Overview
EEG-video monitoring refers to continuous EEG recorded for a more or less prolonged period with simultaneous video recording of the clinical manifestations. Having a correlation of the recorded behavior (video) and the EEG activity, the diagnosis of seizures or nonepileptic attacks can be made definitely in nearly all cases. EEG-video is the criterion standard for the diagnosis. [1, 2, 3, 4]
EEG-video monitoring has become available at most large referral centers with an epilepsy program, and more recently in many smaller hospitals and on an outpatient basis. As a general rule, prolonged EEG-video monitoring should be obtained on any patient who continues to have frequent seizures despite antiepileptic drugs. [5]
The purpose of EEG-video is to answer the following questions:
-
Are the episodes epileptic seizures?
-
If not, what are they?
-
If they are epileptic seizures, what type of epilepsy is it?
-
If the seizures are focal, from where are they arising?
Indications
Currently, EEG-video monitoring is severely underused, as evidenced by the following: 1) The delay for PNEA diagnosis is 7-10 years [6] ; 2) The delay for successful epilepsy surgery is more than 15 years. [7]
Any patient with frequent (weekly) seizurelike episodes despite antiepileptic drug therapy should have EEG-video monitoring. This can help differentiate epileptic seizures from nonepileptic seizure mimics such as psychogenic nonepileptic attacks (PNEA) and organic seizure-mimics like syncope and parasomnias.
Technical Aspects
EEG
Modern EEG-video systems vary in methods of data storage, retrieval, and review. Outpatient ambulatory video-EEG systems have the advantage of keeping the patient in an environment that includes the usual stressors. Inpatient video-EEG systems save the data on hard drives and servers that can be accessed remotely.
Inpatient video-EEG monitoring is performed in a fixed epilepsy monitoring unit and consists of a network that uses cameras fixed in the patient rooms that are linked to a central server. The video signal is digitized and synchronized. Both EEG and video signals are displayed simultaneously for online observation.
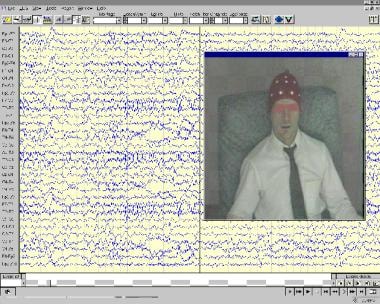 A display of a typical video-EEG monitoring machine. Continuous multichannel EEG is displayed along with a video image of the monitored subject.
A display of a typical video-EEG monitoring machine. Continuous multichannel EEG is displayed along with a video image of the monitored subject.
A review station displays the EEG data, which may be displayed faster than real time for rapid review. EEG recorded in a digital referential format may be displayed later in a variety of referential or bipolar montages.
Spike and seizure detection
Computer detection software can identify interictal epileptiform discharges and seizures. This detection software greatly reduces the amount of EEG raw data that needs to be reviewed. Detection is based on quantitative parameters such as wave frequency, amplitude, sharpness, rhythmicity, and duration. These parameters may be adjusted on a case-by-case or channel-by-channel basis to maximize sensitivity and minimize false detections. Automated detections should have a high sensitivity and a low rate of false negative since they are reviewed critically by the EEGer. They should not be used without a review by an epileptologist/EEGer, as they would then result in a serious over-reading. [8, 9]
Video
A camera is used to visually record all the physical activities of the patient while in the monitoring unit and at the same time the EEG is recording the brain activity. A monitor at the nurses’ station is desirable so that the patient can be monitored at all times. The patients are given a portable alarm system to activate once an event is experienced or witnessed. It is important that the patient or family member cooperate in pressing the alarm once the habitual event is recognized to notify the staff that the patient needs to be assessed and that the video needs to be reviewed.
Technologist’s review
The registered technician reviews and evaluates the raw EEG and video data in the epilepsy monitoring units. The technologist also performs daily scanning, documentation, and annotation of ictal, interictal, and paroxysmal events and creates file clips that represent these findings.
Activation procedures
Standard EEG activation procedures are hyperventilation, photic stimulation, and sleep deprivation. Exercise or other less common triggers may provoke seizures. Provocative techniques specifically for the diagnosis of PNEA are meant to prove suggestibility (see the Medscape Reference article Psychogenic Nonepileptic Seizures).
