicating increased intracranial pressure (horizontal open large arrow). The closed arrowhead shows small intracerebral hemorrhage foci on the right temporal lobe, and the curved arrow shows the effect of increased intracranial pressure on the cerebellum.
Serogroups
Meningococci make up numerous serogroups that are based on the composition of their polysaccharide capsular antigens. They differ in their agglutination reactions to sera directed against polysaccharide antigens. At least 13 serogroups have been described: A, B, C, D, E, H, I, K, L, W-135, X, Y, and Z. Serogroups B and C have caused most cases of meningococcal meningitis in the United States since the end of World War II; before that, group A was more prevalent. More than 99% of meningococcal infections are caused by serogroups A, B, C, 29E, or W-135.
In Europe and the Americas, serogroup B is the predominant agent causing meningococcal disease, followed in frequency by serogroup C. Historically, serogroup A was the main cause of epidemic meningococcal disease globally, and it is still the predominant cause of meningococcal meningitis in Africa and Asia.
Go to Haemophilus Meningitis, Meningitis, Staphylococcal Meningitis, Tuberculous Meningitis, Viral Meningitis, and Aseptic Meningitis for more complete information on these topics.
Etiology
Individuals acquire meningococcal infections if they are exposed to virulent bacteria and have no protective bactericidal antibodies.
The natural habitat and reservoir for meningococci is the mucosal surfaces of the human nasopharynx and, to a lesser extent, the urogenital tract and anal canal. Approximately 5-10% of adults are asymptomatic nasopharyngeal carriers, but that number increases to as many as 60-80% of members of closed populations (eg, military recruits in camps).
The modes of infection include direct contact or respiratory droplets from the nose and throat of infected people. Meningococcal disease most likely occurs within a few days of acquisition of a new strain, before the development of specific serum antibodies.
The incubation period averages 3-4 days (range 1-10 days), which is the period of communicability. Bacteria can be found for 2-4 days in the nose and pharynx and for up to 24 hours after starting antibiotics. Treatment with penicillin may not eradicate the bacteria from the nasopharyngeal carriers.
After adherence to the nasopharyngeal mucosa, meningococci are transported to membrane-bound phagocytic vacuoles. Within 24 hours, they can be seen in the submucosa, close to vessels and local immune cells. In most cases, meningococcal colonization of mucosal surfaces leads to subclinical infection or mild symptoms.
In approximately 10-20% of cases, N meningitidis enters the bloodstream. In the vascular compartment, the bacterium may be killed by bactericidal antibodies, complement, and phagocytic cells, or it may multiply, initiating the bacteremic phase. Organisms replicate rapidly.
Systemic disease appears with the development of meningococcemia and usually precedes meningitis by 24-48 hours. This can lead to systemic infection in the form of bacteremia, metastatic infection that commonly involves the meninges, or severe systemic infection with circulatory collapse and DIC. Meningococcemia leads to diffuse vascular injury, which is characterized by endothelial necrosis, intraluminal thrombosis, and perivascular hemorrhage.
Risk factors
Meningococci that elaborate a capsule can lead to invasive disease. The capsule protects them from desiccation and from host immune mechanisms. Adhesins and endotoxins also enhance their pathogenic potential. Dysfunctional properdin (ie, component of the alternative pathway of complement), HIV infection, functional or anatomical asplenia, and congenital complement deficiencies predispose individuals to meningococcal disease.
Smoking and concurrent viral infection of the upper respiratory tract diminish the integrity of the respiratory mucosa and increase the likelihood of invasive disease. Crowding living conditions also facilitate disease spread, since individuals from different areas have different strains of meningococci.
Epidemiology
Frequency and serogroup incidence in the United States
Since 1960, the incidence of meningococcal meningitis in the United States has been stable, at approximately 0.9-1.5 cases per 100,000 people per year. Most cases occur during winter and early spring.
Serogroups B and C have caused most cases of meningococcal meningitis in the United States since World War II. An increased frequency of serogroup B and Y meningococci has been noted since 1990. The frequency of localized outbreaks has increased since 1991. [3, 4]
Global disease distribution
As previously mentioned, In Europe and the Americas, serogroup B is the predominant agent causing meningococcal disease, followed in frequency by serogroup C. Historically, serogroup A was the main cause of epidemic meningococcal disease globally, and it is still the predominant cause of meningococcal meningitis in Africa and Asia.
In the African "meningitis belt" (a region of savanna that extends from Ethiopia in the east to Senegal in the west), this disease frequently occurs in epidemics during the hot and dry weather (December to March).
The meningococcal meningitis pandemic that began in 1996 has resulted so far in approximately 300,000 cases being reported to the World Health Organization (WHO).
Morbidity and mortality in meningococcal meningitis
Morbidity and mortality rates from the disease remain high. Apart from epidemics, at least 1.2 million cases of bacterial meningitis are estimated to occur every year; 135,000 of them are fatal. Approximately 500,000 of these cases and 50,000 of the deaths are due to meningococci.
