Overview
Spatial neglect is a behavioral syndrome occurring after brain injury. Spatial neglect is defined as pathologically asymmetric spatial behavior, caused by a brain lesion and resulting in disability. [1, 2, 3] As we identify input, knowledge storage, and output information processing stages in aphasia and other cognitive disorders, [4] we can also identify modular, stagewise spatial cognitive processing. Perceptual-attentional Where input, Where representational, and motor-intentional Aiming output can be separately impaired in spatial neglect, or impaired in combination. [5] When patients are identified as having spatial neglect, their deficits must not be fully attributable to primary sensory deficits (e.g., hemianopia) or motor disturbance (e.g., hemiparesis). Treatment for spatial neglect focuses on visuomotor, cognitive, and behavioral training, in a rehabilitation program including specific exercises. There is emerging information on biological approaches to treat this disorder, but none are yet part of standard care. [6] Management of spatial neglect is also tremendously important, including alterations to the patient's environment and caregiver counseling.
Despite the fact that speech and language, memory, and other mental abilities may be spared in brain-injured patients with spatial neglect, the prognosis for recovery of independent function in patients with spatial neglect is significantly worse than in those with seemingly more disabling deficits in these other abilities. [2, 7] Even global aphasia and right hemiparesis may not have as great an effect on the ability to become independent. [8] Because spatial neglect is so disabling, it is troubling that most people with spatial neglect may not be identified, even when evaluated by stroke specialists. [9]
Although patients may recover from spatial neglect as assessed on paper and pencil tests, they frequently have persistent disability, for example, reduced community mobility. [10] This may be related to impaired motor-intentional Aiming in spatial neglect. Paper and pencil testing may detect mainly visual, perceptual-attention impairment (Where spatial neglect). In contrast, assessment of actual functional performance for spatial errors captures motor-exploratory disability and predicts daily life competence. [11, 12] Thus, because motor-intentional Aiming symptoms may determine how patients make adaptive movements and whether they can become independent in the home and community, [7] clinicians should use functional performance assessment, and not just visual-perceptual impairment, to determine spatial neglect recovery.
Spatial neglect is also associated with other cognitive symptoms affecting functional abilities and caregiver interaction, such as emotional processing dysfunction, abnormal awareness of deficits (anosognosia for hemiplegia [7, 13] ) and delirium. [14]
Patient education
Family members involved in patient care should be well educated in the various aspects of spatial neglect and its implications for day-to-day functioning. Family members may assume that pathologically abnormal spatial behavior is a lack of motivation, depression, or even personality changes or psychosis, because understanding where we are in the 3-D world is a very basic aspect of reality-testing to most lay people. Also, lay people are not accustomed to thinking of spatial computations as mental operations. Families, paid caregivers, and patients should be made aware that even after the more dramatic symptoms of spatial neglect improve, patients may still have functional problems, including difficulty with complex navigation in familiar and unfamiliar environments and safe driving.
Etiology
Causes of spatial neglect include stroke, traumatic brain injury, brain tumors, and aneurysm. Rarely, neurodegenerative diseases can cause neglect symptoms. [15]
People with injury to either side of the brain may experience spatial neglect, but neglect occurs more commonly in persons with brain injury affecting the right cortical hemisphere, which often causes left hemiparesis. [2]
Spatial neglect is not only associated with right parietal stroke. It is commonly associated with lesions of the inferior parietal lobule or temporo-parietal region, but also with lesions of the superior temporal cortex, or frontal lobe. Less common are lesions of the subcortical regions, including the basal ganglia, thalamus, and cingulate cortex. [16] Subcortical damage can definitely result in disabling spatial neglect, and white matter disruption in particular is likely to contribute to development of spatial neglect. [17] However, both functional changes in dynamic brain networks and structural lesions are likely to contribute to the pathological spatial bias seen in spatial neglect. [18] This may explain why patients with very similar anatomic injury may present with different spatial neglect symptoms.
Mechanisms and Morbidities in Spatial Neglect
Different stages of spatial processing may be dysfunctional with spatial neglect. Thus, we can observe problems with Where spatial function: [5] both left-sided awareness (the ability to detect and perceive) and stored visual-spatial knowledge about topography.
