Overview
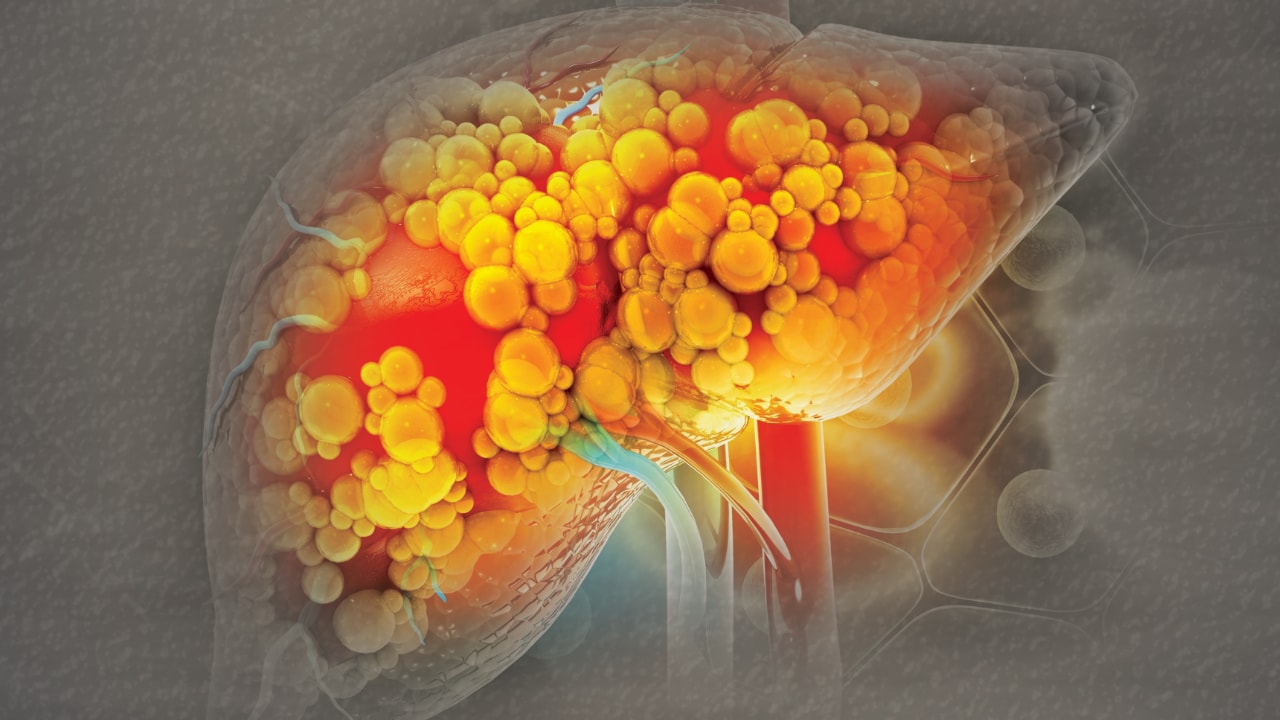
Fatty liver is the accumulation of triglycerides and other fats in the liver cells. The amount of fatty acid in the liver depends on the balance between the processes of delivery and removal. In some patients, fatty liver may be accompanied by hepatic inflammation and liver cell death (steatohepatitis). Potential pathophysiologic mechanisms for fatty liver include the following:
-
Decreased mitochondrial fatty acid beta-oxidation
-
Increased endogenous fatty acid synthesis or enhanced delivery of fatty acids to the liver
-
Deficient incorporation or export of triglycerides as very low-density lipoprotein (VLDL)
No single pathway of cause and effect has been found. However, some studies show higher levels of activation of Hedgehog pathways in patients with the most advanced fatty liver disease. [1] Tripodi et al reported that in nonalcoholic fatty liver disease (NAFLD), a procoagulant imbalance progresses from steatosis to metabolic cirrhosis, which may be caused by an increase in factor VIII and a reduction of protein C. [2] The investigators speculated that this imbalance could play a role in the risk for cardiovascular disease and liver fibrosis, conditions commonly associated with NAFLD.
The American Association for the Study of Liver Diseases (AASLD) defines NAFLD as an overarching term that encompasses all disease grades and stages as well as refers to individuals in whom 5% or more of their hepatocytes demonstrate macrovesicular steatosis when there is no easily identified alternative cause of steatosis, such as medications, starvation, momogenic conditions, in those who drink little to no alcohol (women: < 20 g/d; men: < 30 g/d). [3] NAFLD includes NAFL (nonalcoholic fatty liver) (macrovesicular hepatic steatosis with or without mild inflammation) and NASH (nonalcoholic steatohepatitis) (additionally characterized by inflammation and cellular injury [ballooning], with/without fibrosis, cirrhosis.) [3]
Pathologic changes observed in patients with alcoholic liver disease (ALD) can be divided into the following three groups:
-
Alcoholic fatty liver (simple steatosis)
-
Alcoholic hepatitis
-
Alcohol-related cirrhosis
Alcoholic fatty liver is an early and reversible consequence of excessive alcohol consumption. Fatty liver develops in every individual who consumes more than 60 g of alcohol per day. Many mechanisms of ethanol-induced fatty liver have been proposed. Increased hepatic levels of glycerol 3-phosphate (3-GP) after ethanol ingestion are related to an increase in the ratio of the oxidized form of nicotinamide adenine dinucleotide (NAD+) to the reduced form (NADH) in the liver. A higher concentration of 3-GP results in enhanced esterification of fatty acids.
An increase in free fatty acids has also been incriminated in the pathogenesis. Large amounts of alcohol enhance lipolysis through direct stimulation of the adrenal-pituitary axis. In addition, chronic ethanol ingestion inhibits oxidation of fatty acids in the liver and the release of VLDL into the blood. All of these mechanisms favor steatosis. Centrilobular localization of steatosis results from decreased energy stores caused by relative hypoxia and a shift in lipid metabolism, along with a shift in the redox reaction as a result of preferential oxidation of alcohol in the central zone.
Advances in the understanding of the pathogenesis of alcoholic steatosis have provided some useful insights, including the role of peroxisome proliferator-activated receptor alpha, which is crucial for the regulation of hepatic fatty acid metabolism. Its blockade, in animal models, along with ethanol consumption, contributes to the development of alcoholic fatty liver. In addition, induction of adiponectin, a hormone secreted by adipocytes, has been implicated in the protective effect of saturated fat against the development of alcoholic fatty liver in mice.
The role of the early growth response-1 (EGr-1) transcription factor is thought to be essential for ethanol-induced fatty liver injury in mice. Hepatocyte death by apoptosis occurs in alcoholic fatty liver and has been demonstrated in rats and mice after ethanol feeding. This may be related to mitochondrial proteins that regulate apoptosis and necrosis and that are shown to be induced in mouse fatty liver models.
Serum leptin, a cytokine-type peptide hormone mainly produced by adipocytes, may play an important role in the pathogenesis of steatosis. Steatosis occurs with decreased leptin action, whether due to leptin deficiency or resistance. In patients with alcoholic liver disease, the serum leptin level appears to be independently correlated with the grade of steatosis.
Data from animal studies and clinical studies support the role of proinflammatory cytokine tumor necrosis factor alpha (TNF-alpha) in the early stages of fatty liver, as well as in alcoholic steatohepatitis.
