Practice Essentials
Ebola virus is one of at least 30 known viruses capable of causing viral hemorrhagic fever syndrome. The genus Ebolavirus currently is classified into 5 separate species: Sudan ebolavirus, Zaire ebolavirus, Tai Forest (Ivory Coast) ebolavirus, Reston ebolavirus, and Bundibugyo ebolavirus. [1] The outbreak of Ebola virus disease in West Africa from 2014 to 2016, involving Zaire ebolavirus, was the largest outbreak of Ebola virus disease in history.
As of September 17, 2019, an active outbreak of Ebola virus disease in the Democratic Republic of the Congo (DRC) had resulted in 3,034 confirmed and 111 probable cases of Ebola virus disease, including 2,103 attributable deaths. [2, 3] An experimental vaccine has been credited with limiting the outbreak’s scope. [4]
Signs and symptoms
The following 2 types of exposure history are recognized:
-
Primary exposure – This typically involves travel to or work in an Ebola-endemic area.
-
Secondary exposure – This refers to human-to-human exposure (eg, medical caregivers, family caregivers, or persons who prepared deceased patients for burial), primate-to-human exposure (eg, animal care workers who provide care for primates), or persons who collect or prepare bush meat for human consumption.
Physical findings depend on the stage of disease at the time of presentation. With African-derived Ebolavirus infection, there is an incubation period (typically 3-8 days in primary cases and slightly longer in secondary cases).
Early findings may include the following [5] :
-
Fever
-
Pharyngitis
-
Severe constitutional signs and symptoms
-
Maculopapular rash (best seen in White patients)
-
Bilateral conjunctival injection
Later findings may include the following [5] :
-
Expressionless facies
-
Bleeding from intravenous (IV) puncture sites and mucous membranes
-
Myocarditis and pulmonary edema
-
In terminally ill patients, tachypnea, hypotension, anuria, and coma
Survivors of Ebola virus disease have developed the following late manifestations [5] :
-
Myalgias
-
Asymmetric and migratory arthralgias
-
Headache
-
Fatigue
-
Bulimia
-
Amenorrhea
-
Hearing loss
-
Tinnitus
-
Unilateral orchitis
-
Suppurative parotitis
Diagnosis
Diagnostic studies that may be helpful include the following:
-
Basic blood tests – Complete blood count (CBC) with differential, bilirubin, liver enzymes, blood urea nitrogen (BUN), creatinine, pH
-
Studies for isolating the virus – Tissue culture (only to be performed in one of a few high-containment laboratories throughout the world), reverse-transcription polymerase chain reaction (RT-PCR) assay
-
Serologic testing – Enzyme-linked immunosorbent assay (ELISA) for antigens or for immunoglobulin M (IgM) and immunoglobulin G (IgG) antibodies
-
Other studies – Immunochemical testing of postmortem skin, electron microscopy
Management
General principles of care are as follows:
-
Supportive therapy with attention to intravascular volume, electrolytes, nutrition, and comfort care is of benefit to the patient.
-
Such therapy must be administered with strict attention to barrier isolation; all body fluids contain infectious virions and should be handled with great care.
-
No specific therapy is available that has demonstrated efficacy in the treatment of Ebola hemorrhagic fever.
-
Ebola Zaire vaccine is approved in Europe and the United States. The live recombinant vaccine has shown effectiveness of 97.5% in preventing infection among 90,000 individuals in an active Ebola virus outbreak in the Democratic Republic of Congo. [3]
-
The FDA approved atoltivimab/maftivimab/odesivimab (Inmazeb), a recombinant human monoclonal antibody combination. These antibodies target the glycoprotein (GP) on the Ebola virus surface, thereby blocking attachment and entry of the virus on host cell membranes. [6]
Other agents that have been studied for the treatment or prevention of Ebola virus disease include the following:
-
Ribavirin (possesses no demonstrable anti- Ebolavirus activity in vitro and has failed to protect Ebolavirus -infected primates)
-
Nucleoside analogue inhibitors of S-adenosylhomocysteine hydrolase (SAH)
-
Interferon beta
-
Horse- or goat-derived immune globulins
-
Human-derived convalescent immune globulin preparations
-
Recombinant human monoclonal antibodies
-
Recombinant human interferon alfa-2
-
Activated protein C [7]
-
Recombinant inhibitor of factor VIIa/tissue factor [8]
In those patients who do recover, recovery often requires months, and delays may be expected before full resumption of normal activities. Weight gain and return of strength are slow. Ebola virus continues to be present for many weeks after resolution of the clinical illness.