-
Perception-attention - In the absence of primary sensory deficits, people with spatial neglect may have disordered awareness of events occurring on the neglected side. [3]
-
Imagery/representation - Even when no external stimuli are present, people with spatial neglect may have difficulty maintaining the left side of an internal map or image or other spatial knowledge pertaining to the environment, objects, body, or other reference frames. [3] The left side map may become distorted or the information may be degraded.
As above, the clinician has to be specifically alert to spatial-motor Aiming deficits in spatial neglect. These spatial "output" problems include the following:
-
Motor intentional Aiming deficits - People with spatial neglect may have trouble with activating or directing actions contralesionally, or when any part of the body is in the contralesional space. Thus, if the (good) right hand is in left space after a right brain stroke, it may squeeze less forcefully than when it is in right space. Patients with spatial neglect may also be slow to act in a contralesional direction or in contralesional space, and their motor persistence may also be spatially asymmetric.
Other manifestations of spatial neglect and associated signs:
-
Personal neglect - Individuals may not normally attend to the left side of their body. For example, after a right brain stroke, a woman may not put makeup on the left side of her face.
-
Self-monitoring - People with spatial neglect may be unaware of deficits such as hemiparesis (anosognosia) or may be unconcerned about their deficits (anosodiaphoria). This symptom is distinct from psychological denial.
-
Emotional processing - After a right-hemisphere stroke, individuals may have difficulty making appropriate emotional facial expressions and may lack normal affect or vocal intonation. At times, these signs can be mistaken for post-stroke depression. Patients may also have difficulty representing emotional knowledge (disordered emotional semantics) or perceiving the meaning of the emotional facial expressions or emotional vocal prosody of others.
-
Arousal - Hypoarousal may be associated with spatial neglect
Epidemiology
Reported overall frequency of spatial neglect in the United States is estimated to be anywhere from 13–81% in people who have had a right-hemisphere stroke, although 2 studies reported an overall rate of approximately 50%. [2] The frequency of spatial neglect may increase with age, but in one study did not seem to differ between men and women. [13] International frequency of spatial neglect is not known. Caucasians are over-represented in clinical studies of spatial neglect, and the frequency of spatial neglect in those of low socio-economic status, and under-represented racial and cultural groups, is presently unknown and needs to be evaluated.
Prognosis
Although neglect may be seen at baseline, obvious symptoms improve rapidly within the first few days. The potential mechanisms include reperfusion of the penumbral area and resolution of cytotoxic edema and other factors. Many patients with neglect show early improvement. However, as many as two-thirds of patients with spatial neglect on impairment tests have persistent deficits.at 8–9 days. [19] At 3 months, the NIH Stroke Scale detects neglect symptoms in 9.1% of patients. [20] Because the NIH Stroke Scale does not sample functional performance, this is likely to underestimate chronic neglect prevalence.
Patients who demonstrate symptoms of spatial neglect would be expected to benefit from referral for outpatient treatment with speech therapy, occupational and physical therapy, [18] neuropsychological therapy, or a combination of these referrals. Even if patients are seen as outpatients after obvious signs of spatial neglect appear to have abated, spatial bias may be present in functional tasks that cannot be detected by interacting with the patient briefly in the office environment. Whether people with spatial neglect fully recover is controversial. Although symptoms on bedside testing abate in many patients, functionally important bias, for example, limiting safety or community mobility, [10] may persist.
Even if we examine only the period days and weeks after stroke, the cost to individuals and to society of spatial neglect is considerable. Spatial neglect may greatly increase morbidity and the risk of acute and chronic complications of stroke (eg, hip fracture). It is associated with a longer acute hospital stay, [2, 21] , a higher risk of falls, more rehospitalizations after discharge to post-acute care, and higher rates of discharge to skilled nursing settings. Stroke patients with spatial neglect after stroke experience less functional gain after rehabilitation, despite staying longer during inpatient rehabilitation. This difference is not accounted for by their overall stroke severity, as patients matched to their level of disability on inpatient rehabilitation admission improve more rapidly. It is possible that this difference is accounted for by the effect of the neglect itself on body movements and body awareness. [22] Family caregivers of patients with spatial neglect reported that their loved ones required more than 20 hours daily of care, most of which was required supervision. [23] This contrasted with an average of 13.2 hours of care daily for similarly disabled stroke patients without spatial neglect. This considerable requirement to provide supervision can obviously account for increased caregiver burden caused by spatial neglect.