Etiology
The condition most commonly associated with fatty liver disease is metabolic syndrome. This includes conditions such as type II diabetes, obesity, and hypertriglyceridemia.
Other factors, such as drugs (eg, amiodarone, tamoxifen, methotrexate), alcohol, metabolic abnormalities (eg, galactosemia, glycogen storage diseases, homocystinuria, and tyrosinemia), nutritional status (eg, overnutrition, severe malnutrition, total parenteral nutrition [TPN], or starvation diet), or other health problems (eg, celiac sprue and Wilson disease) may contribute to fatty liver disease. There are reports of lean families with nonalcoholic steatohepatitis (NASH). Low and high birth weights appear to not only increase the risk for development of pediatric NAFLD but also raise the risk for more severe disease. [4] Male sex may also be a risk factor, but this remains controversial. [5]
Several risk factors may influence the development of advanced alcoholic liver disease (ALD), including the following:
-
Minimum amounts of alcohol intake associated with an increased risk of ALD range from 40 to 80 g/day for 10-12 years; safe limits for alcohol use are not clearly defined
-
Genetics play a role in alcohol consumption and alcoholism; early data suggested a genetic predisposition to the development of ALD, mostly related to differences in major hepatic enzymes involved in the metabolism of alcohol (eg, alcohol dehydrogenase [ADH], acetaldehyde dehydrogenase [ALDH], and the cytochrome P-450 system [CYP4502E1])
-
Several studies demonstrate a high prevalence of hepatitis C virus (HCV) antibody in patients with ALD, as well as iron overload
-
Obesity and dietary habits have been implicated in individual susceptibility to ALD
Epidemiology
United States statistics
Steatosis affects approximately 25%-30% of the general population. [3] Steatohepatitis may be related to alcohol-induced hepatic damage or may be unrelated to alcohol (ie, nonalcoholic steatohepatitis [NASH]). Approximately 17.6 million people in the United States abuse or depend on alcohol, with several million more who binge drink that may evolve into problems with alcohol over the long term. [6]
Fatty liver develops in 90%-100% of heavy alcohol users, [7, 8] but only about 10%-20% of chronic heavy drinkers develop clinically important alcoholic fatty liver disease (ALD) (eg, alcoholic hepatitis, cirrhosis). [9] NASH has been detected in 1.2%-9% of patients undergoing routine liver biopsy. Nonalcoholic fatty liver disease (NAFLD) is found in over 80% of patients who are obese, and more than 50% of patients undergoing bariatric surgery have NASH. [9]
International statistics
Worldwide, the prevalence of NAFLD and NASH continues to increase in parallel with that of obesity and metabolic comorbid disease (insulin resistance, dyslipidemia, central obesity, hypertension). [3]
An observational study from northern Italy demonstrated prevalence rates of steatosis in 46.4% of heavy drinkers (>60 g/day of alcohol) and in 94.5% of obese heavy drinkers. [10] Danish and Australian studies of NASH showed less intense disease progression than studies in the United States. [11] Asian studies reported NASH and NAFLD occurring at a lower body mass index (BMI). [12, 13, 14]
Age-related demographics
Fatty liver occurs in all age groups. With respect to alcoholic steatosis, the liver handles alcohol differently as the body ages, and alcohol toxicity increases with age because of increased organ susceptibility. These phenomena are thought to be related to a mitochondrial transport defect developing with age, as well as to decreased function of the smooth endoplasmic reticulum and metabolism of CYP2E1-dependent microsomal ethanol oxidation.
NAFLD is the most common liver disease among adolescents in the United States, including about 8% of lean teens. [15] However, findings from the Project Viva study indicate that pediatric overweight or obesity as early as age 8 years increases the risk of development of NAFLD. [16, 17] Older age often is predictive of more severe grading of fibrosis. NASH is the most common cause of chronic liver disease in adults in the United States (followed by ALD and hepatitis C). [18] It is now probably the leading reason for mild elevations of transaminases. NASH has recurred within 6 months after pediatric or adult liver transplantation. [19, 20, 21]
Sex-related demographics
Women develop more severe ALD more quickly and at lower doses of alcohol than men do. The increased susceptibility of females may be related to sex-dependent differences in the hepatic metabolism of alcohol, cytokine production, and the gastric metabolism of alcohol. In initial studies of NAFLD, the percentage of female patients was reported to be as high as 75%; however, in subsequent studies, the percentage fell to roughly 50%.
Race-related demographics
Findings from a 2016 study demonstrated that the causes and prevalence of chronic liver disease and cirrhosis vary widely among different racial/ethnic groups. [18] Japanese Americans (6.9%) and Latinos (6.7%) appear to be the most affected by chronic liver disease, followed by white persons (4.1%) as well as black persons and Native Hawaiians (3.9%). NAFLD was the most common etiology of chronic liver disease and of cirrhosis among all the groups; however, the most common causes of cirrhosis by ethnicity were NAFLD in Japanese Americans, Native Hawaiians, and Latinos; ALD in white persons; and hepatitis C in black persons. [18]
Very little data are available on racial differences in the incidence of ALD; however, some studies have suggested overall differences. A study of 42,862 US adults showed differences in drinking patterns among different races; white individuals were the most likely to drink, but black individuals had the highest volume of intake and frequency of heavy drinking. [22] Other studies have shown a higher rate of cirrhosis among black persons.
Fatty liver has been found across all races, but NAFLD is most common in white persons, and it is in this population that most of the research has been done. In general, Hispanics do not have higher rates of NASH than white patients unless diabetes is also present. [23] Mutations for hemochromatosis appear to put white individuals at a higher risk for more advanced fibrosis. [24]
A small study evaluating fatty liver disease in the Indian population found its association with the nonobese and its recovery with simple lifestyle habits. [14] However, obesity, when present, was a significant risk factor for NASH in Indians, as well as in Koreans. [13]
It has been observed (and is supported in the author’s clinical practice) that Asian patients often develop NAFLD and NASH at BMIs that are in the normal range for the patient’s ethnicity but tend toward the higher end of the range. A diagnosis of cirrhosis in an 80-year-old, 5-ft, 110-lb Asian female with a BMI of 21 kg/m2 is not unusual.
Prognosis
Steatosis may be reversible with weight loss, cessation of alcohol use, or both. It was once believed to be a benign condition that only rarely progressed to chronic liver disease; however, steatohepatitis may progress to liver fibrosis and cirrhosis and may result in liver-related morbidity and mortality.
Simple alcoholic steatosis is rarely fatal. With complete abstinence, histologic changes generally return to normal within 2-4 weeks. Continued alcohol consumption may result in more advanced forms of liver disease, either alcoholic hepatitis or cirrhosis. Although alcoholic steatosis usually is considered a benign lesion with a favorable prognosis once alcohol consumption is discontinued, several prognostic factors have been described in the literature that may indicate advancement to more severe lesions in patients who continue to drink.
For example, in a study from England that followed 88 patients with fatty liver for a mean of 10.5 years, 9 of the patients developed cirrhosis, and 7 developed fibrosis; all but 1 of these 16 patients had continued to use alcohol. [25] Histologic predictors of progression at the time of fatty liver included the presence of mixed macrovesicular/microvesicular fat and giant mitochondria.