Antiepileptic drug (AED) withdrawal
AEDs may be decreased or stopped while in the hospital undergoing the EEG-video monitoring if the frequency of the events is not high enough. A reduction of AEDs can even be initiated prior to admission. When AEDs are reduced, IV access is mandatory. If the typical event is considered serious, the medications should be reduced with caution and preferably choose the one that can be reloaded intravenously, if necessary. This is very individual, and there is no standard protocol. Some centers never decrease medications beforehand.
Outcome of EEG-Video Monitoring - Nonepileptic Conditions
Psychogenic nonepileptic attacks
Psychogenic nonepileptic attacks (PNEAs) are by far the most common condition misdiagnosed as epilepsy seen in epilepsy monitoring units (EMUs). EEG-video monitoring is the criterion standard for a diagnosis of PNEA. The principle is to record an episode and demonstrate that 1) no epileptiform change occurs in the EEG during the typical clinical event and 2) the clinical event is not consistent with seizure types that can be unaccompanied by ictal EEG changes. The combination of a recorded typical attack with normal ictal EEG makes the diagnosis a nonepileptic event but does not in itself categorize it as psychogenic. Provocative techniques, activation procedures, or inductions can be performed to trigger the habitual event and proves suggestibility. The pros and cons of these techniques have been discussed extensively. [10] The diagnosis of PNEA with EEG-video is not difficult most of the time, but there can be difficult situations.
The most common video features of PNEA that can be seen include a very gradual onset or termination; pseudosleep; discontinuous (stop and go), irregular, or asynchronous (out of phase) activity; side-to-side head movements; pelvic thrusting; opisthotonic posturing; stuttering; weeping; preserved awareness during bilateral motor activity; and persistent eye closure.
For further information, see the Medscape Reference article Psychogenic Nonepileptic Seizures.
Nonepileptic organic conditions seen in an EMU
See the list below:
-
Syncope
Syncope is commonly misdiagnosed as a seizure, but mostly in the outpatient setting. It is a distant second to PNEA in conditions misdiagnosed as seizures that are seen in an EMU. One important reason for the misdiagnosis is the frequency with which syncopal events are convulsive.
Motor symptoms associated with syncope are clonic- or myoclonic-like, tend to last only a few seconds, and terminate once the patient is horizontal, in contrast to the typical generalized tonic-clonic seizure duration of 30-90 seconds.
EEG is very sensitive to decreased cerebral flow, and by the time loss of consciousness occurs, EEG changes are present. When syncope is recorded on EEG-video, there is a very stereotyped pattern of changes (delta slowing and suppression). Syncope (anoxia), when prolonged, can evolve into clear seizures confirmed by EEG recording. However, several symptoms are helpful in pointing one way or the other.
Historical features that favor syncope include presyncopal prodromes (vertigo, dizziness, lightheadedness, nausea, chest pain) as well as age and a history of cardiovascular disease. Historical features that favor seizures include lateral tongue biting, head turning, posturing, urinary incontinence, cyanosis, prodromal déjà vu, and postictal confusion.
-
Parasomnias
Parasomnias are short-lived paroxysmal behaviors that occur out of sleep. They constitute the main differential diagnosis of seizures for nocturnal episodes. In particular, the non-REM parasomnias (night terrors, sleepwalking, and confusional arousals) can superficially resemble seizures since they include complex behaviors and some degree of unresponsiveness and amnesia for the event.
Rhythmic movement disorder is a parasomnia typically seen at transition or stage 1 sleep that can also resemble partial seizures. One common example is head banging (jactatio capitis). Among REM sleep parasomnias, nightmares rarely present a diagnostic challenge, but REM behavior disorder with violent and injurious behaviors during REM sleep may be a diagnostic challenge.
The diagnosis of REM behavior disorder by history is usually easy because it affects older men and the description of acting out a dream is quite typical. EEG-video usually confirms the absence of an EEG seizure and shows that the behavior arises from a specific stage of sleep.
Occasionally, in the absence of ictal EEG changes, the differentiation between seizure and parasomnia can be difficult.
