Practice Essentials
Acute liver failure is an uncommon condition in which rapid deterioration of liver function results in coagulopathy, usually with an international normalized ratio (INR) of greater than 1.5, and alteration in the mental status (encephalopathy) of a previously healthy individual. Acute liver failure often affects young people and carries a very high mortality.
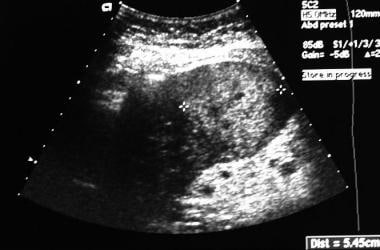
The ultrasonogram shows a hyperechoic mass representing hepatocellular carcinoma.
Signs and symptoms
Acute liver failure is a broad term that encompasses both fulminant hepatic failure and subfulminant hepatic failure (or late-onset hepatic failure). The term fulminant hepatic failure is generally used to describe the development of encephalopathy within 8 weeks of the onset of symptoms in a patient with a previously healthy liver. The term subfulminant hepatic failure is reserved for patients with liver disease for up to 26 weeks before the development of hepatic encephalopathy.
Signs and symptoms of acute failure may include the following:
-
Encephalopathy
-
Cerebral edema: May lead to signs of increased intracranial pressure (ICP) (eg, papilledema, hypertension, bradycardia)
-
Jaundice: Often present but not always
-
Ascites: Potential for hepatic vein thrombosis with rapid development in the presence of fulminant hepatic failure accompanied by abdominal pain
-
Right upper quadrant tenderness: Variably present
-
Change in liver span: May be small due to hepatic necrosis or may be enlarged due to heart failure, viral hepatitis, or Budd-Chiari syndrome
-
Hematemesis or melena: Due to upper gastrointestinal (GI) bleeding
-
Hypotension and tachycardia: Due to reduced systemic vascular resistance
See Presentation for more detail.
Diagnosis
The most important step in the assessment of patients with acute liver failure is to identify the cause, because certain conditions necessitate immediate and specific treatment and affect prognosis. All patients with clinical or laboratory evidence of moderate or severe acute hepatitis should have immediate measurement of prothrombin time (PT) and careful evaluation of the mental status. The presence of PT prolongation or mental status changes is grounds for hospital admission.
Laboratory testing
-
Complete blood count: May reveal thrombocytopenia
-
Coagulation studies: PT and/or international normalized ratio (INR)
-
Liver function tests: Often elevated levels of aspartate aminotransferase (AST)/serum glutamic-oxaloacetic transaminase (SGOT), alanine aminotransferase (ALT)/serum glutamic-pyruvic transaminase (SGPT), alkaline phosphatase (ALP)
-
Serum bilirubin level: Elevated
-
Serum ammonia level: May be dramatically elevated (accuracy: arterial > venous level)
-
Serum glucose level: May be dangerously low
-
Serum (arterial) lactate level: Often elevated
-
Arterial blood gas: May reveal hypoxemia
-
Serum creatinine level: May be elevated
-
Serum free copper and ceruloplasmin levels: Low levels in Wilson disease
-
Serum phosphate level: May be low
-
Acetaminophen and acetaminophen-protein adducts levels
-
Drug screening: Consider in patients who are intravenous drug abusers
-
Blood cultures: For patients with suspected infection
-
Viral serologies: Consider for hepatitis A virus immunoglobulin M (IgM), hepatitis B surface antigen (HBsAg), hepatitis B virus anticore IgM; hepatitis C viral load testing; hepatitis D virus IgM if HBsAg is positive; in posttransplantation or immunosuppressed setting, consider studies for cytomegalovirus viremia, cytomegalovirus antigenemia, and herpes simplex virus
-
Autoimmune markers (for autoimmune hepatitis diagnosis): Antinuclear antibody (ANA), anti-smooth muscle antibody (ASMA), and immunoglobulin levels
Other studies may include the following:
-
Electroencephalography
-
Intracranial pressure monitoring
-
Percutaneous (contraindicated in the presence of coagulopathy) or transjugular liver biopsy
Imaging studies
-
Hepatic Doppler ultrasonography
-
Abdominal computed tomography (CT) scanning or magnetic resonance imaging without contrast
-
Cranial CT scanning
See Workup for more detail.