Patients with alcoholic fatty liver are at high risk of the development of cirrhosis and increased mortality associated with the severity of steatosis in the index liver biopsy. The presence of histologic cholestasis in association with alcoholic steatosis does not appear to be of prognostic significance in determining the risk of progression to cirrhosis. Investigators of a retrospective study noted that, despite a lower incidence of hepatocellular carcinoma, alcoholic liver disease (ALD) confers a worse prognosis in patients with cirrhosis than those with chronic hepatitis C infection or nonalcoholic fatty liver disease (NAFLD)-related cirrhosis. [26]
A study from Denmark that used the Danish National Registry noted an increase in mortality among patients with a hospital discharge diagnosis of alcoholic fatty liver; this increase remained after the censoring of patients with a diagnosis of cirrhosis. [27]
Long-term natural history studies of patients with NAFLD who undergo repeat biopsies have shown that 30% progress, 30% remain stable, and 30% improve over a 3-year period without pharmacologic intervention. [28] Abnormal glucose tolerance testing is an independent risk factor for progression of nonalcoholic steatohepatitis (NASH). [29]
A natural history study from Olmsted County, Minnesota, revealed that over the 10-year study period, mortality was 10% higher in NAFLD patients than in control subjects. [30] Malignancy and heart disease were the top two causes of death. Liver-related disease was the third leading cause of death (13%) for NAFLD patients but only the 13th most common cause of death (< 1%) for control subjects.
In general, the majority of patients with NAFLD without advanced fibrosis die from cardiovascular disease and nonhepatic malignancy, and then liver disease. [3] Individuals with advanced fibrosis most commonly die from liver disease.
In a study by Bhala et al evaluating mortality in 500 patients with chronic hepatitis C or NASH, patients with hepatitis C were more likely to die of liver-related disease; however, long-term mortality for NASH was equivalent to that for hepatitis C, probably because of the increase in cardiovascular causes of death found in the NASH patients. [31]
Fibrosis or cirrhosis of the liver is present in 15%-50% of patients with NASH. Approximately 30% of patients with fibrosis develop cirrhosis after 10 years. Many cases of cryptogenic cirrhosis may represent so-called burnt-out NASH because a high percentage of such cases are associated with obesity, type II diabetes, or hyperlipidemia.
Some patients with drug-induced fatty liver present dramatically with rapid evolution of hepatic failure. Some patients with inborn errors of metabolism (eg, tyrosinemia) may rapidly progress to cirrhosis.
Complications
Continued alcohol consumption may result in a more advanced form of liver disease, either alcoholic hepatitis or cirrhosis. In a study from Denmark, using a population-based National Registry, investigators noted an increased mortality and an increased cancer risk, particularly liver cancer, among patients discharged with a diagnosis of alcoholic fatty liver. [27]
In patients with NAFLD, steatohepatitis may progress to cirrhosis, accompanied with complications that include variceal bleeding, ascites, encephalopathy, and liver failure. The rate of progression appears to be worse if more than one liver disease (eg, alcoholic liver disease [ALD] or chronic viral hepatitis) is present. Uncontrolled diabetes and hypertriglyceridemia also appear to predict worse fibrosis. [30, 32, 33, 34] The rate of formation of hepatocellular carcinoma appears to be the same as with other forms of liver disease, [35] although NAFLD appears to increase the risk for hepatocellular carcinoma in patients whose livers are not cirrhotic. [36] NAFLD also appears to be a strong and independent risk factor for prediabetes in the general adult population. [37]
Patient Education
Fatty liver was once considered to be an entirely benign condition, but it is now clear that this is not always the case. Thus, patient education on dietary decisions and portions is essential. Nutrition and lifestyle education are the mainstays of therapy. Ideally, during every healthcare provider encounter, the issues of food choices, food portions, and exercise, including weight-bearing exercise, should be emphasized and reviewed. In addition, the American Diabetes Association and other organizations offer excellent dietary and lifestyle advice.
Patients with heavy alcohol use (men: >3 drinks per day; women: >2 drinks per day) for longer than 5 years should be counseled that they are at an increased risk for alcoholic liver disease. [8]
Patients with alcoholic fatty liver should be counseled on the detrimental role alcohol plays in their liver problem and the likely progression to more advanced liver disease with continued alcohol use. It is important to emphasize abstinence from alcohol early and continuously so as to optimize its beneficial effects. Abstinence improves liver histology, decreases portal hypertension, and decreases, but does not eliminate, the development of cirrhosis. Alcohol rehabilitation should be offered to all patients, with an understanding of the addictive nature of alcoholism.
Patient handouts on alcoholic liver disease (ALD) are available; these can be provided during inpatient or outpatient visits. Patient family and social support play a central role in the patient’s abstinence from alcohol. Additional resources and support can be obtained from the following organizations:
Alcoholics Anonymous (AA)
Postal address: A.A. World Services, Inc, PO Box 459, Grand Central Station, New York, NY 10163; Phone: (212) 870-3400
Office address: A.A. World Services, Inc, 475 Riverside Drive at West 120th St, 11th floor, NY, NY 10115; Phone: (212) 870-3400
Global AA regional contact information is available at: https://www.aa.org/pages/en_US/communication-with-the-general-service-office-gso-of-aa-in-new-york-city
National Institute on Alcohol Abuse and Alcoholism (NIAAA) – E-mail: niaaaweb-r@exchange.nih.gov
National Council on Alcoholism and Drug Dependence, Inc (NCADD): 217 Broadway, Suite 712, New York, NY 10007; Phone: 212-269-7797; Fax: 212-269-7510; e-mail: national@ncadd.org
Substance Abuse and Mental Health Services Administration (SAMHSA): Headquarters and mailing address: 5000 Fishers Lane, Rockville, MD 20857; Phone: 877-SAMHSA-7 (877-726-4727) or 800-487-4889 (TTY)
For patient education resources, see the Mental Health Center, the Digestive Disorders Center, and the Infections Center, as well as Alcoholism, Hepatitis A (HAV, Hep A), Hepatitis B (HBV, Hep B), Hepatitis C, and Cirrhosis.
Presentation
History
Fatty liver occurs commonly after the ingestion of a moderate or large amount of alcohol, even for a short period of time. Alcohol-induced steatosis usually is asymptomatic. Severe fatty infiltration of the liver can result in symptoms of malaise, weakness, anorexia, nausea, and abdominal discomfort. Jaundice is present in 15% of patients admitted to the hospital.
A thorough clinical history, especially with regard to the amount of alcohol consumption, is essential for determining the role of alcohol in the etiology of abnormal liver test results. History obtained from family members may reveal past alcohol-related problems. No specific test is available to rule out drug-related toxicity, but a good review of all concurrent and recent medications, including over-the-counter medications and alternative treatments, is valuable in evaluating the possible causes of abnormal liver test results.
The 2010 American Association for the Study of Liver Diseases (AASLD) practice guideline for alcoholic liver disease (ALD) recommends the following for diagnosis [38] :
-
If alcohol abuse or excess is suspected from discussion of alcohol use with the patient, screen the patient for alcohol abuse using a structured questionnaire such as the Alcohol Use Disorders Identification Test (AUDIT).
-
If the patient’s history or a screening test indicates alcohol abuse, use laboratory testing to verify the diagnosis of ALD and rule out other considerations.
