Practice Essentials
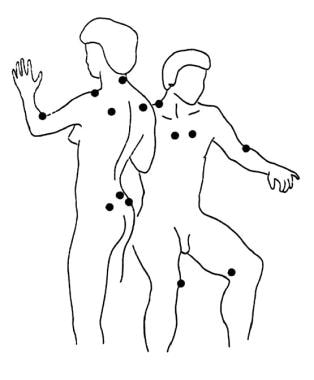
Fibromyalgia is a disorder of chronic, widespread pain and tenderness (see the image below). It typically presents in young or middle-aged women but can affect patients of either sex and at any age.
Signs and symptoms
Fibromyalgia is a syndrome that consists of the following signs and symptoms [1] :
-
Persistent (≥3 mo) widespread pain (pain/tenderness on both sides of the body, above and below the waist, including the axial spine [usually the paraspinus, scapular, and trapezius muscles])
-
Stiffness
-
Fatigue; disrupted and unrefreshing sleep
-
Cognitive difficulties
-
Multiple other unexplained symptoms, anxiety and/or depression, and functional impairment of activities of daily living (ADLs)
See Presentation for more detail.
Diagnosis
Fibromyalgia is a diagnosis of exclusion and patients must be thoroughly evaluated for the presence of other disorders that could be the cause of symptoms before a diagnosis of fibromyalgia is made. The clinical assessment may reveal objective evidence for a discrete or comorbid illness, such as the following:
-
Hypothyroidism
-
Rheumatoid arthritis
-
Systemic lupus erythematosus
-
Polymyalgia rheumatic
-
Other inflammatory or autoimmune disorders
-
Serious cardiac conditions in those with chest pain, dyspnea, and palpitations
Laboratory testing
Although patients with fibromyalgia do not have characteristic or consistent abnormalities on laboratory testing, routine laboratory and imaging studies can help to rule out diseases with similar manifestations and to assist in diagnosis of certain inflammatory diseases that frequently coexist with fibromyalgia. Such tests include the following:
-
Complete blood count with differential
-
Metabolic panel
-
Urinalysis
-
Thyroid-stimulating hormone level
-
25-hydroxy vitamin D level
-
Vitamin B12 level
-
Iron studies, including iron level, total iron binding capacity, percent saturation, and serum ferritin level
-
Magnesium level
-
Erythrocyte sedimentation rate
-
Antipolymer antibody assay: May provide conclusive evidence for a subgroup of people with fibromyalgia; about 50% of fibromyalgia patients have antipolymer antibodies
Patient self-report forms, clinical psychometric testing
Self-report forms, for assessing patients’ pain, fatigue, and overall status, include the following:
-
Modified Health Assessment Questionnaire
-
Fibromyalgia Impact Questionnaire
-
Checklist of current symptoms
-
Scales for helplessness and cognitive performance
-
The Physician Health Questionnaire–9 for depression
-
The Generalized Anxiety Disorder–7 questionnaire for anxiety
-
The Mood Disorder Questionnaire to screen for bipolar disease
Psychometric testing provides a more comprehensive assessment and includes the following:
-
Minnesota Multiphasic Personality Inventory
-
Social Support Questionnaire
-
Sickness Impact Profile
-
Multidimensional Pain Inventory
See Workup for more detail.
Management
There is no cure for fibromyalgia, but education, lifestyle changes, and proper medications can help the individual to regain control and achieve significant improvement.
Models of pain behavior that interrelate biologic, cognitive, emotional, and behavioral variables form the basis for cognitive-behavioral and operant-behavioral approaches to adult pain management. Fibromyalgia in children responds to a combination of psychotherapy, exercise, relaxation techniques, and education. Pharmacotherapy is generally not indicated in children.
Nonpharmacotherapy
-
Diet (eg, promote good nutrition, vitamin supplementation, bone health, weight loss)
-
Stress management
-
Aerobic exercise (eg, low-impact aerobics, walking, water aerobics, stationary bicycle)
-
Sleep therapy (eg, education/instruction on sleep hygiene)
-
Psychologic/behavioral therapy (eg, cognitive-behavioral, operant-behavioral)
Pharmacotherapy
Always combine pharmacologic and nonpharmacologic therapy in the treatment of fibromyalgia. Aggressively treat comorbid depression.
Medications used in the management of fibromyalgia include the following:
-
Analgesics (eg, tramadol)
-
Antianxiety/hypnotic agents (eg, alprazolam, clonazepam, zolpidem, zaleplon, trazodone, buspirone, temazepam, sodium oxybate)
-
Skeletal muscle relaxants (eg, cyclobenzaprine)
-
Antidepressants (eg, amitriptyline, duloxetine, milnacipran, venlafaxine, desvenlafaxine)
-
Anticonvulsants (eg, pregabalin, gabapentin, tiagabine)
-
Alpha 2 agonists (eg, clonidine)
Medications that may prove helpful for sleep problems that do not respond to nonpharmacotherapy include the following:
-
Antidepressants (eg, trazodone, SSRIs, SNRIs, tricyclic antidepressants)
-
Anticonvulsants (eg, clonazepam, gabapentin, tiagabine)
-
Nonbenzodiazepine hypnotics (eg, zolpidem, zaleplon, eszopiclone)
-
Muscle relaxants (eg, cyclobenzaprine, tizanidine)
-
Dopamine agonists (eg, pramipexole)
Other agents used in fibromyalgia may include the following:
-
Vitamins and minerals
-
Malic acid and magnesium combination
-
Antioxidants
-
Amino acids
-
Herbs and supplements
See Treatment and Medication for more detail.
Background
Fibromyalgia (FM) is a syndrome of persistent widespread pain, stiffness, fatigue, disrupted and unrefreshing sleep, and cognitive difficulties, often accompanied by multiple other unexplained symptoms, anxiety and/or depression, and functional impairment of activities of daily living (ADLs). [2, 1, 3] It typically presents in young or middle-aged women, but it can affect patients of either sex and at any age.
Fibromyalgia was once often dismissed by physicians and the public as a psychological disorder or "wastebasket" diagnosis because of an absence of objective findings on physical examination and usual laboratory and imaging evaluations. Some physicians still do not accept fibromyalgia as a discrete illness. However, basic and clinical investigations have clarified the neurophysiologic bases for fibromyalgia and led to its current classification as a central sensitivity syndrome (CSS). [4, 5]
Indeed, fibromyalgia can now be considered a neurosensory disorder characterized in part by abnormalities in pain processing by the central nervous system (CNS). [6] Increased understanding of the biological bases underlying fibromyalgia is rapidly leading to a new era of specific pharmacologic therapy for the condition.