-
Hypnic jerks or sleep starts
Hypnic jerks are benign myoclonic jerks that can resemble the jerks of myoclonic seizures.
Their occurrence only upon falling asleep stamps them as benign nonepileptic phenomena.
They occur at all ages and are easily identified on EEG-video by the fact that they occur in wake to stage 1 transition and have no EEG correlate associated with the jerks.
-
Panic attacks
Panic attacks are paroxysmal manifestations of anxiety or panic disorder and may be mistaken for seizures. Conversely, fear is a relatively common aura in patients with mesiotemporal epilepsy.
The identification of fear as an epileptic aura is easy when it evolves into a clear seizure but can be difficult in the absence of other seizure types.
Panic attacks include intense autonomic, especially cardiovascular and respiratory, symptoms. Abrupt and intense fear is accompanied by at least 4 of the following symptoms: palpitations, diaphoresis, tremulousness or shaking, shortness of breath or sensation of choking, chest discomfort, nausea or abdominal discomfort, dizziness or lightheadedness, derealization or depersonalization, fear of losing control, fear of dying, paresthesias, and chills or hot flashes. The symptoms typically peak within 10 minutes.
-
Nonepileptic myoclonus: This is defined as myoclonus that is not of cortical origin (ie, not visible on EEG). Hiccups and hypnic jerks are examples of normal nonepileptic myoclonus, but abnormal nonepileptic myoclonus can be seen in metabolic or toxic encephalopathies and neurodegenerative diseases.
-
Hemifacial spasm
Hemifacial spasm may superficially resemble a simple partial seizure with motor symptoms of the face, or more simply a facial clonic seizure.
Hemifacial spasm is a chronic progressive disorder.
While facial motor seizures typically involve the perioral area (due to a large representation on the motor homunculus), the unilateral facial twitching of hemifacial spasm typically affects the periorbital muscles first and then spreads to other (ipsilateral) facial muscles over a period of months to years.
Conditions specific to young children
In children and adolescents who have been misdiagnosed as having seizures, in contrast to adults, only 50% have psychological disorders (90% being PNEA), but other psychiatric diagnoses (eg, episodic dyscontrol with rage attacks, behavioral outbursts, panic/anxiety disorder, and factitious disorder by proxy) may be present. The other 50% have nonpsychogenic conditions, the most common of which is nonepileptic inattention with staring spells. Other diagnoses include stereotyped mannerisms, hypnic jerks, parasomnias, tics, gastroesophageal reflux with posturing or laryngospasm, arousals, shuddering attacks, and apneas. Physiologic and organic events predominate in infants and young children, and psychiatric disorders become much more common during later childhood and adolescence.
-
Tics: Tics can superficially resemble simple partial seizures with motor symptoms. Tics tend to occur throughout the day, are sporadic, stereotyped (the same movement repeats itself without evolving, and the same muscle group is involved), and disappear in sleep. They are preceded by an urge to move and are suppressible. Tics are also followed by a sense of ‘‘just right’’ or relief. They are particularly common in children aged 5-10 years.
-
Shuddering attacks: Shuddering attacks are benign paroxysmal spells of older infants and young children. These episodes are usually benign, have no association with increased morbidity or mortality, and tend to remit spontaneously. Parents describe the paroxysmal episodes as a sudden flexion of the neck and trunk and adduction of the arms. A shiverlike movement of the trunk occurs, and the body may stiffen. Consciousness does not seem to be altered, but this can be difficult to confirm. The episode usually lasts 5-15 seconds. Unlike epileptic seizures, shuddering attacks do not occur during sleep.
-
Breath-holding spells (cyanotic infantile syncope): These spells affect children aged 6 months to 5 years. Typically, a clear trigger is present, with the child being upset and crying. At the end of expiration, the child is unable to relax and inhale and becomes apneic and cyanotic. The child may appear angry and upset about this uncomfortable feeling, loses consciousness, may have urinary incontinence, and becomes stiff or even opisthotonic. The EEG during the event typically shows high-amplitude slowing followed by suppression, as is seen in syncope of any cause. When the child relaxes and breathes again, consciousness is gradually regained.