-
If ALD is confirmed, test for other alcohol-related organ damage.
Most patients with nonalcoholic fatty liver disease (NAFLD) are asymptomatic. However, if questioned, more than 50% of patients with fatty liver or nonalcoholic steatohepatitis (NASH) report persistent fatigue, malaise, or upper abdominal discomfort.
Symptoms of liver disease, such as ascites, edema, and jaundice, may arise in patients with cirrhosis due to progressive NASH. Laboratory abnormalities during blood donations or life insurance physical examinations often reveal elevated alanine aminotransferase (ALT) levels and ultimately lead to the diagnosis of fatty liver disease.
Physical Examination
Alcoholic fatty liver may be present in the absence of any abnormalities noted on the physical examination. Hepatomegaly is common in patients who are hospitalized, occurring in over 70% of persons with steatosis proven on biopsy. Portal hypertension is rare in alcoholic steatosis. Extrahepatic effects, such as skeletal muscle wasting, cardiomyopathy, pancreatitis, or peripheral neuropathy, may be present.
Hepatomegaly is also common with nonalcoholic fatty liver disease (NAFLD). Splenomegaly and stigmata of portal hypertension (eg, ascites, edema, spider angiomas, varices, gynecomastia, and menstrual disorders) may occur in patients with cirrhosis. Patients with drug-induced fatty liver may present with rapid fulminant liver failure.
Differential Diagnosis
The differential diagnosis is broad and includes the following conditions:
Primary Sclerosing Cholangitis
Steatosis can be observed on histology in the following conditions:
-
Alcohol excess
-
Starvation
-
Total parenteral nutrition (TPN)
-
Nonalcoholic steatohepatitis (NASH) – A diagnosis of NASH can be established only when alcohol excess (>10 g/day) can be excluded
-
Drug-induced liver disease (eg, disease caused by valproic acid, tetracycline, antiviral agents such as zidovudine, amiodarone, perhexiline maleate, methotrexate, corticosteroids, or estrogens)
-
Acute fatty liver of pregnancy [39] – This can occur during pregnancy and likely results from maternal-fetal interactions related to genetic abnormalities in the mitochondrial beta-oxidation of fatty acids
-
Metabolic liver disease and other inborn errors of metabolism
-
Reye syndrome
AASLD/ACG/AGA Guidelines for Workup of NAFLD
Recommendations from a 2018 practice guideline from the American Association for the Study of Liver Diseases (AASLD), the American College of Gastroenterology (ACG), and the American Gastroenterological Association (AGA) regarding the workup of nonalcoholic fatty liver disease (NAFLD) are below, [40] with the updated 2018 AASLD recommendations incorporated. [5]
-
Clinicians should look for metabolic risk factors and alternate etiologies for hepatic steatosis in patients who have other types of chronic liver disease and who also have steatosis and steatohepatitis.
-
Patients with nonalcoholic steatohepatitis (NASH) cirrhosis should be screened for gastroesophageal varices and should be considered for hepatocellular carcinoma screening.
-
Screen patients with NAFLD for type 2 diabetes. [3]
-
Screening for NAFLD is not advised in adults attending primary care clinics or high-risk groups attending diabetes or obesity clinics because of uncertainties surrounding diagnostic tests, treatment options, long-term benefits, and cost-effectiveness.
-
Patients with diabetes should be screened for advanced fibrosis. [3] Clinicians should have a high index of suspicion for NASH and NAFLD in patients with type 2 diabetes; decision aids such as the NAFLD Fibrosis Score (NFS), vibration-controlled transient elastography (VCTE), or the Fibrosis-4 Index (FIB-4) can be used to determine those individuals who are at risk for advanced fibrosis.
-
Systematic screening of family members of patients with NAFLD is currently not recommended.
-
Competing etiologies for steatosis and coexisting common chronic liver disease must be excluded in patients with suspected NAFLD.
-
Liver biopsy should be considered in patients with suspected NAFLD in whom competing etiologies for hepatic steatosis and coexisting chronic liver diseases cannot be otherwise excluded.
-
Persistently high serum ferritin levels and increased iron saturation may warrant a liver biopsy, especially in patients with homozygous or heterozygous C282Y HFE (hemochromatosis) gene mutations.
-
Patients with high serum titers of autoantibodies and other features suggesting autoimmune liver disease (eg, very high aminotransferases or high globulin levels) should undergo a more thorough workup for autoimmune liver disease.
-
Patients with suspected NAFLD should be considered for evaluation of commonly associated comorbidities, such as dyslipidemia, obesity, insulin resistance or diabetes, hypothyroidism, polycystic ovary syndrome, and sleep apnea.
-
Metabolic syndrome predicts the presence of steatohepatitis in patients with NAFLD and can therefore be used to target patients for a liver biopsy.
-
The NFS or FIB-4 helps to identify patients with NAFLD who have a higher likelihood of having bridging fibrosis or cirrhosis.
-
VCTE, magnetic resonance elastography (MRE), or the enhanced liver fibrosis (ELF) score are clinically useful tools for identifying advanced fibrosis in patients with NAFLD. [3]
-
Metabolic syndrome, NFS, or FIB-4, or liver stiffness measured by VCTE or MRE, may be used to identify patients at risk for advanced fibrosis or steatohepatitis.
The 2023 AASLD guidelines further recommend the following [3] :
-
Regularly assess alcohol intake in individuals with NAFLD, as alcohol can be a cofactor for liver disease progression.
-
Those with clinically significant hepatic fibrosis (≥F2) should completely abstain from alcohol use.
The 2018 ACG guidelines on alcoholic liver disease (ALD) provided the following guidance [8] :
-
Liver function tests and ultrasonography are recommended for patients with harmful alcohol use and/or alcohol disorders.
-
Liver biopsy is not routinely recommended for diagnosis of alcoholic fatty liver disease, but it and noninvasive tools of fibrosis may be considered for diagnosis of steatohepatitis and/or liver fibrosis.
-
The Alcohol Use Disorders Inventory Test (AUDIT) is validated for identifying individuals with alcohol use and dependence.
Laboratory Studies
Fasting insulin and glucose levels will alert the clinician to potential glucose intolerance and may lead to more effective therapies.
An increase in the levels of glutamyl transpeptidase (GGT) may be related to alcohol use, but this study lacks specificity and sensitivity, and as many as 70% of people who abuse alcohol have normal values.
In rare cases, patients with alcoholic steatosis have severe cholestasis. Ballard et al described five patients with alcoholic steatosis who presented with jaundice, all of whose liver biopsy results showed severe steatosis and marked cholestasis with little hepatic fibrosis. Hepatic failure characterized by progressive encephalopathy and coagulopathy developed in and led to death in two patients. [41] In a large cooperative study of alcoholic liver disease (ALD) conducted by the Department of Veterans Affairs (VA), histologic cholestasis was observed in only 19% of patients with alcoholic steatosis.
Macrocytosis (increased mean cell volume) is common in patients with ALD, with a low sensitivity (27%-52%) and a high specificity (85%-91%). Serum carbohydrate-deficient transferrin (CDT) is a specific and sensitive test for alcoholism in patients whose alcohol intake exceeds 60 g/day.