History and Physical Examination
Spatial neglect is commonly observed after cerebral infarction or hemorrhage. Because of associated abnormal self-monitoring (anosognosia), individuals usually do not report attention or perceptual problems. Thus, the disorder must be detected via clinical observation and testing. A complete neurologic evaluation by a thorough and knowledgeable clinician is needed to document the presence of the syndrome and even of the underlying stroke that caused it; a cursory examination in a nonaphasic patient would be unlikely to demonstrate symptoms of spatial neglect.
Spatial neglect symptoms are often first observed by caregivers or therapists, who may note personal neglect (failure to groom or clothe the contralesional side) or spatial motor Aiming neglect symptoms (may not use the contralesional limb despite adequate motor strength, or may not explore left space). Clinicians may observe the following:
-
In acute care settings, patient may lie in bed or sit in a wheelchair with the head and eyes turned to the extreme ipsilesional side, usually the right. A patient may have difficulty maintaining a normal posture (may be tilted or crooked in the bed); the contralesional leg may dangle off the bed.
-
When approached from the left, patients may bizarrely orient and reply to the right, away from the examiner addressing them (allesthesia or allochiria).
-
People with spatial neglect may navigate their wheelchairs or veer when ambulating in a rightward-biased manner; alternately, they may collide with doorways or objects on the left.
-
Spatial neglect of Where perceptual-attentional or representational types, or Aiming motor-intentional types may affect several regions of contralesional space; patients may have problems with near space, within reaching distance (peripersonal neglect), or space beyond reaching distance (extrapersonal neglect).
-
Patients with spatial neglect may deny ownership of their contralateral limb, stating that it belongs to someone else (asomatognosia); they may express dislike of the paralyzed limb (misoplegia). They may report bizarre sensations or illusions such as insisting “someone is sitting on” their left arm.
-
Patients may deny a neurologic problem (anosognosia), underestimate the severity or implications of their deficit, or fail to express sadness or anger about their difficulties and losses (anosodiaphoria); anosognosia particularly impairs participation in rehabilitation.
-
Patients may make dangerous errors in neglecting the left side of the body; the left arm may be dragged or folded behind the back; patients who previously reliably reported angina may not report left chest pain in the presence of electrocardiographic changes consistent with ischemia; infiltrated IV sites, deep venous thrombosis affecting the left leg, or skin breakdown/infection affecting the left body may go unnoticed.
Differential Diagnosis
Conditions to consider in the differential diagnosis of spatial neglect include the following:
-
Complex partial seizures
-
Cortical basal ganglionic degeneration
-
Multiple sclerosis
-
Wallenberg (lateral medullary stroke) syndrome - Lateropulsion may produce an abnormal bed posture
-
Other stroke syndromes
-
Primary visual or motor systems abnormality - Such as cortical blindness or spinal cord abnormality
-
Vestibular abnormality
-
Posterior cortical atrophy - A neurodegenerative disorder that can be associated with spatial neglect
-
Conversion disorder
-
Migraine accompaniment
Lab Studies
Laboratory tests are determined based on the neurologic disorder causing the cortical or subcortical-cortical deficit (eg, stroke, tumor, aneurysm) and vary accordingly.
Check vitamin B-12 levels, thyrotropin levels, and total thyroxine levels if memory impairment accompanies spatial neglect; perform these tests for all patients, even if diagnosed with an acute neurologic syndrome. Elevated homocysteine levels should not be interpreted as idiopathic in stroke patients unless vitamin B-12 deficiency has been excluded as a possible cause.
Check rapid plasma reagent values in patients with memory disorder, especially when associated with stroke, to evaluate for potentially treatable secondary conditions. Although false-negative and false-positive results occur, false-positive results may also be clinically relevant (eg, for connective-tissue disease).
Imaging Studies
Computed tomography (CT) scanning or magnetic resonance imaging (MRI) is indicated even if the clinical picture is otherwise entirely consistent with a right-middle cerebral artery stroke syndrome, because subdural hematomas, brain tumors, or other mass lesions occasionally mimic a stroke. Brain imaging will help to determine whether a patient with spatial neglect after head trauma had an accident because of a stroke, as the stroke may have precipitated a fall or motor vehicle accident.