At a clinical level, fibromyalgia is much more than widespread pain. It overlaps substantially with other central sensitivity syndromes, such as the following:
-
Chronic fatigue syndrome (systemic exertion intolerance disease [SEID])
-
Temporomandibular joint pain
-
Tension-type headaches/migraine
-
Multiple chemical sensitivity
Fibromyalgia also overlaps with other regional pain syndromes and mood and anxiety disorders. Indeed, the diagnostic label attached to a particular case may be determined largely by the first specialist that the patient sees. For example, a rheumatologist might diagnose fibromyalgia, whereas a gastroenterologist may diagnose irritable bowel syndrome or an infectious disease specialist may diagnose chronic fatigue syndrome.
In addition, fibromyalgia coexists in unusually high frequency with certain illnesses characterized by systemic inflammation, such as rheumatoid arthritis (RA), [7] systemic lupus erythematosus (SLE), [8] and chronic hepatitis C infection, [9] among others. In such cases, both disorders must be recognized and treated for optimum therapeutic outcome, as treatment of one will not necessarily improve the other.
Even as evidence-based medicine supplies a growing array of tools for the management of fibromyalgia, the art of medicine retains a central role. To successfully care for patients with fibromyalgia, the physician must demonstrate compassion as well as skill. Taking a careful history, listening to the patient's concerns, and performing a thorough examination are the foundation for diagnosing and treating fibromyalgia.
Management of fibromyalgia begins with a detailed history and a thorough physical and laboratory examination (see Presentation and Workup). Making a correct diagnosis is crucial, and patients need to know that a name exists for the mysterious symptoms that they are experiencing.
The physician should inform the patient that no cure exists for fibromyalgia but that education, lifestyle changes, and proper treatment can help the individual to regain control and achieve significant improvement. The overall approach for chronic pain in fibromyalgia involves a multifaceted treatment plan that incorporates various adjuvant medicines, aerobic exercise, and psychological and behavioral approaches to reduce distress and inflammation and promote self-efficacy and self-management. (See Treatment.)
Historical background
Although fibromyalgia was not defined until the late 20th century, it was discovered much earlier. Descriptions in the medical literature date as far back as the early 17th century and in the lay literature to ancient times with descriptions of the condition in the biblical book of Job.
Until recent decades, many physicians questioned the existence of fibromyalgia. Over time, however, a growing body of evidence established fibromyalgia as a syndrome comprising a specific set of signs and symptoms.
In 1987, the American Medical Association (AMA) acknowledged fibromyalgia as a true illness and a potential cause of disability. Many well-respected organizations, such as the AMA, the National Institutes of Health (NIH), and the World Health Organization (WHO), have accepted fibromyalgia as a legitimate clinical entity.
Before 1990, no accepted guidelines for identifying fibromyalgia patients for study existed. The American College of Rheumatology (ACR) sponsored a multicenter study to develop classification criteria; the results were published in 1990. [10] In 1992, at the Second World Congress on Myofascial Pain and Fibromyalgia, these classification criteria for fibromyalgia were expanded and refined. However, the criteria performed poorly in the clinic, failing to identify nearly half of fibromyalgia patients. [11] To improve diagnosis, new fibromyalgia diagnostic criteria were provisionally accepted by the ACR in 2010. [12]
Despite this progress, the typical patient with fibromyalgia has seen an average of 15 physicians and has had the condition for approximately 5 years before receiving a correct diagnosis. More than 50% of cases are misdiagnosed, and many patients undergo unnecessary surgery or endure costly treatments that provide little benefit.
At some point, most patients have been told that nothing is medically wrong with them and that their condition is imaginary. Therefore, many patients become frustrated and skeptical. Although most patients are relieved when a correct diagnosis is finally made, the patient may need to be convinced that the clinician actually knows what is wrong and has formulated a treatment plan.
Nomenclature
Although descriptions of the symptom complex now termed fibromyalgia have existed since earliest recorded history, the terminology used to refer to the condition has changed numerous times.
The first specific term, muscular rheumatism , was used in the early 19th century by surgeon William Balfour to describe a condition comprising disturbed sleep, fatigue, stiffness, and pain for which there was no explanation. [13] Balfour later described anatomic tender points accompanying the disorder that could be used in identification. In 1880, neurologist George Beard coined a new term, neurasthenia, characterized by a combination of symptoms including fatigue, widespread pain, and anhedonia. [14]
In 1904, Gowers renamed the disorder fibrositis after his incorrect belief that the disorder was caused by inflammation in muscle fascia. [15] Chaitrow asserts that no inflammatory process has ever been found to be part of this disease. [16] The syndrome was renamed fibromyalgia by Yunus et al in their seminal 1981 article derived from the Latin root fibro (fibrous tissue) and the Greek roots myo (muscles) and algos (pain). [17]
Pathophysiology
Fibromyalgia is currently understood to be a disorder of central pain processing or a syndrome of central sensitivity. Research has provided evidence for altered functional connectivity and chemistry in the pain-processing system of the brain. [18]
Clauw describes the syndrome as a diffuse problem of sensory “volume control” such that patients have a lower threshold of pain and of other stimuli, such as heat, noise, and strong odors. Clauw also suggests that patients may have hypersensitivity because of neurobiologic changes that affect the perception of pain or because of expectancy or hypervigilance, which may be related to psychological factors. [19]
Although the pathogenesis of fibromyalgia is not completely understood, research shows biochemical, metabolic, and immunoregulatory abnormalities. These substantiate the proposal that fibromyalgia can no longer be considered a subjective pain condition.
Pain
The International Association for the Study of Pain defines pain as "an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.” [20] Implicit here is the threat associated with pain, which can be trivial or profound.
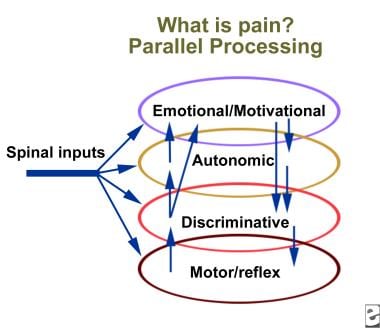
Neurophysiologically, the pain experience derives from a complex sensation-perception interaction involving the simultaneous parallel processing of nociceptive input from the spinal cord to multiple regions of the brain (see the image below).
In addition to strictly sensory-discriminative elements of nociception and afferent input from somatic reflexes, major contributions from pathways and regions of the brain that are associated with emotional, motivational, and cognitive aspects of pain are evident and help determine the subjective intensity of pain. The 2 principal effectors of the stress response, the hypothalamic-pituitary-adrenocortical (HPA) axis and the sympathetic nervous system (SNS), are also activated.
Although normally adaptive, the stress response may become maladaptive in patients with chronic pain and fatigue syndromes such as fibromyalgia. [21, 22, 23, 24] Negative emotions (eg, depression and anxiety) and other negative psychological factors (eg, loss of control, unpredictability in one's environment) and certain cognitive aspects (eg, negative beliefs and attributions, catastrophizing) can all function as stressors with actions in these systems.