Background
Ebola virus is one of at least 30 known viruses capable of causing viral hemorrhagic fever syndrome. Although agents that cause viral hemorrhagic fever syndrome constitute a geographically diverse group of viruses, all of those identified to date are RNA viruses with a lipid envelope, all are considered zoonoses, all damage the microvasculature (resulting in increased vascular permeability), and all are members of 1 of the following 4 families:
-
Arenaviridae
-
Bunyaviridae
-
Flaviviridae
-
Filoviridae
Although some of the hemorrhagic fever viruses are normally spread by ticks or mosquitoes, all but one (ie, dengue hemorrhagic fever) are capable of being spread by aerosols, and this capability makes these viruses potential bioterrorism agents.
The family Filoviridae resides in the order Mononegavirales and contains the largest genome within the order. This family contains 2 genera: Ebolavirus (containing 5 species) and the antigenically distinct Marburgvirus (containing a single species).
In patients who have Ebola virus infection, exposure to the virus may be either primary (involving presence in an Ebolavirus -endemic area) or secondary (involving human-to-human or primate-to-human transmission). Physical findings depend on the stage of disease at the time of presentation.
Studies have demonstrated that patients who die of Ebola viral infection do not develop a humoral immune response. However, in survivors neutralizing antibody can be detected. It is likely that a broad humoral immune response can increase the likelihood of an infected patient surviving Ebola.
No specific therapy is available that has demonstrated efficacy in the treatment of Ebola hemorrhagic fever, and there are no commercially available Ebola virus vaccines. General medical support is critical. Care must be administered with strict attention to barrier isolation. Because the source of Ebola virus is unknown, education and prevention of primary cases is problematic. Education of communities at risk, especially healthcare workers, can greatly reduce the number of secondary person-to-person transmissions.
Pathophysiology and Etiology
Ultrastructure and pathogenesis
The known members of the family Filoviridae are the genera Ebolavirus (Ebola virus) and Marburgvirus (Marburg virus). According to the 2012 virus taxonomy of the International Committee on Taxonomy of Viruses, Ebolavirus is classified into the following 5 separate species:
Sudan ebolavirus
Zaire ebolavirus
Tai Forest ebolavirus (formerly and perhaps still more commonly Ivory Coast ebolavirus or Côte d’Ivoire ebolavirus)
Reston ebolavirus
Bundibugyo ebolavirus
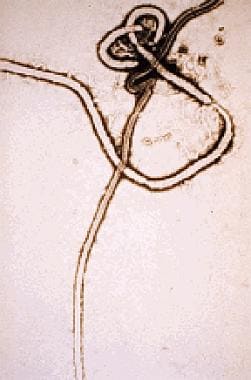
Filoviruses such as Ebola virus share a characteristic filamentous form, with a uniform diameter of approximately 80 nm but a highly variable length. [1] Filaments may be straight, but they are often folded on themselves.
Ebola virus has a nonsegmented negative-stranded RNA genome containing 7 structural and regulatory genes. The Ebola genome codes for 4 virion structural proteins (VP30, VP35, nucleoprotein, and a polymerase protein [L]) and 3 membrane-associated proteins (VP40, glycoprotein [GP], and VP24). The GP gene is positioned fourth from the 3′ end of the 7 linearly arranged genes.
After infection, human and nonhuman primates experience an early period of rapid viral multiplication that, in lethal cases, is associated with an ineffective immunologic response. Although a full understanding of Ebola virus disease must await further investigations, part of the pathogenesis has been elucidated.