Contrast-enhanced MRI is generally nontoxic and increases the sensitivity of the technique for detecting the above diagnostic confounds. CT scanning alone is adequate to detect hemorrhage, but it is insufficiently sensitive to detect some other lesions seen with MRI. Diffusion-weighted MRI distinguishes acute ischemia from chronic infarction.
Magnetic resonance angiography, conventional angiography, or functional imaging, such as single-photon emission CT or positron emission tomography (PET) scanning, may be required for the management of stroke, brain tumor, or another primary brain disorder causing spatial neglect.
Neurologic Exam
A complete neurologic examination needs to be performed. This must include a complete test of higher cortical function at the bedside. Tests of right and left hemisphere function should be performed. Specific tests for neglect often include the following:
-
Line bisection test
-
Letter cancellation test
-
Drawing and copying
-
Reading and writing
-
Sensory tests - Involving double-simultaneous stimulation for extinction in the visual, auditory, somatosensory, or motor modalities
As noted in the Introduction, paper-and-pencil tests, which were once the clinical standard, have been demonstrated to be less acceptable and useful than measures predictive of spatial neglect-related disability such as structured, semiquantitative observation of functional tasks. [12] This kind of assessment is performed by a therapist trained to judge performance reliably, similar to administration of the NIH Stroke Scale. The therapist observes the patient to dress, eat, and transfer, among other tasks, during the examination.
If paper-and-pencil tests are used, a test that has demonstrated ability to predict spatial neglect-related disability is needed. The Behavioral Inattention Test-conventional subtest has this demonstrated predictive value. [11] A disadvantage of using this test is that it takes about 15 minutes to administer. [24]
Line bisection test
Line bisection tests are easy, universally available bedside tests to screen for the presence of hemispatial neglect that take only a few seconds to perform. (See the image below.)
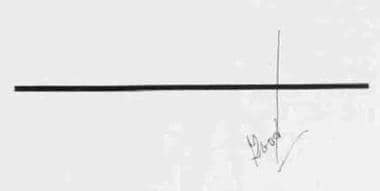 Line bisection task. A male patient is asked to "mark the center of the line," which the examiner presents centered with respect to his head and body. The patient writes "good" on the sheet when asked "How did you do?", reflecting unawareness of his significant rightward bias. (Patient without left hemianopia.)
Line bisection task. A male patient is asked to "mark the center of the line," which the examiner presents centered with respect to his head and body. The patient writes "good" on the sheet when asked "How did you do?", reflecting unawareness of his significant rightward bias. (Patient without left hemianopia.)
Detailed assessment of a patient's ability to bisect lines is ideally accomplished using several trials with different line lengths greater than 22 cm.
Neglect is more apparent when the lines are placed in the contralesional body or head space.
The lines should be as long as possible (eg, the entire span of a page) because spatial neglect is more apparent when longer lines are used.
Cancellation task
The ability to cancel an array of lines or other stimuli may be used. [25] (See the image below.) A classic study in the Lancet revealed that omissions while completing this simple task were more predictive of disability than hemiparesis or aphasia after stroke. [26]
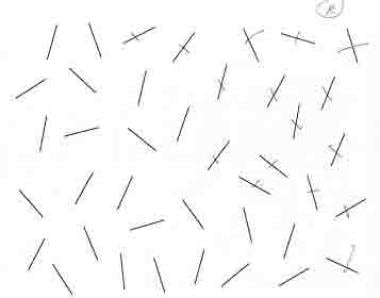 Cancellation task (Albert, 1973). The patient is presented with an array of lines scattered on a piece of paper centered with respect to head and body space and is asked to "cross out all of them." When the patient stops canceling, he or she is prompted "Did you get all the lines?" Patient neglects to cancel stimuli in left space.
Cancellation task (Albert, 1973). The patient is presented with an array of lines scattered on a piece of paper centered with respect to head and body space and is asked to "cross out all of them." When the patient stops canceling, he or she is prompted "Did you get all the lines?" Patient neglects to cancel stimuli in left space.
Double-simultaneous stimulation
Although some authors have separated extinction of contralesional stimuli to double-simultaneous stimulation from spatial neglect, this phenomenon may be categorized as a symptom of spatial neglect. Deficits in stimulus detection and stimulus awareness are observed in spatial neglect under a number of circumstances, and extinction to double-simultaneous stimulation is simply a more sensitive indicator of pathological spatial unawareness, effectively separating problems with stimulus detection due to spatial neglect from problems with stimulus detection due to unilateral sensory deficit. Testing for extinction using double-simultaneous stimulation is performed because patients may be able to detect single stimuli on the right and left hemifields but not double-simultaneous stimuli in both hemifields.