-
Gastroesophageal reflux: Reflux associated with laryngospasm in infants may cause events that look like seizures, with limb posturing, eye deviation, and even opisthotonus. These events tend to occur in sleep and in the postprandial period, and recurrent vomiting is typically present.
-
Benign myoclonus of infancy: Benign myoclonus of infancy must be differentiated from infantile spasms. This requires EEG-video monitoring because the events appear clinically similar. This benign phenomenon resolves spontaneously within a year without neurologic sequelae.
-
Mannerisms: Mannerisms are common in young children, in particular those with a mental handicap. Mannerisms can look odd and unnatural and occasionally mimic motor seizures. Similarly, self-stimulating behaviors, such as masturbation, can be erroneously interpreted as seizures.
-
Spasmus nutans: Spasmus nutans is a benign triad of head nodding, head tilt, and pendular nystagmus, which typically occurs between ages 4 and 12 months.
Benign nonspecific symptoms misinterpreted as seizures
This is an under-reported phenomenon, which consists of the overinterpretation of benign or nonspecific symptoms as seizures. Common unexplained symptoms include transient dizziness, limb numbness, head sensations, and various mild and brief involuntary movements. The misinterpretation of these symptoms is more likely to occur in anxious patients or caregivers with hypochondriacal tendencies. It is also more common in patients who also have or have had seizures, or who have other organic conditions.
Another setting is the intensive care unit, where many patients who are very ill can have nonspecific abnormal movements such as shivers, twitches, or tremors, but are neither epileptic nor psychogenic. EEG-video recordings usually clarify the situation, but since many of the mild nonspecific symptoms mimic simple partial seizures or auras rather than more severe seizures, the mere presence of a normal ictal EEG does not in itself exclude seizures. However, the video, (ie, the characteristics of the movements), usually does exclude seizures, as they are not clonic, tonic, or myoclonic. At times the distinction can be difficult, and when in doubt, being conservative is preferable to labeling the episodes as seizures. [1]
Outcome of EEG-Video Monitoring - Epilepsy
Localization-Related Epilepsy
Temporal lobe epilepsy
Temporal lobe epilepsy is the most common localization-related epilepsy seen in EMUs. Complex partial seizures are the most common manifestation. About one third of patients have secondarily generalized tonic-clonic seizures in addition to complex partial seizures or as their primary seizure type.
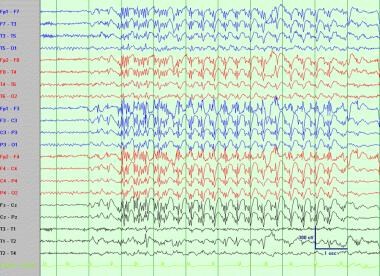
Interictal EEG typically shows temporal sharp waves maximum at anterior or mid temporal electrodes.
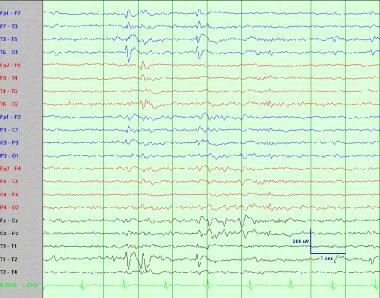
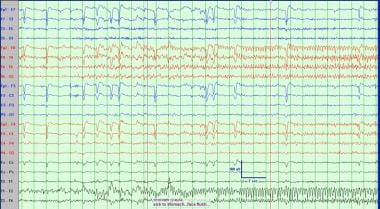
Temporal intermittent rhythmic delta activity (TIRDA) is observed in as many as 25-40% of patients being evaluated for temporal lobe resection. The ictal EEG shows relatively well-defined rhythmic and evolving discharges with a characteristic buildup, with a usual frequency in the theta range (see images below). Lateralized postictal slowing is often observed.
Distinctive characteristics of mesial temporal lobe epilepsy seizures include the following: aura of a rising epigastric sensation (often likened to a roller coaster), and psychic or experiential phenomena, such as déjà vu, jamais vu, or fear. Complex partial seizures usually manifest with a behavioral arrest and staring and last from 30-120 seconds. The patients are generally unaware and unresponsive during this period. Automatisms are common and consist of repetitive, stereotyped, purposeless movements. In temporal lobe epilepsy, they are typically mild, involving the hands (picking, fidgeting, fumbling) and mouth (chewing, lip smacking).
