Practice Essentials
Cholesterol embolism is a type of embolism resulting from fracture of an atherosclerotic plaque. [1] Cholesterol embolism (embolization) syndrome (CES) should be suspected in a patient who develops worsening renal function, [2] hypertension, distal ischemia, or acute multisystem dysfunction after an invasive arterial procedure. Atheroemboli may also occur spontaneously.
Key components of CES include proximal large-caliber arterial plaque, plaque rupture with embolization of debris, mechanical occlusion of small arteries, intense foreign-body inflammation, end-organ damage from mechanical obstruction, and inflammatory vascular changes. The protean manifestations of this syndrome make the diagnosis challenging.
Any risk factor for atherosclerotic disease is a risk factor for cholesterol embolism.
Cholesterol embolism is a disease of persons ranging from middle-aged to elderly (minimum age, 50 y). Men are at higher risk than women are. As the population ages, the incidence of this syndrome will increase.
Medical management of CES is supportive. Pharmacologic therapy has not been particularly successful. Surgical therapy (eg, aortic aneurysm resection) may be necessary to remove the source of atheroembolic material. Stent-grafting may be a less invasive method to reduce embolization risk.
Pathophysiology
Key components of CES include the following:
-
Proximal large-caliber arterial plaque
-
Plaque rupture with embolization of debris
-
Mechanical occlusion of small arteries
-
Intense foreign-body inflammation
-
End-organ damage from mechanical obstruction
-
Inflammatory vascular changes
Any organ system, with the exception of the lungs, may be directly affected. CES has two mechanisms of action.
With the first mechanism, cholesterol crystals spontaneously break off from severely atherosclerotic plaques and shower into downstream organs, occluding arterioles 100-200 μm in diameter. The crystals induce an inflammatory foreign-body reaction and adventitial fibrosis, which eventually obliterate the vessel lumen. Local vasospastic mediators compound tissue ischemia and produce progressive, irreversible organ damage.
With the second mechanism, larger cholesterol plaques break off and occlude larger arteries, causing tissue infarction with acute organ dysfunction. This can occur after local trauma to the atherosclerotic plaque (eg, from angiography or aortic trauma), or it can occur after destabilization of the protective clot overlying the plaque (eg, as a result of anticoagulation).
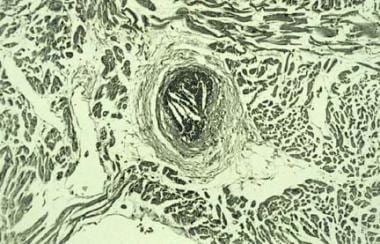
Cholesterol crystal embolization (see the image below) occurs from the arterial system, and crystals are trapped in the arterioles, where they either immediately occlude the vessels or induce an intense inflammatory response that leads to tissue ischemia. Crystals do not travel to the lungs; however, inflammatory mediators released by ischemic tissue may result in acute lung injury.
Etiology
Any risk factor for atherosclerotic disease is a risk factor for cholesterol embolism.
Preoperative risk factors for CES after coronary artery bypass grafting (CABG) include the following:
-
Age greater than 60 years
-
Cerebrovascular disease
-
Mitral anular calcification
Although the other factors have been well known for some time, it was only comparatively recently that the association between mitral anular calcification and aortic atherosclerosis was identified.
Identifying patients at risk and making efforts to minimize aortic-wall trauma help reduce the chance of cholesterol embolism. The risk that cholesterol embolism will develop may be reduced by taking a brachial or axillary approach in patients known to have severely ulcerated aortic plaque, using soft flexible catheters, and avoiding high-pressure jets of contrast material.
A study by Takahashi et al found that a patient age of 70 years or greater, the presence of an aortic aneurysm (23% vs 7.2% p < 0.001), and a femoral approach were all positive predictors of cholesterol crystal embolism after percutaneous coronary intervention (PCI), whereas the use of an inner sheath and a nonfemoral approach were associated with a lower incidence of this condition. [3] Ischemic stroke as a manifestation of CES following PCI has been reported. [4]
Epidemiology
International statistics
Estimates of the incidence of cholesterol embolic disease are usually based on autopsy data. Tissue sections from patients with the following diseases or procedures indicate the incidence of atheroembolic events:
-
Aortic aneurysms (31%)
-
Abdominal aortic aneurysm repair (up to 77%)
-
Severe aortic disease (13-16%)
-
Mild aortic disease (1-2%)
Of patients undergoing angiography, 25-30% may have atheroembolic events, whereas 2.5-3% of patients undergoing percutaneous transluminal coronary angioplasty (PTCA) vein grafts and 1.4-3% of patients undergoing renal artery angioplasty or cardiac catheterization have been reported to have clinical signs of atheroemboli. CES has been reported as occurring months after thrombolytic therapy for stroke, but the true incidence is unknown. [5, 6]
Age- and sex-related demographics
Cholesterol embolism is a disease of persons ranging from middle-aged to elderly, with a minimum age of 50 years. The risk is greater for men than it is for women.
Prognosis
Patients with multisystem CES have a poor prognosis. The mortality of acute multisystem organ failure resulting from CES is 58-90%. Jucgla et al found an overall incidence of 58% at 15 months, which increased to 65% if visceral organs were involved. [7] Preexisting chronic renal insufficiency had a relative risk of death of 4.54.
The mortality of severe cholesterol embolism is 90% at 3 months. Mild cases with renal dysfunction, with or without skin findings, have a mortality of 16%.
Cholesterol crystal showers can become stabilized, leaving patients with varying degrees of organ dysfunction. Renal function can recover if no further insults occur, even to the point where dialysis can be discontinued. However, patients remain at risk for recurrence of emboli.
Patient Education
Patients should be educated to watch for ulcerations and infections in chronically ischemic areas, particularly feet and toes. Ischemic neuropathy may exacerbate injury and tissue loss, predisposing the patient to gangrene.
For patient education resources, see the Cholesterol Center, as well as High Cholesterol, Cholesterol Charts (What the Numbers Mean), Lifestyle Cholesterol Management, and Cholesterol Lowering Medications.
-
Cholesterol crystal embolization from upstream coronary artery plaque after percutaneous transluminal coronary angioplasty.
-
Necrosis of the abdominal wall in a patient with cholesterol embolism syndrome who received anticoagulation.