In testing for extinction using double-simultaneous stimulation, examiners may find that patients are able to detect single stimuli in the right and left hemifields, but not double-simultaneous stimuli presented in both hemifields. A contralesional stimulus may be detected when it is presented alone, but patients with spatial neglect may not perceive a contralesional stimulus when it is simultaneously presented with an ipsilesional stimulus. This may occur simultaneously with visual, tactile, or auditory modalities. [3]
At the bedside, extinction to double-simultaneous stimulation can be tested by asking the patient to count fingers presented to both hemifields, making a sound such as snapping fingers near both of the patient’s ears, or touching both of the patient’s hands. Extinction cannot be tested if a patient is completely unable to detect a single stimulus in the contralesional space due to sensory deficit.
Drawing
Although time consuming, testing the ability of the patient to draw, either by having the patient draw from memory (eg, draw-a-person task) or by having the patient copy the examiner's production (see the image below), may be one of the most sensitive means of detecting spatial neglect.
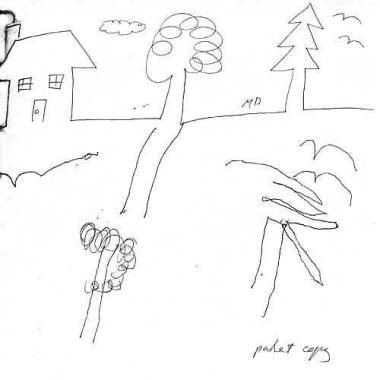 Copying a drawing. The examiner draws a simple scene with a house and 2 trees (top of picture) and asks a female patient to "copy my drawing exactly." The sample for copying is presented centered in the patient's body space, but her attempt to copy (bottom) includes only the right side of the rightward-most parts of the scene. Note that the left neglect affects not only the left side of the page (the house is omitted), but also the left side of objects within the page. (The round tree is to the left of the pine tree, but the left side of the pine tree is still missing.)
Copying a drawing. The examiner draws a simple scene with a house and 2 trees (top of picture) and asks a female patient to "copy my drawing exactly." The sample for copying is presented centered in the patient's body space, but her attempt to copy (bottom) includes only the right side of the rightward-most parts of the scene. Note that the left neglect affects not only the left side of the page (the house is omitted), but also the left side of objects within the page. (The round tree is to the left of the pine tree, but the left side of the pine tree is still missing.)
Additional tests
The patient can be observed to see if he or she has evidence of personal (body) neglect (eg, asymmetric shaving, grooming). It is interesting that some clinical practitioners, although experienced, are not attentive to pathologic asymmetry of grooming, and will insist these errors are related to hemiparesis or hemianopia. In this case, although this test does not yield a formal score, it can be useful to demonstrate body neglect by asking the patient to close his or her eyes while the examiner puts innocuous stimuli such as pieces of masking tape on various areas of the left and right body, being careful to make sure the tape is within easy reach of the good hand. This bedside test, similar to a published test for personal neglect, [27] will usually convince the skeptic that the patient with personal neglect after right brain stroke can look in the left space, but does not explore the left body. Reading assessment can be useful, particularly for planning occupational and vocational rehabilitation. When reading English, patients with spatial neglect may not begin reading at the left margin; rather, they may start in the middle of the page. When asked to identify single words, they may omit left-sided letters so that "blueberry" may be read as "berry" (neglect dyslexia). Asking a patient to read numbers may be an especially sensitive way to detect neglect dyslexia; the examiner can write a few large-magnitude numbers on a piece of paper (e.g. “2,113,461”), and ask the patient to read the number (a patient with neglect dyslexia may read “661”).
Informal anosognosia testing is performed by asking the patient about his or her presentation to the hospital and the symptoms. For example, questions may include the following: "Are you weak anywhere?" It is especially effective to do this immediately after testing that reveals a deficit. Patients may be aware of some symptoms and unaware of others; a patient may be admit to have done poorly on a memory test, for example, but state that he did well on a test for spatial neglect.