Management
The most important aspect of treatment for acute liver failure is to provide good intensive care support, including the protection of the airways. [1, 2, 3, 4, 5] Specific therapy is also dependent on the cause of the patient’s liver failure and the presence of any complications.
Pay careful attention to the patient’s fluid management and hemodynamics. It is crucial to monitor their metabolic parameters, assess for infection, maintain nutrition, and promptly recognize GI bleeding.
Pharmacotherapy
Various medications may be necessary because of the variety of complications that may occur from fulminant hepatic failure. In specific cases, antidotes that effectively bind or eliminate toxins are essential.
The following medications may be used in the management of acute liver failure:
-
Antidotes (eg, penicillin G, silibinin, activated charcoal, N-acetylcysteine)
-
Osmotic diuretics (eg, mannitol)
-
Barbiturate agents (eg, pentobarbital, thiopental)
-
Benzodiazepines (eg, midazolam)
-
Anesthetic agents (eg, propofol)
Surgery
Liver transplantation is the definitive treatment for acute liver failure. In selected patients for whom no allograft is immediately available, consider support with a bioartificial liver. This is a short-term measure that only leads to survival if the liver spontaneously recovers or is replaced. [6, 7, 8, 9]
Nonbiologic extracorporeal liver support systems, such as hemodialysis, hemofiltration, charcoal hemoperfusion, plasmapheresis, and exchange transfusions permit temporary liver support until a suitable donor liver is found. However, no controlled study has shown long-term benefit.
See Treatment and Medication for more details.
Background
Acute liver failure (ALF) is an uncommon condition in which rapid deterioration of the liver function results in coagulopathy and alteration in the mental status of a previously healthy individual. Acute liver failure often affects young people and carries a very high mortality.
The term acute liver failure is used to describe the development of coagulopathy, usually with an international normalized ratio (INR) of greater than 1.5, and any degree of mental alteration (encephalopathy) in a patient without preexisting cirrhosis and with an illness of less than 26 weeks' duration.
Acute liver failure is a broad term that encompasses both fulminant hepatic failure (FHF) and subfulminant hepatic failure (or late-onset hepatic failure). Fulminant hepatic failure is generally used to describe the development of encephalopathy within 8 weeks of the onset of symptoms in a patient with a previously healthy liver. Subfulminant hepatic failure is reserved for patients with liver disease for up to 26 weeks before the development of hepatic encephalopathy.
There are important differences between FHF in children and FHF in adults. For example, in children with FHF, encephalopathy may be absent, late, or unrecognized. For a full discussion of the diagnosis and management of pediatric FHF, see Fulminant Hepatic Failure. The American Association for the Study of Liver Diseases (AASLD) has produced guidelines on the management of acute liver failure in adults. [1, 2]
Some patients with previously unrecognized chronic liver disease decompensate and present with liver failure; although this is not technically FHF, discriminating such at the time of presentation may not be possible. Patients with Wilson disease, vertically acquired hepatitis B, or autoimmune hepatitis may be included in spite of the possibility of cirrhosis, if their disease has been manifest for less than 26 weeks.
The most important step in the assessment of patients with acute liver failure is to identify the cause, as certain causes demand immediate and specific treatment (see Workup). Drug-related hepatotoxicity, especially from acetaminophen, is the leading cause of acute liver failure in the United States (see Etiology).
The most important aspect of treatment is to provide good intensive care support. Careful attention should be paid to fluid management and hemodynamics. Monitoring of metabolic parameters, surveillance for infection, maintenance of nutrition, and prompt recognition of gastrointestinal bleeding are crucial (see Treatment).
Various medications may be necessary because of the variety of complications that occur from fulminant hepatic failure. In specific cases, antidotes that effectively bind or eliminate toxins are essential (see Medication).