Early complications of bacterial meningitis include seizures, raised intracranial pressure (seen in the image below), cerebral venous thrombosis, sagittal sinus thrombosis, and hydrocephalus. The risk of cerebral herniation from acute meningitis is about 6-8%.
 Head CT demonstrates enlargement of the temporal horns indicating increased intracranial pressure (horizontal open large arrow). The closed arrowhead shows small intracerebral hemorrhage foci on the right temporal lobe, and the curved arrow shows the effect of increased intracranial pressure on the cerebellum.
Head CT demonstrates enlargement of the temporal horns indicating increased intracranial pressure (horizontal open large arrow). The closed arrowhead shows small intracerebral hemorrhage foci on the right temporal lobe, and the curved arrow shows the effect of increased intracranial pressure on the cerebellum.
In fulminant meningococcemia, severe disseminated intravascular coagulation (DIC) may develop, leading to hemorrhagic diathesis with bleeding into the lungs, urinary tract, and gastrointestinal tract. Ischemic complications of DIC also are common.
Infrequent suppurative complications include septic arthritis, purulent pericarditis, endophthalmitis, and pneumonia. Of survivors, 10% developed allergic complications manifested as cutaneous vasculitis or arthritis.
Late complications may include communicating hydrocephalus (which can present with gait difficulty, mental status changes, and incontinence) and hearing loss. [5]
In one study, 27% of survivors experienced 1 or more suppurative, allergic, or neurologic complications, including hearing loss, cutaneous vasculitis, and arthritis.
Hearing loss, noted in 9% of children, occurred significantly more often in patients with marked leukocytosis or leukopenia or with cerebrospinal fluid (CSF) leukocytosis greater than 10 X 109/L.
The Waterhouse-Friderichsen syndrome may develop in 10-20% of children with meningococcal infection. This syndrome is characterized by large petechial hemorrhages in the skin and mucous membranes, fever, septic shock, and DIC.
Even when the disease is diagnosed early and adequate therapy is instituted, the case-fatality rate in meningococcal meningitis ranges from 5-10%; it may exceed 40% in patients with meningococcal sepsis.
In a review of 493 episodes of bacterial meningitis in adults, the overall case-fatality rate was 25%. In another study, patients with meningococcal meningitis had a case-fatality rate of 7.5%. [6]
In developing countries, the mortality rate from bacterial meningitis is often higher (20-40%) than in developed countries.
Among those who survive the meningococcal disease, 10-20% experience neurologic sequelae.
A cohort study from Netherlands (the Meningitis Cohort Study) revealed a 7% mortality rate and an unfavorable outcome in 12% of the cases. [7]
Race predilection
In one study conducted in the United States, the incidence of meningococcal disease was slightly higher in African Americans (1.5 cases per 100,000 people) than in whites (1.1 cases per 100,000 people).
Sex predilection
In one study conducted in the United States, males accounted for 55% of total cases of meningococcal meningitis.
Age predilection
Meningococcal meningitis most commonly affects individuals aged between age 3 years and adolescence. It rarely occurs in individuals older than 50 years.
Prognosis
The prognosis for meningococcal meningitis is fair if the patient does not have focal neurologic deficits and is not stuporous or comatose. The prognosis for meningococcal disease is poor when the infection has a septicemic component. Most patients with meningococcal meningitis recover completely if appropriate antibiotic therapy is instituted promptly.
Thrombocytopenia, a lowered coagulation index, moderate anemia (hemoglobin < 11 g/dL), an obtunded mental state, and a history of convulsions were reported to be poor prognostic factors.
In one study, only anemia was correlated independently with fatality; the results suggested that anemia should be considered an important prognostic marker in the acute phase of meningococcal meningitis.
Patient Education
Advise any household contacts and close respiratory contacts that chemoprophylaxis agents are available to eliminate the carrier state and prevent the spread of infection. [8]
For patient education information, see the Brain and Nervous System Center, as well as Meningitis in Adults and Meningitis in Children.
-
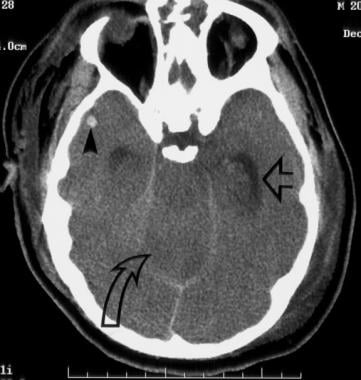
Head CT demonstrates enlargement of the temporal horns indicating increased intracranial pressure (horizontal open large arrow). The closed arrowhead shows small intracerebral hemorrhage foci on the right temporal lobe, and the curved arrow shows the effect of increased intracranial pressure on the cerebellum.
-
Head CT shows small intracerebral hemorrhage foci (vertical closed arrow). Basal ganglia can also not be visualized because of diffuse edema (oblique closed arrow). The black arrow head on the left shows soft tissue edema.