Most filovirus proteins are encoded in single reading frames; the surface GP is encoded in 2 frames (open reading frame [ORF] I and ORF II). The ORF I (amino-terminal) of the gene encodes for a small (50-70 kd), soluble, nonstructural secretory glycoprotein (sGP) that is produced in large quantities early in Ebola virus infection. [9]
The sGP binds to neutrophil CD16b, a neutrophil-specific Fc g receptor III, and inhibits early neutrophil activation. The sGP also may be responsible for the profound lymphopenia that characterizes Ebola infection. Thus, sGP is believed to play pivotal roles in the ability of Ebola to prevent an early and effective host immune response. One hypothesis is that the lack of sGP production by Marburg virus may explain why this agent is less virulent than African-derived Ebola virus.
Leroy and colleagues reported their observations of 24 close contacts of symptomatic patients actively infected with Ebola. [10] Eleven of the 24 contacts developed evidence of asymptomatic infection associated with viral replication. Viral replication was proven by the authors’ ability to amplify positive-stranded Ebola virus RNA from the blood of the asymptomatic contacts.
A detailed study of these infected but asymptomatic individuals revealed that they had an early (4-6 days after infection) and vigorous immunologic response with production of interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF), resulting in enhanced cell-mediated and humoral-mediated immunity. In patients who eventually died, proinflammatory cytokines were not detected even after 2 to 3 days of symptomatic infection.
A second, somewhat larger (120-150 kd) GP, transmembrane glycoprotein, is incorporated into the Ebola virion and binds to endothelial cells but not to neutrophils. Ebola virus is known to invade, replicate in, and destroy endothelial cells. Destruction of endothelial surfaces is associated with disseminated intravascular coagulation, and this may contribute to the hemorrhagic manifestations that characterize many, but not all, Ebola infections.
Clinical infection in human and nonhuman primates is associated with rapid and extensive viral replication in all tissues. Viral replication is accompanied by widespread and severe focal necrosis. The most severe necrosis occurs in the liver, and this is associated with the formation of Councilman-like bodies similar to those seen in yellow fever. In fatal infections, the host’s tissues and blood contain large numbers of Ebola virions, and the tissues and body fluids are highly infectious.
The 5 Ebolavirus species were named for the locations where they caused documented human or animal disease. Two African species, Sudan ebolavirus and Zaire ebolavirus, have been responsible for most of the reported deaths. Clinical disease due to African-derived Ebola virus is severe and, with the exception of a patient who survived infection with a third African species, Ivory Coast ebolavirus, is associated with a mortality ranging from 65% (Sudan, 1979) to 89% (Democratic Republic of the Congo [DRC], December 2002-April 2003).
A fourth Ebolavirus species, Reston ebolavirus, was first isolated in 1989 in monkeys imported from a single Philippine exporter. A virtually identical isolate imported from the same Philippine exporter was detected in 1992 in Siena, Italy. To date, this species has not been documented to cause human disease.
The fifth Ebolavirus species, also of African lineage, is Bundibugyo ebolavirus, which caused an outbreak in Uganda in 2007 to 2008, with a mortality of 25%. [11]
Between 1994 and 1997, a stable strain of Ebola virus caused 3 successive outbreaks of hemorrhagic fever in Gabon (mortality, 60%-74%). [12] Because the Gabon strain shares a greater than 99% homology of the nucleoprotein and GP gene regions with Zaire ebolavirus, it has not been considered a distinct species.
A likely reservoir for filoviruses has been identified. In 1996, members of the National Institute for Virology of South Africa went to Kikwit, DRC, and evaluated the infectivity of Ebola virus for 24 species of plants and 19 species of vertebrates and invertebrates. [13] Insectivorous bats and fruit bats were found to support Ebola virus replication without dying. Furthermore, serum Ebola titers in infected fruit bats reached as high as 106 fluorescent focus-forming units/mL, and feces contained viable Ebola virus.