The development of liver support systems provides some promise for patients with FHF, although the systems remain a temporary measure and, to date, have had no impact on survival. Other investigational therapeutic modalities, including hypothermia, have been proposed but remain unproven. [10, 11]
The outcome of acute liver failure is related to the etiology, the degree of encephalopathy, and related complications (see Prognosis). Although mortality from FHF remains significantly high, improved intensive care measures and the use of orthotopic liver transplantation have improved survival from less than 20% to approximately 60%. [12, 13]
For patient education information, see the Infections Center and Digestive Disorders Center, as well as Hepatitis A (HAV, Hep A), Hepatitis B (HBV, Hep B), Hepatitis C (Hep C, HCV), and Cirrhosis.
Pathophysiology
The development of cerebral edema is the major cause of morbidity and mortality in patients with acute liver failure. [10, 14, 15] The etiology of this intracranial hypertension (ICH) is not fully understood, but it is considered to be multifactorial.
Briefly, hyperammonemia may be involved in the development of cerebral edema. Brain edema is thought to be both cytotoxic and vasogenic in origin.
Cytokine profiles are also deranged. Elevated serum concentrations of bacterial endotoxins, tumor necrosis factor–alpha (TNF-α), interleukin (IL)–1, and IL-6 have been found in fulminant hepatic failure.
Cytotoxic edema
Cytotoxic edema is the consequence of impaired cellular osmoregulation in the brain, resulting in astrocyte edema. Cortical astrocyte swelling is the most common observation in neuropathologic studies of brain edema in acute liver failure.
In the brain, ammonia is detoxified to glutamine via amidation of glutamate by glutamine synthetase. The accumulation of glutamine in astrocytes results in astrocyte swelling and brain edema. There is clear evidence of increased brain concentration of glutamine in animal models of acute liver failure. The relationship between high ammonia and glutamine levels and raised ICH has been reported in humans.
Vasogenic factors
An increase in intracranial blood volume and cerebral blood flow is a factor in acute liver failure. The increased cerebral blood flow results because of the disruption of cerebral autoregulation. The disruption of cerebral autoregulation is thought to be mediated by elevated systemic concentrations of nitric oxide, which acts as a potent vasodilator.
Multisystem organ failure
Another consequence of fulminant hepatic failure is multisystem organ failure, which is often observed in the context of a hyperdynamic circulatory state that mimics sepsis (low systemic vascular resistance); therefore, circulatory insufficiency and poor organ perfusion possibly either initiate or promote complications of fulminant hepatic failure.
Acetaminophen hepatotoxicity
The development of liver failure represents the final common outcome of a wide variety of potential causes, as the broad differential diagnosis suggests (see Differential Diagnosis). As with many drugs that undergo hepatic metabolism (in this case, by cytochrome P-450), the oxidative metabolite of acetaminophen is more toxic than the drug. [13, 16, 17, 18] The highly reactive active metabolite N-acetyl-p-benzoquinone-imine (NAPQI) appears to mediate much of the acetaminophen-related damage to liver tissue by forming covalent bonds with cellular proteins.
Ordinarily, NAPQI is metabolized in the presence of glutathione to N-acetyl-p-aminophenol-mercaptopurine. Glutathione quenches this reactive metabolite and acts to prevent nonspecific oxidation of cellular structures, which might result in severe hepatocellular dysfunction.
This mechanism fails in two different yet equally important settings. The first is an overdose (accidental or intentional) of acetaminophen. Acetaminophen ingestion of more than 10 g simply overwhelms the normal hepatic stores of glutathione, allowing reactive metabolites to escape.
The second and less obvious scenario occurs in a patient who consumes alcohol regularly. This does not necessarily require a history of alcohol abuse or alcoholism. Even a moderate or social drinker who consistently consumes one to two drinks daily may sufficiently deplete intrahepatic glutathione reserves. This results in potentially lethal hepatotoxicity from what is otherwise a safe dose of acetaminophen (below the maximum total dose of 4 g/d) in an unsuspecting individual. Patients with acute liver failure may have unrecognized or uncertain acetaminophen toxicity. [19]
Etiology
Numerous causes of fulminant hepatic failure exist, but hepatotoxicity due to acetaminophen and idiosyncratic drug reactions is the most common cause in the United States. For nearly 15% of patients, the cause remains indeterminate.