Hypertriglyceridemia, steatosis, and hemolysis (Zieve syndrome) may be associated with alcohol abuse. Hyperlipidemia may be present in nonalcoholic fatty liver disease (NAFLD). Increased triglycerides are common in children and in patients with metabolic syndrome.
The alkaline phosphatase (ALP) level can be elevated in some patients with nonalcoholic steatohepatitis (NASH). Usually, it is less than twice to three times normal.
Abnormal levels of aminotransferases (ie, aspartate aminotransferase [AST] and alanine aminotransferase [ALT]) and bilirubin are found in about one third of hospitalized patients with alcohol-induced steatosis. In such patients, elevated bilirubin levels largely result from an increase in the indirect reacting fraction and may reflect alcohol-associated hemolysis. AST levels are usually higher than ALT measurements. The absolute values of serum AST and ALT are almost always less than 500 IU/L.
An elevated AST or ALT level may be the only abnormality in patients with fatty liver; these levels may be elevated as much as 10-fold. However, AST and ALT levels may be normal in some patients with fatty liver or NASH. In the absence of cirrhosis, an AST-to-ALT ratio greater than 2 suggests alcohol use, whereas a ratio of less than 1 may occur in patients with NASH.
Viral serologies for hepatitis C should be obtained to identify or exclude viral infection. In addition, iron levels and total iron-binding capacity (TIBC) should be measured, and abnormal results from liver function tests should be evaluated as indicated.
Elevations in serum ferritin or iron levels, decreased transferrin saturation, or both may occur in patients with NASH. Although iron overload occurs in a small proportion of patients with NASH, these patients have more severe disease. Evidence exists that a serum ferritin greater than 1.5 times the upper limit of the normal range in patients with NAFLD is associated with a higher NAFLD activity score (and thus, NASH) and with advanced hepatic fibrosis. [42] An iron index score may be ordered on a liver biopsy specimen to evaluate for phlebotomy. Hemochromatosis gene testing is recommended when the ferritin is significantly elevated. Simply eliminating dietary iron has been shown to improve fatty liver.
Autoimmune markers, such as antinuclear antibody (ANA) and anti–smooth muscle antibody (ASMA), are often slightly elevated in NASH. Positive antibodies are associated with more severe fibrosis levels. In the appropriate clinical setting, serum protein electrophoresis (SPEP) and anti–liver-kidney antibody may lead to a diagnosis of autoimmune liver disease.
Often, a clinical picture of obesity, hypertriglyceridemia, and elevated transaminases is enough to allow the clinician to conclude that a patient has NASH. However, underlying alcohol or other drug ingestion, as well as smoldering autoimmune disease or hemochromatosis, must be ruled out. Referral to a hepatologist with or without liver biopsy may help in staging and prognosis.
Although NAFLD is more common in men with androgen deficiency, the AASLD does not recommend routine assessment of testosterone levels. [3] However, in the setting of hypogonadism, suggested on the basis of clinical signs/symptoms, the AASLD indicates that this condition should be treated.
Serum beta-trophin level may have potential as a new marker for noninvasive evaluation of NAFLD and liver fibrosis, according to a study by Cengiz et al. [43] In their cohort of 69 patients with NAFLD and 69 healthy control subjects, serum beta-trophin levels were lower in the NAFLD group; those with mild fibrosis had elevated serum beta-trophin levels compared to those with significant fibrosis. In multivariate and ROC (receiver operating characteristic) analyses, levels of serum beta-trophin was, respectively, an independent predictor of significant fibrosis and was statistically significant in identifying significant fibrosis. [43]
Findings from the Multi-Ethnic Study of Atherosclerosis (MESA) appear to indicate that circulating interleukin-6 (IL-6) is a biomarker for coronary atherosclerosis in NAFLD. [44] IL-6 had an independent association with the prevalence and severity of subclinical atherosclerosis.
In a separate study, Abdel-Razik et al proposed mean platelet volume and the neutrophil-lymphocyte ratio as novel inexpensive and simple markers of inflammation to predict fibrosis in patients with NAFLD as well as to predict the presence of NASH. [45] The investigators noted that patients with NASH had elevated levels of mean platelet volume and neutrophil-lymphocyte ratio compared to those without NASH, as well as in patients with advanced fibrosis compared to those with early fibrosis. [45]
Ultrasonography, CT Scanning, and MRI
Noninvasive studies such as ultrasonography (US), computed tomography (CT) scanning, and magnetic resonance imaging (MRI) are useful in helping to establish a diagnosis of steatosis, as well as in finding evidence for portal hypertension; these imaging tests are also helpful in ruling out biliary dilation (eg, choledocholithiasis) in patients with a cholestatic pattern of liver test result abnormalities. However, these imaging modalities can neither define the cause of steatosis nor reliably distinguish between benign steatosis and steatohepatitis. Benign steatosis may be focal or diffuse, whereas steatohepatitis is usually diffuse.
Standard US detects hepatic steatosis, but the American Association for the Study of Liver Diseases (AASLD) does not recommend it as a tool to identify this condition owing to low sensitivity across the spectrum of NAFLD. [3] However, as a point-of-care technique, the controlled attenuation parameter (CAP) may be used to identify steatosis, and MRI-PDFF (proton density fat fraction) can quantify steatosis. [3]
In patients with alcoholic steatosis, the liver appears diffusely echogenic on US. In patients with nonalcoholic fatty liver disease (NAFLD), the liver is hyperechogenic or bright. Steatosis is detected only when substantial (≥ 30%) fatty change is present. Studies in patients who are about to undergo gastric bypass surgery indicate that US has a 93% predictive value for NAFLD, with an accuracy of 76%. Patients with steatosis on US have a higher incidence of coronary artery disease and should undergo cardiac evaluation if suspicious symptoms are present. [46]
The mean CT (Hounsfield unit) count is lower in the liver than in the spleen. CT scans may be used to monitor the course of the disease on successive scans. Focal fatty lesions may be identified by dual-energy CT scans that demonstrate increased attenuation with increasing energy.
MRI may be useful for excluding fatty infiltration. Phase-contrast imaging correlates with the quantitative assessment of fatty infiltration across the entire range of liver disease. Loss of intensity on T1-weighted images may be useful in identifying focal fat. More recently, investigators indicate that two-dimensional magnetic resonance elastography (MRE) can measure shear hepatic stiffness as a biomarker of fibrosis in children with NAFLD, but further investigation is needed to better refine, validate, and integrate MRE into clinical protocols. [47]
Predictive Measures
Because fatty liver is common in the Western world and because nonalcoholic steatohepatitis (NASH) carries a 10% risk of cirrhosis, it would be desirable to have a simple blood test that could predict which patients will have worse disease. The search for such a test has led to studies of databases, rat models, scoring systems, prospective studies, and novel uses for old markers of inflammation and scarring. [13, 48, 49, 50, 51]
The readily obtained nonalcoholic fatty liver disease (NAFLD) fibrosis score—consisting of age, hyperglycemia, body mass index (BMI), platelet count, albumin level, and ratio of aspartate aminotransferase (AST) to alanine aminotransferase (ALT)—appears easy to use for this purpose and promising for helping to avoid excessive liver biopsies. [52]
Another promising tool is the method Kotronen et al developed for predicting NAFLD, which is based on routinely available clinical and laboratory data. [53] Analysis of 470 subjects in whom liver fat content was measured with proton magnetic resonance spectroscopy showed the following to be independent predictors of NAFLD [53] :
-
Presence of metabolic syndrome and type 2 diabetes
-
Fasting serum insulin
-
Fasting serum AST
-
AST-to-ALT ratio
Validation of the score demonstrated an area under the receiver operating characteristic curve of 0.86. [53] The optimal cut-off point of –0.640 predicted increased liver fat content with a sensitivity of 86% and a specificity of 71%.