Furthermore, negative emotions, such as anger and sadness, have been shown to be direct amplifiers of pain in women with and without fibromyalgia. [25] Thus, therapeutic approaches to regulate emotion may attenuate pain sensitization in patients with fibromyalgia.
In some patients with fibromyalgia, such negative emotional, motivational, and cognitive stressors may dominate the clinical picture, potentially leading to a self-sustaining neuroendocrine cascade that contributes to flulike symptoms, depressed mood, fatigue, myalgias, cognitive difficulties, and poor sleep.
The important biologic elements here include proinflammatory cytokines, the HPA axis, other neuroendocrine axes, and the autonomic nervous system. Growth hormone abnormalities are also thought to contribute to symptoms in fibromyalgia. [26]
Pain in patients with fibromyalgia derives partly from a generalized decrease in the pain perception threshold, with reduced discrimination of nociceptive sensations from non-nociceptive sensations (eg, touch, warmth, cold), and in the threshold for pain tolerance, resulting in an unwillingness to receive more-intense stimulation. [27]
These phenomena can be demonstrated clinically by pressure algometry (dolorimetry) or in research settings with quantitative sensory testing (QST) using pressure, heat, cold, or electricity as stimuli or with functional magnetic resonance imaging (fMRI) using pain stimuli. [6] Underlying these changes in thresholds is altered processing of nociceptive stimuli in the CNS (central sensitization).
A number of abnormalities in pain processing have been demonstrated in fibromyalgia. [28, 29, 30, 31, 32] Among them are the following:
-
Excess excitatory (pronociceptive) neurotransmitters (eg, substance P, glutamate levels in the insula)
-
Low levels of inhibitory neurotransmitters (eg, serotonin and norepinephrine) in descending antinociceptive pathways in the spinal cord
-
Maintained enhancement of temporal summation of second pain
-
Altered endogenous opioid analgesic activity in several brain regions known to play a role in pain modulation
-
Dopamine dysregulation
High-throughput genotyping is rapidly identifying a series of single-nucleotide polymorphism (SNP) haplotypes that influence neurotransmitter levels and receptor levels in the brain and thus contribute to the various abnormalities in pain processing. [33, 34] Such SNP haplotypes constitute vulnerability elements in the development of fibromyalgia and other central sensitivity syndromes.
Pharmacologic agents that reduce pain in fibromyalgia function in this regard by either increasing levels of inhibitory neurotransmitters (eg, duloxetine) or decreasing levels of excitatory neurotransmitters (eg, pregabalin). [28, 35] Because fibromyalgia is a polygenic syndrome with multiple different underlying genetic polymorphisms, genetic testing to tailor therapy and to predict response to therapy will soon become available.
The biochemical changes seen in the CNS, the low levels of serotonin, the four-fold increase in nerve growth factor, and the elevated levels of substance P all lead to a whole-body hypersensitivity to pain and suggest that fibromyalgia may be a condition of central sensitization or of abnormal central processing of nociceptive pain input. [5] Ongoing research will continue to provide a clearer picture of the pathophysiology of this complex syndrome.
Pain sensitivity in women
Fibromyalgia is most common in women. Among the mechanisms that may contribute to increased pain sensitivity in women are the following [36] :
-
Differences in primary afferent input to the CNS, with developmental and menstrual cycle–dependent enhancement
-
Developmental and phasic gonadal-hormonal modulation of pain regulatory systems, stress-induced analgesia, and opioid receptors
-
Higher levels of trait and state anxiety
-
Increased prevalence of depression
-
Use of maladaptive coping strategies
-
Increased behavioral activity in response to pain
Central processes
Plasticity in the function of N-methyl-D-aspartate (NMDA) subtype glutamate receptors is necessary for central sensitization to occur. Increased sensitivity of central NMDA receptors was implicated in earlier studies as playing a primary role in fibromyalgia. However, subsequent evidence has suggested that suppression of the normal activity of dopamine-releasing neurons in the limbic system is the primary pathology in fibromyalgia. Increasing evidence indicates that fibromyalgia may represent a dysregulation of dopaminergic neurotransmission.
Serotonin
The most widely acknowledged biochemical abnormality associated with fibromyalgia is abnormally low serotonin levels. Many studies have linked serotonin, a neurotransmitter, to sleep, pain perception, headaches, and mood disorders. Lower-than-normal levels of serotonin have been observed in patients with fibromyalgia. A low platelet serotonin value is believed to be the cause of the low serum levels, which have been correlated with painful symptoms.
Low serotonin levels in the CNS are thought to result from low levels of tryptophan (the amino acid precursor to serotonin) and 5-hydroxyindole acetic acid (a metabolic by-product) in the cerebrospinal fluid (CSF). Investigators have proposed a link between low serotonin levels and symptoms of fibromyalgia [37] ; indeed, many propose that low serotonin levels may cause fibromyalgia in whole or in part.
Substance P
Substance P is a neurotransmitter that is released when axons are stimulated. Elevated levels of substance P increase the sensitivity of nerves to pain or heighten awareness of pain. Four independent studies have found that levels of substance P are 2 to 3 times higher than normal in the CSF of patients with fibromyalgia. [38] These elevated levels cause fairly normal stimuli to result in exaggerated nociception.
Some authors believe that neither elevated substance P levels nor low serotonin levels alone can be the primary cause. Instead, the dual dysfunction may be responsible for fibromyalgia.
Adenosine triphosphate
Researchers have found low levels of adenosine triphosphate (ATP) in red blood cells of patients with fibromyalgia. Although the significance is unknown, it has been suggested that low platelet serotonin levels can be explained if platelet ATP levels are also low. ATP is necessary to move and then hold serotonin in platelets. More investigation into ATP and the link to serotonin is needed.
Dysfunction of the hypothalamic-pituitary-adrenal axis
Studies of the neuroendocrine aspects of fibromyalgia have found dysfunction of the HPA axis. [39] The HPA axis is a critical component of the stress-adaptation response. The sequence of HPA action is that corticotropin-releasing hormone (CRH) from the hypothalamus stimulates the anterior pituitary to release adrenocorticotropic hormone (ACTH). In turn, ACTH stimulates the adrenal cortex to produce glucocorticoids (eg, cortisol).