Viral hepatitis may lead to hepatic failure. Hepatitis A and B account for most of these cases. In the developing world, acute hepatitis B virus (HBV) infection dominates as a cause of fulminant hepatic failure because of the high prevalence of the disease.
Hepatitis C rarely causes acute liver failure. Hepatitis D, as a coinfection or superinfection with hepatitis B virus, can lead to fulminant hepatic failure. Hepatitis E (often observed in pregnant women) in endemic areas is an important cause of fulminant hepatic failure.
Atypical causes of viral hepatitis and fulminant hepatic failure include the following:
-
Paramyxovirus
Autoimmune hepatitis may also result in hepatic failure.
Hepatic failure in pregnancy
Acute fatty liver of pregnancy (AFLP) frequently culminates in fulminant hepatic failure. [21] AFLP typically occurs in the third trimester; preeclampsia develops in approximately 50% of these patients. AFLP has been estimated to occur in 0.008% of pregnancies.
The most common cause of acute jaundice in pregnancy is acute viral hepatitis, and most of these patients do not develop fulminant hepatic failure. The one major exception to this is the pregnant patient who develops hepatitis E virus infection, in whom progression to fulminant hepatic failure is unfortunately common and often fatal.
The exposure history in patients with hepatitis E is usually remarkable for travel and/or residence in the Middle East, India and the subcontinent, Mexico, or other endemic areas. In the United States, hepatitis E is relatively uncommon but must be considered in the appropriate setting.
The HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome occurs in 0.1-0.6% of pregnancies. It is usually associated with preeclampsia and may rarely result in liver failure.
Drug-related hepatotoxicity
Many drugs (both prescription and illicit) are implicated in the development of fulminant hepatic failure. Drug-induced liver injury (DILI) is a leading cause of emergent liver transplantation [22] ; in Western nations, DILI is the primary cause of acute liver failure in adults. [23] The more common agents are discussed below.
Idiosyncratic drug reactions may occur with virtually any medication. Fortunately, these appear to lead to fulminant hepatic failure only rarely, although they are the most common form of drug reaction to lead to fulminant hepatic failure (with the exception of acetaminophen poisoning). [23, 24, 25]
Acetaminophen (also known as paracetamol and N-acetyl-p-aminophenol [APAP]) may lead to liver failure as a result of intentional or accidental overdose. In the US Acute Liver Failure (ALF) study, unintentional acetaminophen use accounted for 48% of cases, whereas 44% of cases were due to intentional use; in 8% of cases, the intention was unknown. [17] Chronic alcohol use may greatly increase the susceptibility to hepatotoxicity from acetaminophen because of depleted glutathione stores. Some patients with acute liver failure have unrecognized or uncertain acetaminophen toxicity. These cases have been diagnosed by highly specific acetaminophen-cysteine adducts assay. But this assay is currently not available for routine clinical use.
Fluoroquinolones are sometimes associated with mild, transient elevations in aminotransferase levels. In particular, moxifloxacin has been identified as presenting a risk for acute liver failure. A study by Paterson et al examined the risk of acute liver injury associated with the use of moxifloxacin relative to other antibiotics. Results showed an association between moxifloxacin and an increased risk of acute liver failure among adults aged 66 years or older with no history of liver disease who were admitted to the hospital for acute liver injury within 30 days of receiving a prescription for the antibiotic. [26]
Prescription medications that have been associated with idiosyncratic hypersensitivity reactions include the following:
-
Antibiotics (ampicillin-clavulanate, ciprofloxacin, doxycycline, erythromycin, isoniazid, nitrofurantoin, tetracycline)
-
Antidepressants (amitriptyline, nortriptyline)
-
Antiepileptics (phenytoin, valproate) [25]
-
Anesthetic agents (halothane)
-
Lipid-lowering medications (atorvastatin, lovastatin, simvastatin)
-
Immunosuppressive agents (cyclophosphamide, methotrexate)
-
Salicylates (ingestion of these agents may result in Reye syndrome)
-
Others (disulfiram, flutamide, gold, propylthiouracil)
Illicit drugs that have been associated with idiosyncratic hypersensitivity reactions include the following:
-
Ecstasy (3,4-methylenedioxymethamphetamine [MDMA])
-
Cocaine (may be the result of hepatic ischemia)
Herbal or alternative medicines that have been associated with idiosyncratic hypersensitivity reactions include the following:
-
Ginseng
-
Pennyroyal oil
-
Teucrium polium
-
Chaparral or germander tea
-
Kawakawa
In October 2013, the Centers for Disease Control and Prevention (CDC) issued a warning that the weight-loss and bodybuilding supplement OxyELITE Pro was associated with severe acute hepatitis and fulminant liver failure. [27, 28]
Lo Re et al have proposed a new prognostic model to predict the risk of acute liver failure in patients with drug-induced liver injury that takes into consideration a patient's platelet count and total bilirubin level rather than the conventional use of alanine aminotransferase or aspartate aminotransferase and total bilirubin values used in Hy's law. [29] They reported a high sensitivity of predicting acute liver failure with their model as compared with the low sensitivity but high specificity when Hy's law is used.
