Practice Essentials
Paraneoplastic encephalomyelitis (PEM) is a multifocal inflammatory disorder of the central nervous system (CNS) associated with remote neoplasia. [1] Frequently, the disorder is accompanied by subacute sensory neuronopathy (SSN) due to involvement of the dorsal root ganglia. Anti-Hu antibodies may be detected in both of these conditions. Although various malignancies have been reported in PEM, 80% of cases are associated with bronchial cancer, typically small cell lung carcinoma. [2] Neurologic manifestations commonly precede the diagnosis of cancer, although variable presentations have been reported. Symptoms usually progress over the course of weeks to months, reaching a plateau of neurologic disability. Neurologic impairment may be more debilitating than the associated cancer. No effective therapeutic approaches have been established, although immunosuppressive therapies are commonly used. See the images below.
Pathophysiology
Neurologic dysfunction probably results from an autoimmune reaction directed against onconeural antigens in the human nervous system. Polyclonal immunoglobulin G (IgG) anti-Hu antibodies or type 1 antineuronal nuclear antibodies are most prevalent (~50%), although several other circulating autoantibodies have been identified. Some patients have no identifiable paraneoplastic antibodies. These markers of paraneoplasia have an undetermined pathogenic role. Cytotoxic T cell–mediated neuronal damage is suspected, although no animal models have been developed to confirm this. [3]
Almost all cases of PEM with anti-Hu antibodies are related to small-cell lung carcinoma. These antibodies react with a group of 35- to 40-kilodalton neuronal RNA-binding proteins, including HuD [4] , PLE21/HuC, and Hel-N1. Nuclear and cytoplasmic staining of CNS neurons demonstrates the presence of these antibodies. A ubiquitous protein, HuR, is also an antigenic target. The neuronal proteins are homologous to the embryonic lethal abnormal visual (ELAV) protein in Drosophila species. Anti-Hu antibodies may alter the production of these proteins, which are essential for the development, maturation, and maintenance of the vertebrate nervous system. Intrathecal synthesis of anti-Hu antibodies may represent an autoimmune cross-reaction with neurologic tissue, triggered by a remote carcinoma. Recent work has focused on the detection of neuron-specific ELAV mRNA in peripheral blood of SCLC patients using real-time quantitative polymerase chain reaction (PCR). [5]
In one report, a subset of patients with limbic encephalitis associated with a systemic neoplasm previously attributed to antibodies against voltage gated potassium channel antibodies actually recognize LGI1 protein complex epitopes and do not represent a channelopathy. The authors propose the term limbic encephalitis associated with LGI1 antibodies. [6]
Other PEM antibodies include anti-CV2, anti-Yo, anti-Ma1, anti-Ta or anti-Ma2, anti-LGI1, and several other atypical antibodies. The targets of such antibodies may be quite varied, including neuropil and intraneuronal sites.
Nonneuronal autoantibodies, such as antinuclear antibodies and anticytoplasmic antibodies, are frequently detected in cases with anti-Hu antibodies or anti-Yo antibodies. The presence of such nonneuronal autoantibodies, however, does not correlate with particular clinical characteristics. [7]
Voltage-gated potassium channel antibodies may be associated with nonparaneoplastic limbic encephalitis.
Recent reports have noted detection of the prion-related 14-3-3 protein [8] and of herpes simplex virus [9] by PCR in the cerebrospinal fluid (CSF) of patients with PEM. The significance of these findings is unclear.
Epidemiology
Frequency
The incidence of paraneoplastic encephalomyelitis (PEM) is unknown. PEM affects approximately 0.4% of patients with bronchial carcinoma. Increased recognition of clinical manifestations may provide estimates of incidence in the future.
Mortality/Morbidity
PEM has a variable and unpredictable course.
Progressive evolution of neurologic dysfunction may lead to coma and death in a few patients.
Most patients experience severe neurologic impairment with susceptibility to related medical complications.
Race-, sex-, and age-related demographics
No racial predilection has been reported.
Anti-Hu–associated PEM has a slight female predominance. [10]
PEM occurs most frequently in middle-aged or older adults with small-cell lung carcinoma. It may occur in younger individuals with other types of cancer.
Prognosis
The clinical course of paraneoplastic encephalomyelitis (PEM) is unpredictable, although the titer of anti-Hu antibodies has been suggested as a prognostic indicator. Elevated titers have been associated with worse neurologic outcome and death.
-
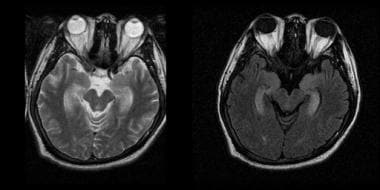
Paraneoplastic encephalomyelitis.
-
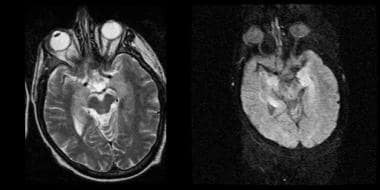
Paraneoplastic encephalomyelitis.
-
Mesial temporal hyperintensity demonstrated on T2-weighted (left) and fluid-attenuated inversion recovery (FLAIR, right) MRI.