Distinguish neglect and hemianopia (which may coexist) by directing the patient's gaze into the preferred hemispace (eg, right, after a right brain injury). In many people with spatial neglect, the ability to detect visual stimuli in the contralesional retinal hemifield improves when the left and right visual hemifield are tested while they gaze into the non-neglected hemispace. In other words, a patient who is unable to see a left-sided stimulus while looking straight ahead, may be able to see a stimulus presented to approximately the same retinal area when she is looking to right of her body midline. If a stimulus can be detected in the left retinal hemifield by manipulating the body space in which the stimulus is presented, the patient is less likely to have true hemianopia. [28]
Approach to the Care of Spatial Neglect Patients
The most important step in treatment of spatial neglect is identification of spatial neglect symptoms through an assessment. As above, assessment is needed that assigns a quantitative score directly related to the degree of functional disability. This means that a simple screen like the line bisection test or cancellation test (reviewed above) is only useful to alert the team that the patient needs further assessment—these tests cannot be used to assign and follow treatment.
As many as 4 out of 5 patients with spatial neglect (usually patients with milder symptoms) are not documented as having symptoms. [9] It is, of course, very likely that patients who do not receive the formal diagnosis of spatial neglect do not receive the right care plan. Assessment for spatial neglect with a measure that predicts functional disability is thus a likely process marker of quality care. This assessment can be performed by an occupational therapist, physical therapist, cognitive neurologist or neuropsychologist. When patients receive this kind of assessment, it indicates that a stroke team is specialized, patient-centered, and aware of barriers affecting community re-entry.
The American Heart Association (AHA) consensus recommendations for stroke rehabilitation [29] included a Class II recommendation for spatial neglect evaluation among recommendations for Assessment of Cognition and Memory. However, information about the presence of spatial neglect will also obviously help the physician to select best medications—because these patients are probably at higher risk of delirium [30] , the prescriber should avoid sedatives and other deliriants. The presence of spatial neglect will also help the team to create a falls prevention plan, and may also help with other aspects of health self-management such as teaching medication self-administration. The presence of spatial neglect, because it is often associated with unawareness of deficit, means that self-reported symptoms and goals of treatment should be supplemented with clinician and caregiver observations to ensure that important issues are addressed. [31] For example, a patient with spatial neglect may deny pain, but grimace whenever the caregiver moves the left leg, suggesting that he is unable to report the pain verbally, but that it still mayneed medical evaluation.
Treatment for spatiel neglect includes 1) management and compensation, 2) restorative therapies, and 3) caregiver, family, and patient support.
Management and compensation for spatial neglect
The American Heart Association and the American Occupational Therapy Association (AOTA) provide recommendations for spatial neglect. [29, 32]
-
Visual scanning training. Patients learn to do a conscious visual search of the neglect space in this intervention, usually administered by occupational therapists. Spatial cuing, and feedback to train increased amplitude of eye and head movements toward the neglected space, are essential components of this approach. [33] Both the AHA and AOTA groups included this intervention among recommended approaches. Limitations of this approach include failure to generalize: a patient who is able to scan leftward while reading after receiving this training may still fail to scan leftward when crossing the street. The approach also relies upon self-implementation and engagement in the therapeutic program: patients with unawareness of deficit may not respond.
Restorative therapies
See the list below:
-
Prism adaptation treatment. Both the AHA and the AOTA listed this treatment approach first among recommended interventions. In this treatment, patients make repeated movements with the good hand and arm while wearing binocular optical prisms. The prisms shift what they see about 11 degrees into the preferred (ipsilesional) field; unconsciously, patients increase their propensity to move into the neglected field. Patients under treatment do not need to wear the prisms at other times. The standard protocol is ten sessions over fourteen days. [34] Advantages of this treatment include its effectiveness (>20 studies demonstrate it improves functional independence [35] ), feasibility, and low cost. It may be particularly effective in stroke survivors with frontal brain lesions and hemiparesis. [36] The major disadvantage of this treatment is that although meta-analysis suggests it results in a large magnitude of improvement in spatial neglect compared to other treatments, [37] it is not yet widely implemented. When prescribing occupational therapy, physicians need to request prism adaptation treatment specifically, and ensure that the occupational therapist has been trained to administer the evidence-based protocol. Prism adaptation treatment should not be confused with prism exposure, in which prism lenses are worn by the patient during all waking hours without specific training: controlled studies supporting this approach are not available.
