Practice Essentials
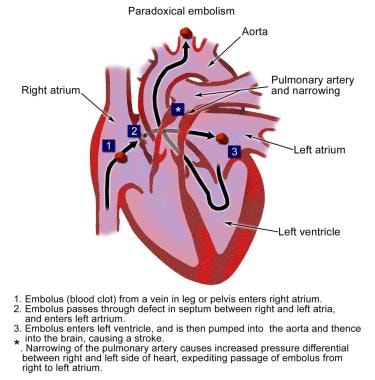
The clinical manifestations of paradoxical embolism (PDE) are nonspecific, making the diagnosis difficult to establish. Patients with PDE may present with signs and symptoms of systemic embolization affecting multiple organs (eg, brain, heart, visceral organs, and peripheral vasculature). The disease starts with the formation of emboli within the venous system, which enter the systemic circulation after traversing a right-to-left shunt such as a patent foramen ovale (PFO), atrial septal defect (ASD), or pulmonary arteriovenous malformation (AVM). [1, 2, 3, 4]
PDE typically originates in the veins of the lower extremities and occasionally in the pelvic veins. Emboli may be of various types, such as clots, air, tumor, fat, and amniotic fluid. [5] Septic emboli have led to brain abscesses.
PDE is considered the major cause of cerebrovascular accidents (CVAs) in young patients. On rare occasions, it may occlude the pelvic aortic bifurcation. One of the largest documented thromboses discovered in a PFO (impending PDE) was 25 cm long. [6]
PDE is typically discovered in the workup of patients presenting with stroke, myocardial infarction (MI), mesenteric ischemia, or acute limb ischemia when there also is a clinical suspicion for embolism as opposed to thrombosis.
Previously, a definitive diagnosis of PDE required the presence of a thrombus within an intracardiac defect at autopsy. [7] However, the current diagnostic approach relies on the presence of an arterial embolism with concomitant deep venous thrombosis (DVT) with or without pulmonary embolism (PE), right-to-left shunting through an intracardiac (commonly the PFO) or interpulmonary communication, and a favorable right-to-left pressure gradient. [8, 9, 10] Typically, more common arterial or cardiac sources for embolization (eg, aortic aneurysm and atrial thrombus) are absent.
Available therapies for PDE include medical treatment, percutaneous endovascular intervention, and surgery. [11] Anticoagulation is the mainstay of therapy, with concomitant closure of the intracardiac shunt by means of endovascular or open surgical interventions. [11]
The presence of PDE in association with PE or atrial clots is associated with increased mortality. In the most common case of PDE with PFO, there is mixed evidence regarding treatment with medical therapy alone versus a combination of medical therapy and PFO closure. Outcomes following three randomized control trials suggested a benefit to percutaneous PFO closure over medical treatment alone; however, a meta-analysis demonstrated differences in patient outcomes depending on the device used for PFO closure. [1]
Pathophysiology
PDE originates from a venous thrombosis (see the image below). In most cases, the source is in the deep veins of the lower extremities; thrombosis occurs less frequently in the upper extremities than in the lower extremities. The thrombus is composed of platelets, fibrin, and, eventually, red blood cells (RBCs). It tends to propagate in the direction of the blood flow.
The intracardiac communication between the venous and arterial circulations can be in the form of a PFO, an ASD, a pulmonary AVM, a ventricular septal defect (VSD), an Ebstein anomaly, or a patent ductus arteriosus (PDA).
A PFO is defined as a valvelike opening between the septum primum and the septum secundum without evidence of an anatomic septal defect. PFO is significant in the etiology of PDE if associated right-to-left shunting is present. Causes of right-to-left shunting include the following:
-
Right atrial hypertension
-
Right ventricular hypertension
-
Right ventricular failure with increased end-diastolic pressure; positive-pressure ventilation
-
Positive end-expiratory pressure
-
Pulmonary hypertension from hypoxemia
-
MI of the right side of the heart
-
Valsalva-type maneuvers (forced expiration against a closed glottis), including urination, defecation, and sneezing
The clinical manifestations are based on complications of embolism and depend on the site of the embolus; multiorgan ischemia and infarction can occur. Rarely, cases of PDE have been reviewed without pathologic evidence of PE. [4] PE increases the pressure in the right chambers of the heart, promoting right-to-left shunting of blood emboli. If the left pulmonary artery is occluded suddenly, the mean pulmonary artery pressure (PAP) increases by 30% from the baseline. According to estimates, PE may lead to PDE only if it produces a rise in mean PAP greater than 30 mm Hg, facilitating an increase in right atrial pressure (RAP) above left atrial pressure (LAP) that results in right-to-left shunting.
The PFO (most common intracardiac communication) increases in size with advancing age, from a mean of 3 mm in the first decade to 6 mm in the 10th decade.