Some authors have noted that 5 main measurable neuroendocrine abnormalities are associated with dysfunction of the HPA axis. [40] These are as follows:
-
Low free cortisol levels in 24-hour urine samples
-
Loss of the normal circadian rhythm, with an elevated evening cortisol level (when it should be at its lowest level)
-
Insulin-induced hypoglycemia associated with an overproduction of ACTH
-
Low levels of growth hormone
-
Stimulated ACTH secretion leading to insufficient adrenal release of glucocorticoids
Circadian regulation and the stress-induced stimulation of the HPA axis are, in part, regulated by serotonin. Perturbations in serotonin metabolism (as well as premorbid abnormalities of the HPA axis) may explain the abnormalities of the HPA axis in fibromyalgia. Dysfunction of the HPA axis may exaggerate the effects of abnormal serotonin metabolism. Hypoactivity of the HPA axis may cause low central serotonin levels.
Growth hormone
Growth hormone, produced during delta sleep, is involved in tissue repair. Therefore, disrupted stage 4 (delta) sleep associated with fibromyalgia may account for low levels of growth hormone. Growth hormone stimulates the production of insulinlike growth factor I (IGF-I) in the liver. Some authors have found that most patients with fibromyalgia have low levels of IGF-I and that low levels are specific and sensitive for fibromyalgia. [41]
Nerve growth factor
In some studies, nerve growth factor was found to be 4 times higher in the CSF of patients with fibromyalgia than it was in the CSF of individuals without the condition. Nerve growth factor enhances the production of substance P in afferent neurons, increasing an individual's sensitivity to or awareness of pain. Nerve growth factor also may play a role in spreading or redistributing perceived pain signals.
Glial activation
A functional brain imaging study has demonstrated activation of glial cells in patients with fibromalgia; these cells release inflammatory mediators that are thought to sensitize pain pathways and contribute to symptoms such as fatigue. Albrecht et al demonstrated brain inflammation in fibromyalgia by using hybrid magnetic resonance/positron emission tomography (MR/PET) and the radioligand (11C)PBR28, which binds to the translocator protein (TSPO). Expression of TSPO is low in healthy CNS tissue, but TSPO is widely upregulated in microglia and astrocytes under inflammatory conditions. [42]
In the study, which included 31 patients with fibromyalgia and 27 healthy controls, the patients had higher levels of TSPO, most pronounced in the medial and lateral walls of the frontal and parietal lobes. The degree of glial activation correlated with the degree of fatigue the patients reported. [42]
Cognitive impairment
Fibromyalgia is associated with a decline in short-term, working, episodic, semantic (predominantly verbal), and procedural (skills) memory. Imaging modalities such as single-photon emission computed tomography (SPECT) scanning have helped to define some of the abnormalities linked to this cognitive dysfunction. SPECT shows decreased blood flow in the right and left caudate nuclei and thalami.
Functional magnetic resonance imaging (fMRI) can show brain activity by depicting increased blood flow to areas actively engaged in a task. Increased blood flow and, hence, increased oxygenation have different magnetic properties. These properties can be detected and measured using fMRI.
In a study of persons performing a task requiring memory (alphabetization), persons with fibromyalgia performed almost as well as controls, but fMRI showed that more brain areas were activated during the memory task in persons with fibromyalgia than in controls, because the task was harder for the patients to perform. In another study, working memory and episodic memory scores of patients with fibromyalgia were similar to those of healthy controls who were 20 years older. [43]
Another study measured neural activation during response inhibition using fMRI. Patients with fibromyalgia had lower activation in the inhibition and attention networks but increased activation in other areas. The study indicates that inhibition and pain perception may use overlapping networks, which may cause resources to be unavailable for other processes when they are taken up by pain processing. [44]
Cognitive dysfunction has been linked to CNS imbalances. Abnormal levels of such neurotransmitters as substance P, serotonin, dopamine, norepinephrine, and epinephrine may cause cognitive dysfunction. Neuroendocrine imbalance of the HPA axis may play a role. Another possible cause of cognitive dysfunction is the distracting quality of pain in fibromyalgia. Cognitive performance of patients with fibromyalgia correlates with their reported level of pain.
Brain damage from the effects of stress hormones may be involved in the cognitive dysfunction in fibromyalgia. Researchers are exploring this possibility by measuring tissue volumes in the hippocampus. Other studies have implicated yeast overload, water retention, and glial cell abnormalities as causes of cognitive dysfunction in fibromyalgia.
Sleep disruption
Sleep dysfunction is considered an integral feature of fibromyalgia. About 70% of patients recognize a connection between poor sleep and increased pain, along with feeling unrefreshed, fatigued, and emotionally distressed. [45, 46] Several studies have linked abnormal sleep with these symptoms. Sleep studies have shown that patients with fibromyalgia have disordered sleep physiology.
Sleep is not a state of massive system shutdown. On the contrary, the brain is active during sleep, constantly communicating with the body. Many neurohormones, antibodies, and other molecules are synthesized during sleep; therefore, when sleep is disrupted, biochemical abnormalities can occur, leading to multisystem disturbances.
To understand abnormal sleep architecture, it is essential to know the basics of normal sleep. Sleep can be divided into 2 main parts: nonrapid eye movement (NREM) and rapid eye movement (REM), which alternate cyclically through the night, always starting with NREM sleep. In each successive cycle through the night, NREM sleep decreases, and REM sleep increases. Each cycle, NREM plus REM, lasts about 90 minutes.
NREM is divided into 4 stages:
-
Stage 1 – Initial drowsiness
-
Stage 2 – Light sleep
-
Stages 3 and 4 – Progressively deeper levels of sleep.
In stages 3 and 4, an electroencephalogram (EEG) will show delta waves, which are high-amplitude (>75 mV) waves that move slowly (0.5-2 Hz). Much of the body's regulatory work, as well as the synthesis of many substances (eg, antibodies, growth hormone, other neurochemicals), occurs during NREM sleep.
REM sleep has a low-voltage, mixed-frequency pattern on EEGs and is considered dream sleep. In this stage, the body has a complete loss of muscle tone, known as flaccid paralysis, and it cannot move. During this part of sleep, consolidation of memories may occur, but disagreement still exists as to what takes place with regard to memory during REM sleep.
During waking hours, the brain generates alpha waves with a frequency of 7.5-11 Hz. The disordered sleep physiology in fibromyalgia has been identified as a sleep anomaly of alpha-wave intrusion, which occurs during NREM stage 4 sleep. This intrusion into deep sleep causes the patient to awaken or to be aroused to a lighter level of sleep. Some investigators describe the altered sleep physiology and somatic symptoms as a nonrestorative sleep syndrome.
Sleep dysfunction is believed to be linked to the numerous metabolic disturbances associated with fibromyalgia, including abnormal levels of neurotransmitters (serotonin, substance P) and neuroendocrine and immune substances (growth hormone, cortisol, interleukin-1). These metabolic imbalances are thought to be responsible—through impairment of tissue repair and disturbance of the immunoregulatory role of sleep—for the increased symptoms associated with this sleep disorder of alpha-wave intrusion.