-
Other approaches. No other approaches were recommended by both the AHA and AOTA guidelines, however, three other interventions were listed in both resources for which there is demonstrated functional benefit in randomized controlled studies:
See the list below:
- Limb activation. In this approach, patients receive sensory or verbal cues to make movements with the affected limbs in the neglected space during therapy sessions. By moving the weaker limb on the neglected side, spatial motor-intentional systems may be activated and, indirectly, spatial perceptual-attentional Where function as well. [38] The treatment is usually administered by an occupational therapist and requires no specific equipment, although devices to facilitate left-sided movement cuing are available. [39, 40] Although different protocols have been used for this treatment, a total of 14–20 hours of treatment over 12 weeks in one or two weekly sessions is appropriate. Advantages to this treatment are its simplicity and feasibility. The disadvantage is that, like prism adaptation treatment, few occupational therapists are trained to use this approach. Therapists report that this treatment is labor-intensive, as they need to remember to implement the movement cuing, which interrupts the chain of activities in training dressing, bathing, or other therapy goals during treatment sessions.
- Alternate approaches. Optikinetic stimulation, virtual reality, mental imagery, and neck vibration combined with prism adaptation are also reviewed in the AHA and AOTA guidelines as supported by limited evidence. Although these approaches allow for a second- or third-line behavioral treatment plan, optikinetic stimulation, virtual reality, and neck vibration are dependent on available equipment, and few therapists are formally trained to use any of these approaches, thus their feasibility is questionable.
- Medications. See below: Medications
Caregiver, family, and patient support
See the list below:
-
Spatial neglect is a cognitive disorder. However, interacting with the 3-dimensional world is fundamental to every daily life activity, and so spatial neglect can result in a much more profound disruption of self-care and independence than other stroke-related thinking problems. [26] One study indicated that informal family caregivers of patients with spatial neglect spend more than 20 hours daily in supervision and direct care. Because about half of stroke survivors have spatial neglect during the weeks and months after stroke, [2] spatial neglect is thus responsible for very significant burden on caregivers and our society. [23]
-
The optimal caregiver, family, and patient supports needed for adjustment and return to function and freedom are not yet established. However, standard principles to improve burden, strain, and quality of life for caregivers of stroke survivors include providing interventions for both the caregiver alone, and the caregiver-patient dyad, providing resources for skill-building together with psycho-education, tailoring interventions to caregiver needs and providing interventions on an individual basis, providing telephone and web access when face-to-face intervention is not feasible, and providing interventions over 5–9 sesions. [41]
Consultations
Consultation with a skilled optometrist or ophthalmologist specialized in low vision assessment may be considered in the presence of hemianopia. A detailed bedside examination is preferred over automated methods of assessing visual-field deficits; neglect may otherwise be misinterpreted as visual field deficit. Visual assessment and vision therapy may be particularly useful when patients have both ocular disorders and spatial neglect, because these disorders may interact. [42]
Consultation with a neuropsychologist can be helpful for family and caregiver counseling and for transition to long-term stages of recovery and potential community reintegration, as well as for dealing with issues of psychological adjustment by the patient, who may have intact emotional reactions but an impaired ability to communicate emotionally. A neuropsychologist should be chosen who is knowledgable about assessment and treatment of right brain disorders; this is not always part of clinical neuropsychological training.
Transitions to postacute and chronic stages of recovery can be particularly challenging for stroke survivors with spatial neglect. It is difficult for their families to anticipate the difficulties they will have, purely as a result of their stroke, in taking medications accurately, managing transfers and ambulation safely, and reintegrating into their social and community roles. Focusing planned postacute follow-up on avoiding these care transition problems may mean transitional consultation with a case manager, nurse, occupational therapist or speech-language pathologist, or psychologist, depending on which professionals are available and most skilled in particular communities.
People with mild spatial neglect symptoms living in the community, and their caregivers, may benefit greatly from neuropsychiatric consultation and couples or family therapy to adjust to chronic disability. Caregivers of people with spatial neglect are at higher risk of caregiver burden, perhaps because unawareness of deficit and safety problems increase the need for patient supervision. [23]
Medications
Although cholinergic anddopaminergic medications for spatial neglect are an exciting and developing area, this approach has not yet become standard care. [43, 44] The 2010 VA/DoD Clinical Practice Guideline for Management of Stroke Rehabilitation [45] recommends considering cholinesterase inhibitors (rivastigmine, galantamine, donepezil) for vascular cognitive impairment in the doses and frequency used for Alzheimer disease, although no medication recommendations for spatial neglect are made in this document. In the AHA guidelines, recommendations for cholinesterase inhibitors for cognitive enhancement after stroke is a Class IIb recommendation (utility is unclear).