Other noninvasive commercial tests for fibrosis (eg, FIBROSpect, FibroSURE, and FibroScan) have not yet been proved useful for NASH in Western populations.
Liver Biopsy and Histopathologic Examination
Liver biopsy and histopathologic examination are important components of the diagnostic evaluation in patients with suspected alcoholic liver disease (ALD). They are the most sensitive and specific means of evaluating the degree of liver cell injury and hepatic fibrosis. Several reasons justify obtaining a liver biopsy in patients with ALD, including the following:
-
Confirming the diagnosis
-
Excluding other unsuspected causes of liver disease
-
Assessing the extent of liver damage
-
Defining the prognosis
In making the decision on whether to perform a biopsy, it is important to consider the strength of the clinical diagnosis and the role that the biopsy findings would have in guiding therapeutic options. For patients who are unlikely to receive specific treatments or who have conditions that make a biopsy unsafe, the 2018 ALD guideline recommends including procedure risk in the biopsy decision. [5]
A liver biopsy and histopathologic examination are required to establish the diagnosis of nonalcoholic fatty liver disease (NAFLD). The diagnosis should be considered in all patients with unexplained elevations in serum aminotransferases (eg, with findings negative for viral markers or autoantibodies or with no history of alcohol use). It should also be considered in patients with NAFLD who are at increased risk of having steatohepatitis and/or advanced fibrosis. [5] The Brunt classification is the standard used to report NAFLD and nonalcoholic steatohepatitis (NASH) biopsy specimens. [54]
Histologic findings
Histologically, fatty liver is characterized by fat accumulation, which is most prominent in the pericentral (centrilobular) zone. Macrovesicular steatosis is the rule; hepatocytes containing one or more large fat droplets displace the nucleus to an eccentric position. Occasional lipid release from rupture of distended hepatocytes may produce a mild localized inflammatory response (lipogranulomas) composed predominantly of macrophages and occasional lymphocytes.
Although infiltration of liver with inflammatory cells typically is not prominent in patients with steatosis alone, in some instances, fibrosis around terminal venules (ie, perivenular fibrosis) or hepatocytes (ie, pericellular fibrosis) has been noted. Early changes observed with the electron microscope include accumulation of membrane-bound fat droplets, proliferation of smooth endoplasmic reticulum, and gradual distortion of mitochondria. Microvesicular steatosis also is being recognized with increasing frequency.
Alcoholic foamy degeneration (microvesicular fatty change) was the term used by Uchida et al to describe a clinical syndrome in people with chronic alcoholism. [55] The syndrome is characterized by jaundice and hyperlipidemia and is associated with striking microvesicular steatosis and abundant giant mitochondria observed on liver biopsy.
Specific histologic findings in NAFLD or NASH include the following:
-
Steatosis, which usually is macrovesicular but may be microvesicular or mixed
-
Inflammatory infiltrates consisting of mixed neutrophilic and mononuclear cells, usually without portal infiltrates (in contrast to hepatitis C)
-
Ballooning degeneration
-
Fibrosis
The first three findings are used to calculate the NAFLD activity score, which is determined on a scale of 0 to 8. The stage of disease is determined by the NAFLD activity score and the amount of fibrosis present.
Treatment & Management
There is no definitive pharmacologic therapy approved for treatment of nonalcoholic fatty liver disease (NAFLD). [3] However, in the appropriate clinical setting, consider medications approved to treat the associated comorbidities that have potential benefit in NAFLD. [3] Thus, management of NAFLD should include treating the associated obesity, hyperlipidemia, insulin resistance, and type 2 diabetes.
The American Association for the Study of Liver Diseases (AASLD) indicates that statins are safe and recommended to lower the risk of cardiovascular disease in those with conditions across the NAFLD spectrum, including compensated cirrhosis. [3] However, for patients with decompensated cirrhosis, there are only limited data regarding the safety and efficacy of statins, although use of these agents could be considered in populations at high CVD risk along with close monitoring.
Although alcohol-induced hyperhomocysteinemia (which has been associated with endoplasmic reticulum stress leading to apoptosis and up-regulation of lipid synthesis) and its correction by betaine have been studied in animal models, no definite role of the use of betaine to treat alcoholic fatty liver in humans is available.
Weight loss and control of comorbidities appear to slow the progress of NAFLD and may reverse some of the steatosis and fibrosis. In a randomized trial, improvement on liver biopsy was seen after a 7% weight loss resulting from lifestyle changes (improved diet, exercise, and behavioral modification). [56]
Previously, there was no established treatment available for nonalcoholic steatohepatitis (NASH). However, in March 2024, the FDA approved resmetirom (Rezdiffra) under their accelerated approval pathway, in addition to diet and exercise, for the treatment of noncirrhotic NASH in adults with moderate to advanced liver scarring (fibrosis). [57] Resmitirom, a thyroid hormone receptor beta selective agonist, is the first drug approved by the FDA for this indication.
A study by Foster et al found that atorvastatin 20 mg, combined with vitamins C and E, is effective in reducing the odds of having hepatic steatosis by 71% in healthy individuals with NAFLD after 4 years of active therapy. [58]
The 2018 and 2023 practice guidelines from the American Association for the Study of Liver Diseases (AASLD) include the following recommendations regarding treatment of NAFLD [3, 5] :
-
Weight loss of 3%-5% of body weight generally reduces hepatic steatosis, but up to 10% weight loss may be needed to improve necroinflammation.
-
A combination of reduced calorie diet and moderate intensity exercise may aid in sustaining weight loss, along with aggressive modification of cardiovascular risk factors.
-
Patients with NAFLD should not consume heavy amounts of alcohol; data are insufficient to make recommendations with regard to nonheavy alcohol consumption.
-
Pharmacologic treatments should be limited to individuals with biopsy-proven NASH and fibrosis.
-
Vitamin E 800 IU/day improves liver histology in nondiabetic adults with biopsy-proven NASH; it should therefore be considered as a first-line pharmacotherapy for this patient population, and the risks and benefits should be discussed with the patient prior to starting treatment.
-
Omega-3 fatty acids may be considered for hypertriglyceridemia in patients with NAFLD, but it is premature to recommend them for the specific treatment of NAFLD or NASH. The 2023 AASLD guidelines also recommend lifestyle changes and supplementation with omega-3 fatty acids, icosapent ethyl, or fibrates. [3]
-
Metformin is not recommended as a specific treatment for liver disease in adults with NASH.
-
Pioglitazone may be used to treat steatohepatitis in both patients with and without type 2 diabetes with biopsy-proven NASH, but the risks and benefits should be thoroughly discussed with the patient prior to initiation of treatment.
-
Glucagon-like peptide (GLP)-1 agonists have been studied to treat liver disease in patients with NAFLD or NASH; however, it is still premature to consider these agents as treatment options at this time.