More recently, researchers in the United Kingdom and Denmark developed a statistical outcome prediction model to support decision making in patients with acetaminophen-induced acute liver failure. [30] Variables include patients’ age, Glasgow coma scale, arterial pH and lactate levels, creatinine levels, international normalized ratio, and cardiovascular failure, as well as changes in INR and lactate levels.
Toxin-related hepatotoxicity
The following toxins are associated with dose-related toxicity:
-
Amanita phalloides mushroom toxin [31]
-
Bacillus cereus toxin
-
Cyanobacteria toxin
-
Organic solvents (eg, carbon tetrachloride)
-
Yellow phosphorus
A phalloides mushroom intoxication is much more common in Europe and in California than in the remainder of the United States.
Vascular causes
The following are vascular causes of hepatic failure:
-
Ischemic hepatitis (consider especially in the setting of severe hypotension or recent hepatic tumor chemoembolization)
-
Hepatic vein thrombosis (Budd-Chiari syndrome)
-
Hepatic veno-occlusive disease
-
Hepatic arterial thrombosis (consider posttransplant)
Metabolic causes
The following metabolic diseases can cause hepatic failure:
-
Fructose intolerance
-
Galactosemia
-
Lecithin-cholesterol acyltransferase deficiency
-
Wilson disease
Malignancies
Malignancies that can cause hepatic failure include the following:
-
Primary liver tumor (usually hepatocellular carcinoma, rarely cholangiocarcinoma)
-
Secondary tumor (extensive hepatic metastases or infiltration from adenocarcinoma, such as breast and lung, and melanoma primaries [common]; lymphoma; leukemia)
Miscellaneous
Miscellaneous causes of hepatic failure include adult-onset Still disease, heatstroke, and primary graft nonfunction in liver transplant recipients.
Epidemiology
The incidence of fulminant hepatic failure appears to be low in the United States, with approximately 2000 cases annually. Drug-related hepatotoxicity accounts for more than 50% of acute liver failure cases, including acetaminophen toxicity (42%) and idiosyncratic drug reactions (12%). Nearly 15% of cases remain of indeterminate etiology. Other causes seen in the United States are hepatitis B, autoimmune hepatitis, Wilson disease, fatty liver of pregnancy, and HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome. [32]
International statistics
In developed nations, acute liver failure has an estimated incidence of fewer than 10 cases per million people per year. [33] Acetaminophen (paracetamol) overdoses are prominent causes of fulminant hepatic failure in Europe and, in particular, Great Britain. Hepatitis delta virus (HDV) superinfection is much more common in developing countries than in the United States because of the high rate of chronic hepatitis B virus (HBV) infection.
Hepatitis E virus (HEV) is associated with a high incidence of fulminant hepatic failure in women who are pregnant and is of concern in pregnant patients living in or traveling through endemic areas. [32] These regions include, but are not limited to, Mexico and Central America, India and the subcontinent, and the Middle East.
Racial distribution of acute liver failure
Acute liver failure is seen among all races. In a US multicenter study of acute liver failure, the ethnic distribution included white persons (74%), Hispanics (10%), black persons (3%), Asians (5%), and Latin Americans (2%). [3, 17, 18]
Acute liver failure in women
Viral hepatitis E and autoimmune liver disease are more common in women than in men. [32] In a US multicenter study group, acute liver failure was seen more often in women (73%) than in men, and women with acute liver failure were older (39 y) than men (32.5 y).