Most alpha-wave intrusions occur during the first few hours of sleep, decreasing throughout the night to normal levels by early morning. This hypothesis correlates well with patients' frequent reporting that their best sleep is obtained in the early morning hours, just before arising.
Many fibromyalgia patients also have primary sleep disorders that can reduce sleep quality, such as obstructive sleep apnea, restless legs syndrome, or periodic limb movement disorder. All patients should be screened for the presence of primary sleep disorders before assuming that reduced sleep quality is due to fibromyalgia.
Neuroimmune dysfunction
Goebel et al reported that immunoglobulin G (IgG) obtained from patients with fibromyalgia and injected intraperitoneally into mice caused sensitization of nociceptive neurons, resulting in sensory hypersensitivity by sensitizing nociceptive neurons. The mice displayed greater sensitivity to mechanical and cold stimulation, reduced locomotor activity, reduced paw grip strength, reduced intraepidermal nerve fibers, and sensitization of nociceptive small fibers. [47]
Injection of IgG from healthy controls, or of IgG-depleted serum from fibromyalgia patients, did not produce any of those effects. In mice receiving IgG injections from fibromyalgia patients, the effects diminished after discontinuation of the injections. [47]
Histologic analysis showed that the IgG from fibromyalgia patients had bound to satellite glial cells, which envelope sensory neurons in the dorsal root ganglia. Activation of satellite glial cells is known to mediate chronic pain by augmenting neuronal activity. [47, 48]
Etiology
The etiology of fibromyalgia is multifactorial and includes both environmental and genetic factors. While the causes of fibromyalgia have not yet been fully clarified, remarkable progress in the understanding of this disorder has been made. For example, with the identification of central sensitization and abnormal central nociceptive processing in affected patients, fibromyalgia pain can now be classified as a neurosensory disorder. Increasing evidence points to "complex, dynamic, and mutual crosstalk between neurophysiological and psychosocial domains." [49]
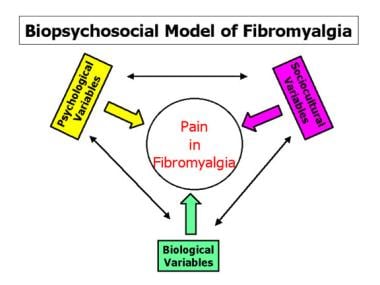
Engel's biopsychosocial model of chronic illness (ie, health status and outcomes in chronic illness are influenced by the interaction of biologic, psychological, and sociologic factors) provides a useful way to conceptualize fibromyalgia. [50] The model is pictured in the image below.
Biologic variables
Certain biologic variables contribute to the development and persistence of fibromyalgia, although none, as a single element, explains all facets of fibromyalgia. Certain variables (eg, physical trauma, exposure to toxins) have been widely incriminated by the public, particularly in medicolegal settings, but are actually of little significance in the etiology of fibromyalgia, as shown by prospective studies.
Inheritance
The extremely important genetic contribution to fibromyalgia and related central sensitivity syndromes was first suggested by family studies. [51, 52] Subsequently, the application of sophisticated genotyping and statistical methodology has provided a detailed view of this relationship. [53, 54] Susceptibility to and severity of fibromyalgia appears to be influenced by polymorphisms in genes involved in the catecholaminergic pathway, the serotonergic pathway, pain processing, oxidative stress, and inflammation. Epigenetic changes may promote the development of fibromyalgia, and microRNAs may affect the expression of certain proteins associated with symptoms of fibromyalgia. [55]
For example, altered serotonin metabolism in a subgroup of patients with fibromyalgia has been linked to a genotype of the promoter region of the serotonin transporter gene. [56] Single-nucleotide polymorphisms in the genes for catecholamine-O-methyltransferase (which inactivates catecholamines) and β2-adrenergic receptors have been linked to increased pain perception. [33, 37, 57]
Female sex
Sex-related effects are important in fibromyalgia and with pain in general. [58] Central pain modulatory systems in females are influenced by phasic alterations in reproductive hormone levels. Aversive stimuli and stressful tasks are more likely to evoke SNS, HPA axis, and psychological responses in females than in males.
Sleep
Almost all patients with fibromyalgia sleep poorly—hence, the common report that a night of poor sleep is followed by a more painful day. Indeed, intrusion of alpha waves into slow delta wave stage III/IV (deep) sleep was the first objective abnormality observed in fibromyalgia. [59] Although not the proximate cause of fibromyalgia, abnormal sleep affects both limbs of the stress response system and contributes to negative mood and cognitive difficulties.
Trauma and tissue injury
Trauma as a trigger of fibromyalgia has been a highly contentious and medicolegally charged issue in American society. Until very recently, physical trauma as a causative factor in the development of fibromyalgia was an open question because properly designed prospective studies had not been performed and little experimental evidence explained the presence of pain in the absence of tissue injury.
Setting aside case series and other anecdotal observations that do not provide valid evidence concerning causation, numerous controlled investigations on this issue are now available. The preponderance of current evidence does not support physical trauma as a significant causative factor in the development of fibromyalgia. [60, 61, 62, 63, 64] At a clinical level, however, patients who attribute their fibromyalgia to trauma have more perceived disability, self-reported pain, life interference, and affective distress than patients with idiopathic onset.
Stress/neuroendocrine and autonomic dysregulation
A large body of data suggests that fibromyalgia, chronic fatigue syndrome, regional chronic pain syndromes, and certain emotional disorders that frequently coexist with fibromyalgia all involve central dysregulation of the stress response system. [22, 24, 53, 65, 66] In these disorders, various forms of stress function as initiators or perpetuators of functional alterations in the corticotropin-releasing hormone (CRH) neuron, with associated effects on the HPA axis, other neuroendocrine axes, and the SNS.
Subtle abnormalities in the stress response system, which cannot be detected by routine clinical and laboratory assessments, may contribute to the diverse clinical manifestations in this spectrum of illnesses. Although incomplete, the emerging evidence is beginning to clarify how the brain, endocrine, and immune systems (especially proinflammatory cytokines) interact in the pathophysiology of pain, fatigue, neurally mediated hypotension, depression, anxiety, and poor sleep.
The extremely high prevalence of stress-related disorders in society may reflect maladaptation of the stress response system in the face of the almost universal stress and consequent distress that characterizes modern life.
Other variables
Age is an important variable. While most patients begin to experience symptoms between the ages of 20 and 50 years, the prevalence of the syndrome increases with age. The highest prevalence occurs between ages 60 and 79 years. [67]
Physical deconditioning is also an important variable. Moldofsky et al showed that disrupting stage 4 sleep in sedentary healthy controls elicited the appearance of musculoskeletal and mood symptoms similar to those seen in fibromyalgia patients. [59] However, when similar sleep disruption was performed in healthy controls who were regular exercisers, fibromyalgia symptoms did not develop. [68] This implies that regular physical activity may be protective and underscores the importance of maintaining physical activity in fibromyalgia patients.