-
Consider bariatric surgery as a treatment option in those who meet the criteria for metabolic weight loss surgery (resolves NAFLD or NASH in most patients without cirrhosis; lowers mortality from cardiovascular disease and malignancy). [3]
-
Foregut bariatric surgery is not contraindicated in otherwise eligible obese individuals with NAFLD or NASH but without established cirrhosis; however, it is premature to consider foregut bariatric surgery as an established option to treat NASH specifically.
-
Ursodeoxycholic acid (UDCA) and obeticholic acid (OCA) are not recommended to treat NASH or NAFLD.
-
Statins can be used to treat dyslipidemia in patients with NAFLD and NASH, but they should not be used specifically to treat NASH, pending evidence from randomized controlled trials. Statins should be avoided in patients with decompensated cirrhosis.
Abstinence from alcohol
Abstinence from alcohol may reverse steatosis in patients with alcohol-related fatty liver. The steatosis usually resolves within 2 weeks of discontinuance of alcohol. Almost all authorities agree that abstinence from alcohol improves survival and is the cornerstone of long-term management in these patients. Management of patients with alcoholism and fatty liver often requires recognition and treatment of alcohol withdrawal.
Diet and weight loss
No specific dietary restrictions are needed in patients with simple alcoholic steatosis. Patients with alcoholic fatty liver may have deficiencies of vitamins, minerals, and trace elements. Adequate replacement of these deficiencies should be a part of management. Protein-calorie malnutrition is a common finding in patients with alcoholic liver disease (ALD) and is associated with the major complications observed with cirrhosis. Consequently, it is vital to recognize and understand the significance of malnutrition in these patients.
A low-fat American Diabetes Association (ADA) diet is recommended, and a weight loss goal of 1-2 pounds per week is suggested. Diets associated with improvement include those restricted in rapidly absorbed carbohydrates and those with a high protein-to-calorie ratio. Weight loss should be gradual, moderate, and controlled. [59]
Mounting evidence indicates that high-fructose diets (eg, sodas and preserved foods) are factors for developing fatty liver and that their elimination may reverse fatty liver. [60, 61] The mechanism appears to be related to depletion of adenosine triphosphate (ATP), as well as to increased uric acid production from excess fructose. [62]
In mouse models of NASH, a high-fat diet combined with a high-fructose diet (equivalent to the typical American “fast food diet”) resulted in more liver damage than a high-fat diet alone. [60] In a study of rats on a high-fructose diet, exercise (swimming 1 hour a day, 5 days a week) prevented the development of fatty liver disease. [61]
NAFLD can be prevented in most patients by taking the following measures:
-
Eating appropriate portions
-
Eating healthy choices
-
Exercising regularly
Treatment of the underlying disease
Patients with celiac sprue who follow a gluten-free diet can experience reversal of fatty liver disease. Patients with growth hormone deficiency who receive growth hormone can experience reversal of NASH. [63]
Exercise
Multiple human studies have shown that exercise added to diet appears to improve the results and increase insulin sensitivity by increasing muscle mass. Exercise that includes both cardiovascular fitness and weight training should improve NASH. Cardiovascular fitness often results in weight loss. Weight training will increase the muscle mass and improve insulin sensitivity. Combining these two activities helps relieve the underlying derangements of NASH.
Even regular exercise that is not associated with weight loss has been shown to improve fatty liver disease. [61, 64, 65] An Australian study evaluating just 4 weeks of cycling exercise found that despite no change in body weight, liver cholesterol levels improved. [64] A California study involving more than 800 adults with fatty liver found that vigorous exercise was associated with less severe scar tissue in the liver. [65] Most experts agree that walking for 20 minutes 5-7 days a week can stabilize liver disease.
Pharmacologic therapy
A number of studies have been initiated to evaluate the therapeutic roles of lipid-lowering agents and insulin sensitizers in the management of fatty liver. Specifically, thiazolidinediones (eg, pioglitazone and rosiglitazone), metformin, gemfibrozil, and atorvastatin have all been found to yield laboratory and histologic improvement in small uncontrolled trials. [66, 67, 68]
Thiazolidinediones have been shown to decrease inflammation in the liver in both humans and rats, with the effects lasting only as long as the medication is being delivered. [69, 70] This class of medication results in improved insulin sensitivity and universal weight gain (which has been shown to involve an increase in whole-body fat rather than total-body water). [71]
A randomized placebo-controlled trial comparing pioglitazone plus diet with diet alone in 55 patients undergoing liver biopsy reported improvements in the transaminase levels and steatosis; however, the fibrosis score improved only within the pioglitazone group before, not after, the 6-month treatment. [72] The posttreatment differences between the pioglitazone group and the placebo group were not statistically significant. Larger, longer studies are warranted.
In a study published in 2010, nearly 250 patients with NASH were divided into three groups as follows [73] :
-
Group 1, pioglitazone 30 mg/day
-
Group 2, vitamin E 800 IU/day
-
Group 3, placebo
After 96 weeks, each patient underwent a follow-up liver biopsy. Group 2 patients showed the most improvement on their liver biopsies. Both group 1 and group 2 patients showed improvements in liver lab test results and fatty liver inflammation numbers. However, group 1 patients gained the most weight and did not improve their liver scar readings. [73]
Rosiglitazone is an antidiabetic agent (thiazolidinedione derivative) that improves glycemic control by improving insulin sensitivity. It is sold both as a single-ingredient product under the brand name Avandia and as combination products under the brand names Avandamet (rosiglitazone with metformin) and Avandaryl (rosiglitazone with glimepiride).
Rosiglitazone was studied for 48 weeks in 30 patients with NASH and was found to yield biochemical as well as histologic improvement. [74] In a randomized, open-label trial, rosiglitazone plus metformin was compared with rosiglitazone plus losartan and with rosiglitazone alone after 48 weeks of therapy in 137 subjects with biopsy-proven NASH; the combination regimens yielded no greater benefit than rosiglitazone alone with respect to histopathology. [75]
The 2007 publication of a meta-analysis raised concerns among patients and healthcare professionals that rosiglitazone was potentially associated with an increased risk of myocardial infarction (MI) and heart-related deaths. [76] A 2010 update of this meta-analysis concluded that the totality of the randomized clinical trials continued to demonstrate increased risk for MI (though not for cardiovascular or all-cause mortality) and that the available findings suggested an unfavorable benefit-to-risk ratio for rosiglitazone. [77]
As of November 18, 2011, the US Food and Drug Administration (FDA) requires that healthcare providers must enroll in the Avandia-Rosiglitazone Medicines Access Program if they wish to prescribe rosiglitazone medicines to outpatients or patients in long-term care facilities. (See Safety Alert on Avandia [last updated 11/4/2011]).
Patients currently taking rosiglitazone and benefiting from the drug may continue if they choose to do so. Rosiglitazone is available to new patients only if they are unable to achieve glucose control on other medications and are unable to take pioglitazone, the only other thiazolidinedione.