Extratemporal epilepsy
Extratemporal epilepsy is more diverse, depending on the location of the seizure-onset zone. Frontal lobe seizures are most common in this group and are characterized by short duration (< 30 s) and predilection for occurrence during sleep. Seizure clusters and status epilepticus are also more common than with temporal lobe epilepsy.
A postictal state may be brief or absent. Both ictal and interictal EEG can be misleading in frontal lobe epilepsy with normal or nonspecific abnormal findings.
Complex partial seizures are often characterized by hypermotor behaviors, and bizarre-looking episodes that may be mistaken for psychogenic nonepileptic seizures. Tonic posturing and head and eye deviation (version), usually contralateral to the side of the seizure focus, can occur in some patients. Vocalizations are also common. Occipital lobe epilepsy is characterized by initial visual and parietal lobe epilepsy by somatosensory symptoms.
Hemispheric Syndromes
These syndromes are localization-related and neocortical, but the epileptogenic zone is so widespread as to involve nearly an entire hemisphere. In most cases, structural abnormalities are identified on magnetic resonance imaging (MRI). EEG abnormalities include multifocal or widespread discharges lateralized to 1 hemisphere, along with amplitude asymmetry, lateralized or focal slowing, and background slowing. Hemiparesis, hemianopia, and developmental delay often coexist. Causes include perinatal infarction, Rasmussen syndrome, Sturge-Weber syndrome, and hemimegalencephaly.
Symptomatic Generalized Epilepsy
Symptomatic generalized epilepsy refers to epilepsy syndromes caused by a diffuse brain insult. Known etiologies associated with brain dysfunction include anoxic birth injury, trauma (the most common), infection, metabolic defect, developmental malformations, or chromosomal abnormalities. There is usually clinical evidence of diffuse brain dysfunction either intellectually, or motor, or both.
EEG usually shows evidence of diffuse brain dysfunction in the form of slowing in addition to the epileptic discharges. The EEG manifestations are not specific as to etiologies, but vary markedly with age, and are thus age dependent. The types of generalized seizures that occur in symptomatic generalized epilepsy include myoclonic, tonic, atonic (see video below), atypical absence, and generalized tonic-clonic. The most common types seen in EMU are West syndrome and Lennox-Gastaut syndrome.
Idiopathic Generalized Epilepsy
Idiopathic generalized epilepsy, also called primary generalized epilepsy, is a group of epilepsy that has very distinct features. They have a genetic basis and are not caused by a structural lesion. Thus, a family history of epilepsy exists. This epilepsy tends to begin during childhood or adolescence, although it may not be diagnosed until adulthood. Patients with idiopathic generalized epilepsy have normal intelligence, normal neurologic examination, and normal MRI. EEG shows generalized epileptiform discharges and may show photosensitivity.
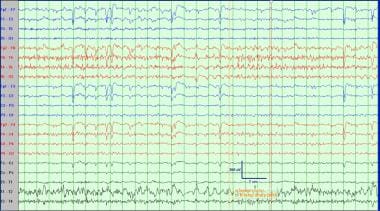
Patients with idiopathic generalized epilepsy have 1 or more of 3 types of seizures: generalized tonic-clonic (see videos below), absence, and myoclonic seizures. Their EEG equivalents are generalized spikes, sharp waves, polyspikes, and spike-wave complexes (see image below).
Depending on age at onset, predominant seizure type(s), and EEG findings, several subtypes of idiopathic generalized epilepsy exist. These types are childhood absence epilepsy, juvenile myoclonic epilepsy, and adult-onset idiopathic generalized epilepsy. The idiopathic generalized epilepsies are usually easy to treat (ie, about 90% of patients respond to medications). Many idiopathic generalized epilepsies are outgrown in young adulthood, with the exception of juvenile myoclonic epilepsy. [11]
Pitfalls in EEG-Video Monitoring
Ictal EEG has limitations because it may be negative in simple partial seizures and in some complex partial seizures, especially those of frontal lobe onset. Ictal EEG may also be uninterpretable or difficult to read if movements generate excessive artifact. Therefore, knowledge of the types of clinical seizures that may be unaccompanied by ictal EEG changes is critical. The most common type of seizures that are unaccompanied by ictal EEG changes are those without impairment of awareness (ie, simple partial seizures). This includes all simple partial seizures with subjective phenomena (ie, auras) that can involve the 5 senses as well as psychic or experiential sensations. Other simple partial seizures that are commonly unaccompanied by ictal EEG changes are brief tonic phenomena such as those typical of frontal lobe seizures.