While considered unlikely to be sole triggers, infection may also contribute to exacerbation of symptoms via cytokine–vagus nerve stimulation of the corticotropin-releasing hormone neuron/stress response system in bidirectional brain–immune system communication. [9]
Variables with an uncertain relationship to the development of fibromyalgia include the following:
-
Decreased collagen cross-linking
-
Hypermobility
-
Chiari malformation
-
Environmental chemicals
Psychological variables
Although not significant in all patients with fibromyalgia, cognitive-behavioral variables can be pivotal in the development and maintenance of persistent pain and functional disability. [36] The repertoire of operant cognitive-behavioral variables in adults have antecedents in earlier life (eg, childhood abuse, parental alcoholism, learned behaviors from living as children with dysfunctional or chronically ill parents).
By early adulthood, a failure in goal-oriented behavior may develop, leading to lower self-efficacy, the inability to achieve goals, and a fear of failure. In turn, this may presage reporting of chronic pain as a socially acceptable excuse for failure to achieve goals in later life.
Meaning structures
Qualitative research shows that some patients with fibromyalgia exhibit meaning structures that facilitate their "invisible," "capricious" illness for which they cannot be blamed. Unwittingly, this may serve as an excuse for not meeting the demands and challenges of life, with accompanying strong rejection of any notion that fibromyalgia could have psychological antecedents. When this occurs, physicians and/or counselors should assist the patient in avoiding the choice of illness as a way to deal with difficult personal-life situations.
Pain beliefs and attributions
Negative beliefs (eg, self-blame for the mysterious enduring pain) are associated with a range of adverse consequences, as follows:
-
Increased subjective pain intensity
-
Reduced compliance with treatment
-
Low self-esteem
-
Somatization
-
Psychological distress
In patients with chronic pain, the expected degree of tolerance to stimuli or activities that evoke pain or fatigue predicts actual tolerance. Expected danger (damage) predicts avoidance.
Self-assessed inability to work, helplessness, low perceived control over pain, and maladaptive coping all affect pain severity and the overall impact of fibromyalgia. Thus, some patients with fibromyalgia perceive that they are using excessive effort during formal exercise testing of muscle, even though their actual muscle function is electrophysiologically normal.
Similarly, the discordance between self-reported disability versus observed functional disability can be high in some patients with fibromyalgia. In contrast, such discordance is generally low or absent in patients with other rheumatic diseases, such as ankylosing spondylitis and rheumatoid arthritis.
Hypervigilance
Certain data support a hypervigilance model of pain in patients with fibromyalgia. [69] Heightened sensitivity to pain leads at least in part to increased attention to external stimuli and a preoccupation with pain sensations. Thus, pain is amplified by hypervigilance to pain. Patients with fibromyalgia may become what they perceive themselves to be.
Self-efficacy and coping
Perceived self-efficacy is the level of confidence that the patient requires to control pain effectively. People with high self-efficacy beliefs engage in coping behaviors until success is achieved. People with low self-efficacy beliefs anticipate failure and stop using effective coping strategies. Higher coping self-efficacy is associated with less negative mood and less pain.
Treatments that improve coping reduce pain and enhance a positive mood. However, excessive use of active coping may actually be detrimental in patients with fibromyalgia who have low self-efficacy for pain control.
Self-efficacy may be a significant determinant of pain itself, particularly with respect to its emotional arousal and unpleasant effects. In a study of patients with osteoarthritis, those scoring high for self-efficacy about arthritis pain control exhibited higher thresholds and tolerance for thermal pain compared with those who had low scores. [70] Conversely, maladaptive coping strategies, such as catastrophizing about pain, worsen the pain experience, especially with respect to the development of depression.
Pain catastrophizing, defined as characterizing pain as unbearable or horrible, is an important factor in the experience of pain. Research using functional magnetic resonance imaging (fMRI) to measure regional cerebral blood flow (rCBF) and quantitative sensory testing (QST) techniques has demonstrated that in persons with high catastrophizing, pain perception is augmented by increased activity in response to painful stimuli in brain areas involved in the following [71] :
-
Anticipation of pain (medial frontal cortex, cerebellum)
-
Attention to pain (dorsal anterior cingulate gyrus, dorsolateral prefrontal cortex)
-
Emotional aspects of pain (claustrum, closely connected to the amygdala)
Depression and anxiety
Lifetime psychiatric comorbidity is common in individuals with fibromyalgia, including the following [72, 73] :
-
Mood disorders (bipolar disorder, major depressive disorder)
-
Anxiety disorders (generalized anxiety disorder, obsessive-compulsive disorder, panic disorder, PTSD, social phobia)
-
Eating disorders
-
Substance use disorders
Pressure-pain thresholds (degree of tenderness with application of pressure) correlate with psychological comorbidity in patients with fibromyalgia, as follows [74] :
-
Low tenderness is associated with moderate depression/anxiety, moderate catastrophizing, and moderate control over pain
-
High tenderness is associated with high depression/anxiety, high catastrophizing, and low control over pain
-
Extremely high tenderness is associated with normal levels of depression/anxiety, very low catastrophizing, and highest control over pain
Depression contributes to the subjective unpleasantness and distress of pain through parallel, somewhat independent neural pain processing networks for purely sensory and affective pain elements. People who are healthy and people who have fibromyalgia but no depression exhibit increased rCBF only in the somatosensory cortices and the anterior insula, whereas people with fibromyalgia and depression also show increased rCBF in the amygdala and contralateral anterior insula, which are involved in affective pain processing. [75]
However, chronic pain is not simply a manifestation of depression. Despite common reports of pain and other somatic symptoms, patients with pure major depression, compared with patients with fibromyalgia, actually have fewer tender points, higher pain thresholds, and more stoic responses to pain stimuli. [76] In addition, negative emotions such as sadness and anger have been shown to be general risk factors for pain amplification independent of a diagnosis of fibromyalgia. [25]
Personality traits and disorders
Personality traits have the largest effect on the cognitive processes by which people attach meanings and implications to their pain. [36] For example, neuroticism, which is associated with hypochondriasis, irritability, and emotional disturbance, has no influence on the discrimination of thermal pain but exerts powerful influences in the delayed reflective stage of pain (ie, at the level of emotions related to suffering, including depression, anxiety, and, especially, frustration).
Several personality styles among patients with fibromyalgia are encountered in clinical practice. [77, 78] Most common is a perfectionism-compulsiveness personality, characterized by a rigid belief system in the need to be perfect, high underlying anxiety, and an unawareness of feelings and emotions. Another common personality style is the self-sacrificing type, characterized by a tendency to put everyone else’s needs before one’s own.