An established practice is to withhold anticholinergic medications, antidopaminergic medication (eg, for gastrointestinal indications), sedatives, and hypnotics in these patients unless absolutely necessary. These agents are likely to adversely affect the symptoms of spatial neglect and eventual functional recovery. Similarly, phenytoin is relatively contraindicated. Benzodiazepines are reported to unmask spatial neglect symptoms that previously recovered [46] and so are also contraindicated.
Patients in whom other conditions make taking the above medications necessary, must be carefully monitored and their spatial neglect symptoms periodically reevaluated.
No current clinical literature supports a benefit related to the use of modafinil in patients with spatial neglect. Although methylphenidate was helpful for spatial neglect in a small study, [47] it was used in combination with behavioral prism adaptation treatment, and using this agent without prism adaptation treatment is questionable.
Safety Issues
The most important issue that may have legal implications in cases of spatial neglect is driving. Patients with spatial neglect may not be allowed to drive, for their safety and the safety of the others. Unfortunately, how people with driving disability can be identified is not clear, short of an on-road standard driving evaluation by consultation through a clinical driving program. Although visual-spatial and continuous performance assessments such as the Useful Field of View [48] may be excellent predictors of driving ability in aged people, prospective psychometric development of instruments to predict driving errors in people with mild spatial neglect has not yet been performed.
Patients who have had acute spatial neglect, even if the symptoms appear to have resolved, should undergo on-road evaluation before returning to driving.
Patients should undergo an occupational/vocational rehabilitation evaluation before returning to any kind of work that involves handling machines or tools that may cause injury to self or others.
Dangerous tools, firearms, and other environmental risks should be removed from the homes of patients with spatial neglect who are homebound but are not constantly supervised. The author has observed a number of accidents in the home and workplace when patients and families were not compliant with management recommendations.
Vocational disability in spatial neglect may extend to other, non–safety-related issues. Difficulty reading left-sided material (neglect dyslexia) may lead to embarrassing errors in financial, academic, or other detail-oriented work. Spatial bias may also affect social behavior (effective audience interaction during presentations), and social-emotional changes are, of course, common after right brain stroke. A cognitive remediation program may be extremely valuable if a legal dispute arises between a stroke survivor and his or her employer about job fitness. If it is hard to locate a cognitive remediation program, one can sometimes be identified among resources primarily intended for individuals with traumatic brain injury or even developmental disabilities, and may offer referral resources to a job coach specialized in right brain neurorehabilitative challenges.
-
Line bisection task. A male patient is asked to "mark the center of the line," which the examiner presents centered with respect to his head and body. The patient writes "good" on the sheet when asked "How did you do?", reflecting unawareness of his significant rightward bias. (Patient without left hemianopia.)
-
Cancellation task (Albert, 1973). The patient is presented with an array of lines scattered on a piece of paper centered with respect to head and body space and is asked to "cross out all of them." When the patient stops canceling, he or she is prompted "Did you get all the lines?" Patient neglects to cancel stimuli in left space.
-
Copying a drawing. The examiner draws a simple scene with a house and 2 trees (top of picture) and asks a female patient to "copy my drawing exactly." The sample for copying is presented centered in the patient's body space, but her attempt to copy (bottom) includes only the right side of the rightward-most parts of the scene. Note that the left neglect affects not only the left side of the page (the house is omitted), but also the left side of objects within the page. (The round tree is to the left of the pine tree, but the left side of the pine tree is still missing.)
Tables
What would you like to print?
- Overview
- Etiology
- Mechanisms and Morbidities in Spatial Neglect
- Epidemiology
- Prognosis
- History and Physical Examination
- Differential Diagnosis
- Lab Studies
- Imaging Studies
- Neurologic Exam
- Approach to the Care of Spatial Neglect Patients
- Consultations
- Medications
- Safety Issues
- Show All
- Media Gallery
- References