Age and liver failure
Age may be pertinent to morbidity and mortality in those with acute liver failure. Patients younger than 10 years and older than 40 years tend to fare relatively poorly.
Prognosis
Before the introduction of orthotopic liver transplantation (OLT) for fulminant hepatic failure, mortality was generally greater than 80%. Approximately 6% of OLTs performed in the United States are for fulminant hepatic failure. However, with improved intensive care, the prognosis is much better now than in the past, with some series reporting a survival rate of approximately 60%.
The etiologic factor and the development of complications are the main determinants of outcome in acute liver failure. Patients with acute liver failure caused by acetaminophen have a better prognosis than those with an indeterminate form of the disorder. Patients with stage 3 or 4 encephalopathy have a poor prognosis. The risk of mortality increases with the development of any complications, which include cerebral edema, renal failure, adult respiratory distress syndrome (ARDS), coagulopathy, and infection.
Preoperative prognostic factors for liver transplantation survival in patients with acute liver failure appear to include the recipient's pretransplantation lowest pH and body mass index. [34] According to Hoyer et al, the recipient's lowest preoperative pH is also independently associated with inpatient mortality, in which the calculated cutoff is a pH of 7.26. [34]
Viral hepatitis
In patients with fulminant hepatic failure due to hepatitis A virus (HAV), survival rates are greater than 50-60%. These patients account for a substantial proportion (10-20%) of the pediatric liver transplants in some countries despite the relatively mild infection that is observed in many children infected with HAV. The outcome for patients with fulminant hepatic failure due to other causes of viral hepatitis is much less favorable.
Acetaminophen toxicity
Fulminant hepatic failure due to acetaminophen toxicity generally has a relatively favorable outcome, and the prognostic variables permit reasonable accuracy in determining the need for OLT. Patients in deep coma (hepatic encephalopathy grades 3-4) on admission have a higher mortality than patients with milder encephalopathy. An arterial pH of lower than 7.3 and either a prothrombin time (PT) greater than 100 seconds or serum creatinine level greater than 300 mcg/mL (3.4 mg/dL) are independent predictors of poor prognosis.
Non-acetaminophen-induced fulminant hepatic failure
In non-acetaminophen-induced fulminant hepatic failure, a PT of greater than 100 seconds and any three of the following five criteria are independent predictors [35] of a poor prognosis:
-
Age younger than 10 years or older than 40 years
-
Fulminant hepatic failure due to non-A, non-B, non-C hepatitis; halothane hepatitis; or idiosyncratic drug reactions
-
Jaundice present longer than 1 week before the onset of encephalopathy
-
PT longer than 50 seconds
-
Serum bilirubin level greater than 300 mmol/L (17.5 mg/dL)
In patients who meet three or more of these criteria, preparations for OLT should be arranged.
The above criteria were developed at King's College Hospital in London [35] and have been validated in other centers. However, significant variability occurs in terms of the patient populations encountered at any center, and this heterogeneity may preclude widespread applicability.
Many other prognosticating tests have been proposed. The combination of reduced levels of group-specific component (Gc)-globulin (a molecule that binds actin) is reported in fulminant hepatic failure, [36, 37] and a persistently increasing PT portends death. These and other parameters have not been widely validated yet.
Wilson disease
Wilson disease that presents as fulminant hepatic failure is almost uniformly fatal unless the patient undergoes OLT.
Onset of encephalopathy
Paradoxically, rapid progression from the onset of jaundice (usually the first unequivocal sign of liver disease recognized by the patient or family) to encephalopathy is associated with improved survival. When this interval is less than 2 weeks, patients have hyperacute liver failure. Although the grade of encephalopathy is a prognostic factor in cases of acetaminophen overdose, it does not correlate with outcome in other settings.
-
Ultrasonogram shows a hyperechoic mass representing hepatocellular carcinoma.
-
Subacute subdural hematoma with extension into the anterior interhemispheric cistern. Note that the sulci do not contain the spread of these hemorrhages.