Less common is the "wounded warrior" type. These patients, who may be totally helpless and disabled physically and psychologically, carry a great burden of adverse psychosocial experiences and psychiatric comorbidity.
These 3 personality styles are difficult to treat and often require counseling or psychiatric intervention. The "resilient" patient who lacks maladaptive schemas and psychiatric comorbidity has a much better prognosis.
Pain behaviors
At one level, pain behaviors are the various signals that serve to communicate the pain experience to the outside world and include nonverbal expressions of pain (eg, grimacing, bracing, sighing, rubbing, groans, histrionic behavior). Increased pain behaviors are associated with more depression, reduced self-efficacy for pain control, and more negative thoughts.
Pain behaviors can be important perpetuators of illness through reinforcement of the responses that patients with fibromyalgia induce as a means to get attention, to obtain medication, or to avoid work or activity. This can lead to limitation of physical and social activity, dependence on narcotics and alcohol, and unemployment.
A common pain behavior in patients with fibromyalgia is an excessive use of medical services. Care seekers exhibit lower pain thresholds and greater psychiatric morbidity than patients without fibromyalgia who do not have chronic pain, an observation consistent with the idea that care seeking reduces the emotional distress consequent to symptoms and life stressors.
Environmental and sociocultural variables
Multiple experiences and forces in a person's environment and social culture influence the pain experience, either positively (eg, high job satisfaction in a person who strains his or her back at work) or negatively (eg, a physician who medicalizes a minor injury by diagnostic waffling and inappropriate diagnostic testing). [36] Environmental and sociocultural variables include the following:
-
Psychosocial experiences during childhood
-
Spousal and family support
-
Ethnologic factors
-
Focus on definable causes
-
Media hype
-
Primary and secondary gain
Developmental variables
Developmental variables include the psychosocial experiences during childhood (eg, school stress, role models, unhappy families, abuse) that shape the cognitive, affective, and behavioral aspects of pain in adults. Some studies show that two thirds of patients with chronic pain have first-degree relatives with chronic pain, one third have a family member with an affective illness, and one third have a family member with alcohol abuse.
Childhood physical, emotional, or sexual abuse appears to be a common antecedent of anxiety, somatization, and chronic pain in many adults. For example, in a community population–based screening survey, the association of childhood abuse with the presence of more than 5 tender points (a characteristic of fibromyalgia) in adults was very strong (odds ratio, 6.9). [79] Biologic vulnerability likely derives, in part, from persisting effects of early life stresses on the stress response system.
Family and work variables
Spousal and family support can either mitigate or exacerbate the various dimensions of chronic pain. Training of spouses to enhance their ill partner's coping skills improves self-efficacy for pain control and reduces pain and psychological distress. Spousal reinforcement of pain behaviors can lower experimentally determined pain thresholds.
Job satisfaction and a healthy work environment lessen the emotional distress associated with chronic pain. Conversely, job dissatisfaction strongly predicts the progression of acute back pain to chronic low back pain. Similarly, workers' compensation and disability benefits can be significant disincentives for recovery from chronic pain.
Sociocultural factors
Pain tolerance may be profoundly influenced by culture. The prevalence of widespread chronic pain is zero in Pima Indians but is approximately 10% in white populations on both sides of the Atlantic. The current epidemic of fibromyalgia, chronic fatigue syndrome, sick building syndrome, and multiple chemical sensitivity syndrome is arguably due, at least in part, to media hype, fear, suggestibility, and a focus on definable causes by patients and physicians.
Epidemiology
Cases of fibromyalgia have been reported by researchers from around the world. Fibromyalgia exhibits no race predilection. Researchers have reported the condition in all ethnic groups and cultures.
In the United States, chronic pain and fatigue are extremely prevalent in the general population, [67, 80, 81] especially among women and persons of lower socioeconomic status. The prevalence of regional pain is 20%; widespread pain, 11%; and chronic fatigue, approximately 20%.
Fibromyalgia, as defined by the 1990 American College of Rheumatology (ACR) classification criteria, [10] has a prevalence of 3-5% in females and 0.5-1.6% in males. Because the ACR criteria are insensitive, the actual prevalence of fibromyalgia is higher, particularly in men.
Fibromyalgia is the second most common disorder that rheumatologists encounter, seen in 15% of evaluated patients. Approximately 8% of patients cared for in primary care clinics have fibromyalgia.
The annual economic burden of fibromyalgia in 2005 was $10,199 per patient per year, nearly double that of matched controls. [82] It has been estimated that overall, fibromyalgia costs the US economy over $9 billion annually. [83]
United States prevalence
Wolfe et al estimated that the prevalence of fibromyalgia in the US general population was 2% (3.5% in women and 0.5% in men). [67] However, this estimation was reached using the original 1990 American College of Rheumatology (ACR) classification criteria, [10] and those classification criteria miss nearly half the patients clinically diagnosed with fibromyalgia, [11] Thus, this estimate is probably low. It is especially likely to have underestimated the prevalence in men, who have fewer positive tender points and so are less likely to meet the classification criteria.
A study by Vincent et al using the 2010 ACR diagnostic criteria estimated the prevalence of fibromyalgia at 6.4% (7.7% in women and 4.9% in men). [84] It is likely that this higher prevalence rate is a more accurate estimate.
International prevalence
Using data from 5 countries (France, Germany, Italy, Portugal, and Spain), Branco et al estimated the prevalence of fibromyalgia in Europe at 4.7%. [85] Prevalence was estimated to be 5.8% in women and 3.5% in men. However, this estimate used the London Fibromyalgia Epidemiological Study Screening Questionnaire (LFESSQ), a nonstandard method of identifying fibromyalgia patients. Another study using the LFESSQ estimated the prevalence of fibromyalgia in Tunisia at least at 8.3%. [86]
White et al estimated the prevalence of fibromyalgia at 3.3% in Ontario, Canada (4.9% women vs 1.6% men). [87] However, this estimate was derived using the 1990 ACR classification criteria, [10] so it is likely this estimate is low, particularly in the male population.
The prevalence of fibromyalgia in the general population of Brazil has been estimated at 4.5%. [88] A similar Brazilian study in the elderly population estimated the prevalence at 5.5%. [89] Interestingly, all fibromyalgia patients identified in both Brazilian studies were female, despite a large percentage of male participants. Since both studies used the 1990 ACR classification criteria, it is likely the number of both male and female patients were underestimated.
Race-related differences in incidence
While studies have identified patients with fibromyalgia in countries around the world, most have been done in developed countries and few have looked specifically at the effect of race.