The published studies to date on metformin do not include histologic data but do show short-term radiologic and biochemical improvement. [66, 67, 78, 79, 80]
Atorvastatin was studied for 1 year with repeat biopsies and was shown to yield improvement with respect to ballooning degeneration and inflammation. The drug was combined with vitamin C 1 g and vitamin E 100 IU and compared with placebo in a study lasting longer than 3 years. [58] This study used computed tomography (CT) scan measurements to diagnose liver disease and demonstrated that the odds of developing fatty liver were 34% with treatment and 70% without treatment. [58]
Gemfibrozil has resulted in biochemical improvement, but histologic data are lacking. Ezetimibe was studied in a Japanese population in conjunction with lifestyle changes and yielded improved results on follow-up liver biopsy in 6 of 10 patients after only 6 months. [81]
Pentoxifylline has received much attention in both animal models and human trials, but published results have been conflicting. [82, 83, 84, 85] Orlistat has led to histologic and biochemical improvement in patients who used the drug for several months. [86]
Vitamin E and ursodeoxycholic acid (ursodiol) have brought about improvements in specific populations. Data on the latter are conflicting in both adults and children: Some studies show biochemical and histologic improvement, whereas others studies show no difference from placebo.
Folic acid supplementation does not appear to alleviate biopsy-proven NASH. [87] Angiotensin-receptor blockers have been studied in rat models, with nonuniform results. [88, 89]
Experimental therapy
Research data suggest a possible link between obstructive sleep apnea and NAFLD/NASH. Studies have been initiated to determine whether treatment of obstructive sleep apnea results in alleviation of fatty liver disease. [90, 91, 92] The use of N-acetylcysteine [93] and cannabinoid blockers is also being explored in animal studies. [94, 95]
Bariatric surgery
There is evidence to indicate that bariatric surgery with appropriate weight loss results in both biochemical improvement and histologic improvement of NASH. [96] Roux-en-Y gastric bypass with repeat biopsy within 2 years has yielded improvement in 100% of patients. One study showed that 94% of repeat liver biopsies no longer met the pathologic criteria for NAFLD or NASH; another, in which repeat liver biopsies were done only in patients with NASH (not NAFLD), demonstrated that 89% no longer had NASH. [97, 98, 99, 100]
Early studies reporting possible worsening of hepatic function after rapid weight loss have not been substantiated. Thus, bariatric surgery may be a viable alternative in appropriate candidates.
Long-term monitoring
All patients with chronic liver disease should be tested for hepatitis A total antibodies and vaccinated if necessary. Physicians should also consider testing for hepatitis B surface antibody and vaccinating in the appropriate clinical situations (ie, life expectancy >20 years).
All patients with chronic liver disease are at risk for liver disease progression.
Patients should be educated to avoid alcohol and other hepatotoxic substances. If patients have a liver insult from another liver problem, they may have longer recovery times than patients without fatty liver disease would.
Patients with fatty liver disease should be seen regularly by a primary care physician, who may be able to detect disease progression through physical examination findings (eg, spider telangiectasia, palmar erythema, or splenomegaly), laboratory findings (eg, decreasing platelets, elevated bilirubin, or decreasing albumin), patient complaints (eg, encephalopathy, ascites, or fatigue), or incidental imaging study findings (eg, cirrhotic liver, splenomegaly, varices, or ascites).
Provide follow-up care for patients in an outpatient facility. In patients with alcoholic steatosis, determination of blood alcohol at every outpatient visit often is helpful in determining patient’s compliance with abstinence.
Patients who have NASH cirrhosis should be screened for gastroesophageal varices as well as hepatocellular carcinoma.
Questions & Answers
Overview
What are pathologic changes observed in patients with alcoholic liver disease (ALD)?
What is the pathogenesis of fatty liver disease?
What is the role of metabolic syndrome in the etiology of fatty liver disease?
Which factors increase the risk for fatty liver disease?
Which factors increase the risk for advanced alcoholic liver disease (ALD)?
What is the prevalence of fatty liver disease in the US?
What is the global prevalence of fatty liver disease?
How does the prevalence of fatty liver disease vary by age?
How does the prevalence of fatty liver disease vary by sex?
What is the racial predilection of fatty liver disease?
What is the prognosis of fatty liver disease?
What are complications of fatty liver disease?
What is included in the patient education about fatty liver disease?
Which organizations provide resources and support for patients with fatty liver disease?
Which clinical history findings are characteristic of fatty liver disease?
What is the focus of clinical history in the evaluation of fatty liver disease?
What are symptoms of fatty liver disease?
Which physical findings are characteristic of fatty liver disease?
What is included in the differential diagnoses for fatty liver disease?
When is steatosis observed in fatty liver disease?
What are AASLD/ACG/AGA guidelines for the workup of nonalcoholic fatty liver disease (NAFLD)?
What is the role of insulin and glucose testing in the diagnosis of fatty liver disease?
What is the role of glutamyl transpeptidase (GGT) testing in the diagnosis of fatty liver disease?
How prevalent is cholestasis in fatty liver disease?
How prevalent is macrocytosis in fatty liver disease?
What is the role of triglycerides in the diagnosis of fatty liver disease?
What is the role of alkaline phosphatase (ALP) measurement in the diagnosis of fatty liver disease?
What is the role of aminotransferases in the diagnosis of fatty liver disease?
Which lab findings suggest nonalcoholic fatty liver disease (NAFLD)?
What is the role of imaging studies in the diagnosis of fatty liver disease?
What is the nonalcoholic fatty liver disease (NAFLD) fibrosis score?
What are independent predictors of nonalcoholic fatty liver disease (NAFLD)?
What is the role of liver biopsy and histopathologic exam in the diagnosis of fatty liver disease?
Which histologic findings indicate fatty liver disease?
What are the treatment options for fatty liver disease?
What is the role of alcohol abstinence in the treatment of fatty liver disease?
What is the role of diet and weight loss in the treatment of alcoholic liver disease (ALD)?
How is nonalcoholic fatty liver disease (NAFLD) prevented?
Treatment of which underlying diseases may reverse fatty liver disease?
What is the role of exercise in the treatment of fatty liver disease?
What is the role of drug treatment for fatty liver disease?
What is the role of pioglitazone in the treatment of fatty liver disease?
What is the role of rosiglitazone in the treatment of fatty liver disease?
What is the role of metformin in the treatment of fatty liver disease?
What is the role of atorvastatin in the treatment of fatty liver disease?
What is the role of gemfibrozil and ezetimibe in the treatment of fatty liver disease?
What is the role of pentoxifylline in the treatment of fatty liver disease?
What is the role of vitamin supplements in the treatment of fatty liver disease?
Which therapies are under investigation for the treatment of fatty liver disease?
What is the role of bariatric surgery in the treatment of fatty liver disease?
What is included in the long-term monitoring of patients with fatty liver disease?
-
Liver steatosis
-
Ballooning degeneration
-
Periportal hepatosteatosis
-
Mechanisms of cytokine injury. IL = interleukin ; NO = nitric oxide; O2- = superoxide anion; OH- = hydroxyl radical; PMN = polymorphonuclear lymphocyte; TNF = tumor necrosis factor.
Tables
What would you like to print?
- Overview
- Etiology
- Epidemiology
- Prognosis
- Patient Education
- Presentation
- Differential Diagnosis
- AASLD/ACG/AGA Guidelines for Workup of NAFLD
- Laboratory Studies
- Ultrasonography, CT Scanning, and MRI
- Predictive Measures
- Liver Biopsy and Histopathologic Examination
- Treatment
- Questions & Answers
- Show All
- Media Gallery
- References