Background
Electrical alternans is a broad term that describes alternate-beat variation in the direction, amplitude, and duration of any component of the electrocardiograph (ECG) waveform (ie, P, PR, QRS, R-R, ST, T, U). It was first recognized over a century ago by Theodor Herring in 1909, [1] further characterized by Sir Thomas Lewis in 1910, [2] and subsequently identified on surface ECG in 1948 decades later by Kalter and Schwartz. [3]
Electrical alternans is not a distinct entity in itself, but rather an ECG sign of an underlying cardiac pathology. The component of the ECG displaying alternans may provide a clue in this regard. For example, electrical alternans related to the T wave (ie, T wave alternans) has shown its potential value in cardiac risk stratification and prediction of sudden cardiac death.
Electrical alternans must be distinguished from mechanical alternans (eg, pulsus alternans), although both may coexist.
Pathophysiology
The pathophysiologic mechanisms that cause electrical alternans can be divided into three main categories:
Alternans due to cardiac motion
Alternans due to cardiac motion is the most well-known mechanism of electrical alternans, encountered in large pericardial effusions and cardiac tamponade. The pendulous swinging motion of the heart in a fluid-suspended cavity in such situations effectively causes electrical alternans. [4] This motion with respect to the fixed overlying surface electrode [5, 6, 7, 8] results in total electrical alternans involving all portions of the electrocardiogram. Rarely, this phenomenon may be witnessed in hypertrophic cardiomyopathy as well.
Conduction alternans (P, PR, QRS)
Conduction via distinct alternate pathways with differing conduction and recovery characteristics can lead to the development of altering cycle lengths and can thus give rise to alternans. This is most classically seen in atrioventricular reentrant tachycardia (AVRT). It was once thought that the presence of electrical alternans recorded on ECG during supraventricular tachycardia (SVT) suggested AVRT rather than other forms of SVTs. However, it became evident that electrical alternans during SVTs was more likely a function of the heart rate rather than the mechanism of arrhythmia. [9] The rate of tachycardia remains the most important determinant of QRS alternans [10, 11] ; it may be encountered in a number of cardiac conditions associated with high rates of conduction, including atrial fibrillation, Wolff-Parkinson-White Syndrome, ventricular tachycardia, SVT, and accelerated idioventricular rhythm. [4]
Conditions such as cardiomyopathies or heart failure are associated with structural alterations of the cardiac tissue as well as generation of pathways with altered conduction characteristics.
Repolarization alternans (ST, T, U)
A number of cardiac conditions (eg, ischemia, heart failure) can exaggerate the inherent heterogeneity of the myocardial repolarization characteristics, [12, 13] serving as a substrate for ventricular arrhythmias and sudden cardiac death. This heterogeneity manifests as T-wave alternans, which is increasingly being utilized for risk stratification of sudden cardiac death (see the discussion in the Workup section under Other tests).
Alterations in calcium-handling dynamics in certain regions of the myocardium lead to changes in the repolarization characteristics of these areas, manifesting as electrical alternans. This occurs through direct effects on calcium conduction during the plateau phase of the action potential, and also through effects on calcium-sensitive sodium channels. [14, 15, 16, 17, 18, 19, 20, 21] Cardiomyopathies, heart failure, and certain arrhythmias are associated with changing cycle lengths, which result in changing stroke volumes on a beat-to-beat basis. Consequently, the constantly changing mechanical stretch of the chamber walls affects the conduction of stretch-sensitive ion channels—a phenomenon known as mechanoelectric feedback (MEF). [22, 23] Cardiac memory of the preceding cycle lengths, a property known as hysteresis, plays a role in perpetuating alternans even after normalization of the heart rate. [19]
Etiology
The reported causes or associations of electrical alternans have been mentioned already and are relisted here for convenience.
Alternans due to cardiac motion
Causes include the following:
-
Large pericardial effusion /cardiac tamponade
-
Hypertrophic cardiomyopathy
-
Emphysema / pneumothorax
-
Large bilateral pleural effusions
Repolarization alternans (ST, U, T)
ST alternans
-
Myocardial ischemia
-
Vasospastic angina pectoris
-
Acute myocardial infarction
T-wave alternans
-
Congenital long QT syndromes
-
Cardiomyopathies
-
Treatment with quinidine or amiodarone [15]
-
Dyselectrolytemia (hypokalemia, hypomagnesemia, hypocalcemia)
-
Following cardiac resuscitation
Conduction alternans (P, PR, QRS)
Note the following causes:
-
Left ventricular dysfunction
-
Myocardial contusion
-
Acute pulmonary embolism
-
Ventricular tachycardia
Epidemiology
United States data
Electrical alternans is estimated to be encountered in about 1 to 6 of 10,000 electrocardiograms (ECGs). Overall, QRS alternans is the most commonly reported, although it is only seen in 5%-10% of patients with tamponade. The incidence of ST alternans has been reported to be 5%-7.7% of patients during coronary intervention. T-wave alternans is observed in about 45% of patients with congenital long QT syndrome during Holter monitoring.
Prognosis
The finding of electrical alternans during supraventricular tachycardia does not in itself change the prognosis; however, some forms of electrical alternans have prognostic value. For example, obvious “macro-T wave” alternans indicates impending ventricular tachycardia and fibrillation leading to cardiac arrest (see the following image).
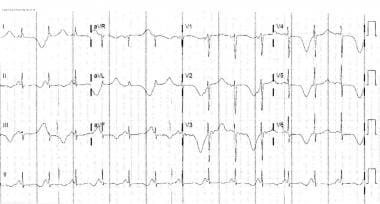 Electrical alternans. This electrocardiogram reveals macro-T wave alternans with switched polarity seen in all leads.
Electrical alternans. This electrocardiogram reveals macro-T wave alternans with switched polarity seen in all leads.
Similarly, electrical alternans seen during ventricular tachycardia is associated with significant hemodynamic instability (see the image below).
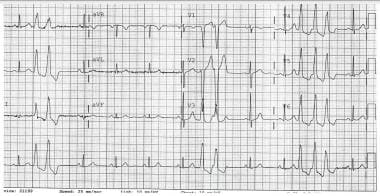 Electrical alternans. This electrocardiogram shows ventricular tachycardia from the right ventricular outflow tract (RVOT) region. Note the R wave alternans seen in the wide QRS complexes.
Electrical alternans. This electrocardiogram shows ventricular tachycardia from the right ventricular outflow tract (RVOT) region. Note the R wave alternans seen in the wide QRS complexes.
The presence of micro-T wave alternans may indicate a higher risk of sudden cardiac death and spontaneous ventricular arrhythmias. However, its greatest utility lies in its high negative predictive value (NPV) for future arrhythmias (>90% NPV for 1 year). [25]
Morbidity/mortality
Morbidity or mortality in the setting of electrical alternans is wholly related to the underlying cardiac pathology. T-wave alternans has been associated with higher risk of developing ventricular arrhythmias as well as sudden cardiac death.
Complications
Electrical alternans is frequently associated with serious underlying cardiac conditions. All complications are related to the underlying disease process.
-
Electrical alternans. This electrocardiogram shows a typical alternate-beat QRS electrical alternans. Note that the QRS voltage is low.
-
Electrical alternans. This electrocardiogram reveals supraventricular tachycardia with alternans. Note the phasic nature to the QRS morphology, particularly in the rhythm strip in V1.
-
Electrical alternans. This electrocardiogram reveals macro-T wave alternans with switched polarity seen in all leads.
-
Electrical alternans. This electrocardiogram shows ventricular tachycardia from the right ventricular outflow tract (RVOT) region. Note the R wave alternans seen in the wide QRS complexes.