In the United States, African-American women have a higher prevalence of fibromyalgia than white women. [90] However, increased body pain and tenderness are associated with decreased socioeconomic status, so this may be an important influence on racial differences. Another study comparing Sephardic and Ashkenazic Israeli women found that education, rather than ethnic identity, was a determining factor in clinical features of fibromyalgia. [91] Studies of persons in China appear to demonstrate a consistently lower prevalence of fibromyalgia than persons in the United States and Europe. [92]
Much work needs to be done to better understand racial differences, but it has been limited by the need to perform tender-point examinations to identify patients. The demonstration that a patient self-report questionnaire using the modified 2010 ACR criteria fibromyalgia can reliably identify fibromyalgia patients should allow for more studies on race and fibromyalgia to be conducted. [93]
Sex-related differences in incidence
In pediatric cases, differences in fibromyalgia prevalence between boys and girls are hardly evident. In adults, women tend to develop fibromyalgia more often than men. However, the true difference in prevalence between women and men depends on how the disorder is defined. If fibromyalgia is defined as fulfillment of the original 1990 ACR classification criteria that require pain on palpation of at least 11 of 18 tender points, [10] fibromyalgia prevalence displays a 7:1 female:male ratio. [67]
However, the 1990 ACR classification criteria miss nearly half of patients clinically diagnosed with fibromyalgia and perform particularly poorly in men since they tend to have fewer painful tender points. [11] If instead fibromyalgia is defined using the 2010 ACR diagnostic criteria that do not use tender points, the difference in prevalence of fibromyalgia between women and men is only about 2:1. [84]
Males with fibromyalgia tend to have lower health perception and more physical limitations than females. Females with fibromyalgia have greater pain sensitivity [58] and may exhibit greater life interference due to pain.
Among the mechanisms that may contribute to increased pain sensitivity in women are the following [36] :
-
Differences in primary afferent input to the CNS, with developmental and menstrual cycle–dependent enhancement
-
Developmental and phasic gonadal-hormonal modulation of pain regulatory systems, stress-induced analgesia, and opioid receptors
-
Higher levels of trait and state anxiety
-
Increased prevalence of depression
-
Use of maladaptive coping strategies
-
Increased behavioral activity in response to pain
Age-related differences in incidence
Although usually considered a disorder of women aged 20-50 years, fibromyalgia can occur at any age and in persons of either sex. Fibromyalgia occurs in pediatric populations, especially during adolescence. [94] The prevalence of fibromyalgia increases with age, and the peak prevalence is not seen in women until age 60-70 years. [67] All patients with widespread pain, regardless of age, should be evaluated for fibromyalgia.
Prognosis
Fibromyalgia is a chronic relapsing condition. In academic medical centers, long-term follow-up care of patients with fibromyalgia reportedly averages 10 outpatient visits per year and 1 hospitalization every 3 years. Chronic pain and fatigue in fibromyalgia increases the risk for metabolic syndrome.
Entirely reversing the allodynia and hyperalgesia in patients with fibromyalgia may be impossible. Nevertheless, symptoms can be significantly improved in many patients, particularly if ongoing stressors are relieved and self-efficacy for pain control can be achieved.
The treatment goal that responds least to therapy is improvement in daily functioning. A positive therapeutic response usually requires resolution of pending litigation (personal injury or workers’ compensation claims). While most patients assume that stopping work will improve their symptoms, numerous studies have shown that symptoms worsen when fibromyalgia patients go on disability. [95]
The following three distinct subsets of patients with varying prognoses have been identified [96, 97] :
-
Adaptive copers, who often do not seek care for their symptoms, do well with respect to pain, sleep, and fatigue.
-
Interpersonally distressed patients may respond to resolution of life stressors and interdisciplinary therapeutic approaches, including counseling.
-
Dysfunctional patients have high levels of pain and anxiety, major impairment in daily functioning, and, quite often, opioid dependence. These patients have a very poor prognosis.
Other patient characteristics associated with guarded prognosis include the following:
-
High levels of distress
-
Long-standing fibromyalgia
-
Major psychiatric disease or severe depression and anxiety that responds poorly to treatment
-
An ingrained pattern of work avoidance
-
Marked functional impairment despite multidisciplinary approaches to treatment
-
Opioid or alcohol dependence
Fibromyalgia is not a life-threatening, deforming, or progressive disease. Without proper diagnosis and treatment, however, a patient with fibromyalgia may have the illusion of disease progression. This illusion does not occur as a result of disease but is instead caused by sleep deprivation and physical deconditioning.
Approximately one third of patients with fibromyalgia reportedly modify their work to keep their job. Some patients shorten their workday and/or workweek, and many persons with fibromyalgia change to a job that is less physically and mentally taxing than their previous one. Patients have also reported an inability to achieve career or educational advancement, and some have reported career loss. Such changes often lead to a decreased income and increased financial burdens.
One study of patient perspectives confirmed that fibromyalgia has a significant negative impact on the quality of social and economic functions in patients' lives. One report suggested that approximately 15% of the people with fibromyalgia are receiving disability benefits. Disability rates as high as 44% in fibromyalgia patients have been reported.
A prospective study from Denmark reported a 10-fold increased risk of death from suicide in patients with fibromyalgia who were followed for as long as 16 years. [98] This study also found a six-fold increased risk of liver cirrhosis/biliary tract disease and a three-fold increased risk of cerebrovascular disease. [98] Owing to the severity of these risks, these associations need to be studied in other populations and all patients should be monitored for suicide risk.
Patient Education
Education is an essential element in fibromyalgia management. It begins with an empathetic manner on the part of the physician, who must affirm the patient's pain, explore social and behavioral variables (both in childhood and current) that influence the illness, and explain to the patient how stress and distress can amplify the severity of symptoms. Scheduling time to provide this education at early visits can save time in subsequent visits.
The patient should be encouraged to foster self-efficacy, and healthcare providers should work to diminish dependence over time. Providers can help by teaching patients about the following:
-
Identifying triggers of flare-ups, so as to avoid and manage them
-
Sleep hygiene
-
Diet
-
Physical activity recommendations including stretching, resistance, and aerobic activity
For patient education information, see the Fibromyalgia Health Center. Other valuable educational resources include the following:
-
MedlinePlus Health Information, a service of the US National Library of Medicine and the National Institutes of Health
-
FamilyDoctor.org, an American Academy of Family Physicians Web site
Friends International Support is an online support group for people with chronic pain, fibromyalgia, chronic fatigue syndrome (myalgic encephalopathy), and back pain. Local patient support groups can also be helpful if the overall tenor of meetings is one of optimism and realism rather than pessimism and quick-fix orientation.
-
A neurophysiologist's view of pain. Courtesy of Alan R. Light, PhD.
-
Tender points in fibromyalgia.
-
Pressure algometer (dolorimeter).
-
Biopsychosocial model of fibromyalgia.