The lack of ictal EEG changes only indicates that the episodes are nonepileptic, and nonepileptic does not always mean psychogenic. Other diagnoses must be considered before making a diagnosis of psychogenic nonepileptic attacks. The most common ones to consider are syncope for episodes that occur during waking, and parasomnias for episodes that occur in sleep.
A common myth is that a recorded episode with a negative EEG is all it takes to make a diagnosis of psychogenic nonepileptic attacks. This is grossly inaccurate. A negative EEG can only be interpreted in the context of the semiology of the attack in question. Thus, both the video and EEG must be available.
Errors in EEG interpretation are frequent and a major cause of epilepsy misdiagnosis. [8, 9] They happen on routine EEGs but also during EEG-video monitoring.
EEG-video monitoring is a powerful procedure and is best performed at an experienced center.
Questions & Answers
Overview
What is electroencephalography (EEG) video monitoring?
What is the purpose of electroencephalography (EEG) video monitoring?
When is electroencephalography (EEG) video monitoring performed?
How is electroencephalography (EEG) video monitoring performed?
What is the role of electroencephalography (EEG) video monitoring in spike and seizure detection?
What is the role of the video camera in electroencephalography (EEG) video monitoring?
What is the technologist's role in electroencephalography (EEG) video monitoring?
Which activation procedures are used in electroencephalography (EEG) video monitoring?
When are antiepileptic drugs (AEDs) withdrawn in electroencephalography (EEG) video monitoring?
Which findings on electroencephalography (EEG) video monitoring are characteristic of syncope?
Which findings on electroencephalography (EEG) video monitoring are characteristic of parasomnia?
Which findings on electroencephalography (EEG) video monitoring are characteristic of panic attacks?
What are the limitations of electroencephalography (EEG) video monitoring?
-
A display of a typical video-EEG monitoring machine. Continuous multichannel EEG is displayed along with a video image of the monitored subject.
-
Complex partial seizure. Typical temporal lobe seizure with oral (chewing) and manual automatisms. Note the clear loss of awareness (patient unable to follow commands).
-
Psychogenic nonepileptic attacks. The event is provoked by an induction (or provocative) technique. Note the typical irregular nonclonic nontonic and asynchronous movements (including bicycling) with stop-and-go phenomenon.
-
Generalized clonic seizure. This event begins with staring to the left and left clonic eye movements and evolves into bilateral clonic jerking of all extremities with a clonic epileptic cry.
-
Atonic seizure. Abrupt loss of muscle tone is followed by clonic rhythmic movements. This type of seizure is typical for the symptomatic generalized epilepsies of the Lennox-Gastaut type.
-
Generalized tonic clonic of idiopathic generalized epilepsy. Increased tone in all extremities associated with an epileptic cry followed by rhythmic clonic movements. No focal features observed.
-
Interictal generalized spike-wave complexes (idiopathic generalized epilepsy).
-
Ictal EEG recording of right temporal lobe epilepsy.
-
Ictal EEG recording of right temporal lobe epilepsy.
-
Interictal left temporal sharp wave (left temporal lobe epilepsy).
-
Typical generalized tonic seizure in an adult patient with a "symptomatic" (now termed structural-metabolic) generalized epilepsy of the Lennox-Gastaut type.
-
Typical generalized tonic seizure in a patient with a "symptomatic" (now termed structural-metabolic) generalized epilepsy of the Lennox-Gastaut type and severe static encephalopathy with cerebral palsy.
-
Typical myoclonic seizure in an adult patient with a generalized epilepsy of the Lennox-Gastaut type. These episodes were causing the patient to fall.