Etiology
The etiology of PDE is related to factors promoting venous thrombosis and right-to-left shunting. Thus, many conditions predispose individuals to increased risk for DVT, including the following:
-
Hypercoagulable states, such as factor V Leiden (resistance to activated protein C); antithrombin III, protein C, and protein S deficiencies; antiphospholipid antibody syndrome; prothrombin mutation; and dysfibrinogenemia
-
Previous DVT
-
Immobilization
-
Pregnancy and estrogen use
-
Cancer
-
Abdominal and thoracic surgical procedures
-
Orthopedic and genitourinary surgical procedures
-
Trauma
Intracardiac communication of the venous and arterial circulations can lead to PDE and may occur via the following:
-
PFO
-
ASD
-
Pulmonary AVM
-
VSD
-
Ebstein anomaly
-
PDA
It has been suggested that cardiopulmonary resuscitation (CPR) could cause PDE by producing a sudden increase in RAP during the compression phase and thereby giving rise to a right-to-left shunt. [12]
Epidemiology
United States statistics
The actual frequency of PDE has not been definitively established, because most cases are presumed rather than proved and most cryptogenic strokes are not investigated.
PDE may be common. The incidence of first or new strokes in the United States is approximately 610,000 per year. [13] Of all strokes, as many as 40% are cryptogenic (ie, lack an identifiable source). [14, 15] PFOs contribute to the pathophysiology of approximately 20-30% of these cryptogenic strokes; however, they have been reported in as many as 56% of patients younger than 55 years who have cryptogenic strokes. [15]
Autopsy data suggest that PFO may be present in 25-30% of the normal population. Right-to-left atrial shunts in PDE are associated with an underlying PFO in approximately 70% of case series and autopsy reports. May-Thurner syndrome, typically involving compression of the left common iliac vein by the right common iliac artery, can generate stenosis, stasis, and occult thrombosis as a source of PDE. In a systematic review of the literature on May-Thurner syndrome, 2.2% of cases presented with paradoxical strokes. [16]
DVT may be subclinical in more than 50% of cases. Venous thrombosis may occur in more than 50% of orthopedic surgical procedures and more than 20% of patients undergoing abdominal or thoracic surgical procedures.
The clinical findings of PDE are arterial embolic manifestations that include cerebral (40%), peripheral (50%), coronary (8%), renal (1%), and splenic (1%) ischemia or infarction. Reported rates of PE have been as high as 85% in patients diagnosed with PDE. Chronic elevation of right-side heart pressures has been associated with 5% of PDE cases. [8]
Age-, sex-, and race-related demographics
Elderly patients are commonly affected; PDE is not common in children. The risk of DVT is increased in the elderly population; this is correlated with the increased incidence of PDE in patients older than 55 years. Elderly patients may be at increased risk for the passage of thrombus through a PFO. The size of the PFO is usually greater in this age group than in younger populations; the average size of a PFO is 3 mm in the first decade of life versus 6 mm in the 10th decade of life.
However, PDE can still occur in younger adults (ie, < 55 y) when an intracardiac communication is present with right-to-left atrial shunting and risk of DVT. For example, in young patients with cryptogenic stroke, PFO is found more frequently than it is discovered in the general population (~25%). [17] PFO with atrial right-to-left shunting is the most frequent cardiac finding in patients younger than 55 years with an otherwise unexplained ischemic cerebral insult or cryptogenic stroke.
No significant differences between the sexes or among various racial and ethnic groups have been identified in patients with PDE.
Prognosis
PDE generally has a good prognosis when it is not complicated. Morbidity and mortality are increased in patients with PDE and PE, depending on the size of the embolus and end-organ lodgment. When impending PDE occurs and the thrombus is lodged in connection between arterial and venous systems (usually PFO or ASD), mortality estimates of 18.4% at 30 days have been reported. [18] Treatment options for impending PDE include open-heart surgery for thromboembolectomy and closure of PFO, thrombolysis, and anticoagulation.
Some patients with PDE experience devastating outcomes with complications such as neurologic deficits, blindness, permanent cardiac damage, gangrene of extremities, limb amputation, and mesenteric ischemia, depending on the location of the emboli. Other possible organ damage may include renal infarction with eventual acute renal failure (acute kidney injury [AKI]), or splenic infarct. [4]
Patient Education
Patients on long-term anticoagulant therapy should be educated in the importance of compliance with their medication regimen for prevention of recurrent thromboembolic events. They should also be instructed to avoid vitamin K–containing foods such as green leafy vegetables (eg, spinach, broccoli, and cauliflower).
To prevent elevation of RAP above LAP, which can lead to transient right-to-left shunting in patients with symptomatic PDE and persistent open shunts, Valsalva maneuvers should be avoided.
For patient education resources, see the Circulatory Problems Center, as well as Blood Clot in the Legs.
-
Paradoxical embolism.