Mechanisms of dispersion
African-derived filovirus infections are characterized by transmission from an unknown host (possibly bats) to humans or nonhuman primates, presumably via direct contact with body fluids such as saliva or blood or other infected tissues. Evidence in nonhuman primates indicates that Sudan ebolavirus and Zaire ebolavirus may be transmitted by contact with mucous membranes, conjunctiva, pharyngeal and gastrointestinal surfaces; through small breaks in the skin; and, at least experimentally, by aerosol. [14]
Dogs have been shown to acquire asymptomatic Ebola virus infections, possibly by contact with virus-laden droplets of urine, feces, or blood of unknown hosts. [15] Of epidemiologic significance was the observation that seroprevalence rates in dogs rose in a linear fashion as sampling approached areas of human cases, reaching as high as 31.8%. Thus, an increase in canine seroprevalence may serve as an indicator of increasing Ebola virus circulation in primary vectors within specific geographical areas.
Human infection with African-derived strains has often occurred in caregivers (either family or medical) and in family members who have prepared dead relatives for burial. Late stages of Ebola virus disease are associated with the presence of large numbers of virions in body fluids, tissues, and, especially, skin. Individuals who are exposed to patients infected with Ebola without proper barrier protection are at high risk of becoming infected.
A report from the DRC identified Ebola virus RNA in 100% of oral secretions from patients who had the viral RNA in their serum. Both serum and oral secretions were tested with reverse-transcriptase polymerase chain reaction (RT-PCR) assay. Thus, oral secretions may be capable of transmitting Ebola virus.
Among infection survivors, only males had been shown to transmit the virus, via semen, in which the virus can persist for up to 2 years. However, a 2018 study found that previously infected women may also harbor a reservoir of dormant virus, which is theorized to have reactivated upon immunosuppression (suspected to result from pregnancy in the study case). [16]
The first recorded outbreak occurred in 1976, in Yambuku, DRC, where 316 patients were infected. In the largest recorded urban outbreak to date (DRC, 1995; 318 cases), admission to a hospital greatly amplified the frequency of transmission. The lack of proper barrier protection and the use and reuse of contaminated medical equipment, especially needles and syringes, resulted in rapid nosocomial spread of infection. Only after adequate barrier protection and alteration in burial rituals were implemented was the outbreak contained.
Unlike Asian-derived Ebola virus (ie, Reston ebolavirus, traced to a Philippine supplier of primates), African-derived species appear to be spread more often by direct contact than via the respiratory route. However, the Reston species has repeatedly been demonstrated to spread among nonhuman primates and possibly from primates to humans via the respiratory route. Fortunately, although the Reston species has been documented to be capable of infecting humans, it does not appear to be pathogenic to humans.
Epidemiology
Ebola virus is not endemic in the United States, although, during the 2014-2016 Ebola outbreak, several US healthcare personnel were in Africa and were transported to the United States for treatment, in addition to a traveller from Liberia who became ill and sought treatment while visiting Texas. The patient later died of the infection. One of his treating nurses then presented with a low-grade fever and tested positive for Ebola virus infection. In addition, individuals in several US states who travelled to West Africa developed fever and other symptoms, prompting evaluation for Ebola virus infection at US hospitals. [17]
Before the 2014 - 2016 outbreak, several human infections with the Reston strain of Ebola had been acquired by animal care workers at primate holding facilities within the United States. Fortunately, the Reston strain has not demonstrated pathogenic effects in humans. Others at potential risk are laboratory workers who work with inf ected animals or with the virus in tissue culture.
International statistics
On May 8, 2018, a new outbreak of Ebola virus disease was declared in the Democratic Republic of the Congo (DRC) following laboratory confirmation of 2 cases of EVD. [18] Before confirmation of the outbreak, 21 patients with signs of hemorrhagic fever had recently been reported in the country, 17 of whom died. [19] As of September 17, 2019, 3,034 confirmed cases had been reported and 111 probable cases, including 2,103 attributable deaths. [2, 3]
Ebola and Marburg viruses are responsible for well-documented outbreaks of severe human hemorrhagic fever, with resultant case mortalities ranging from 23% for Marburg virus to 89% for Ebola virus in which more than one case occurred.
The 2014-2016 Ebola virus outbreak was significant and primarily involved 3 African countries—Guinea, Liberia, and Sierra Leone. Localized transmission was been reported in Nigeria. Based on genetic analysis, the virus was 97% identical to the Zaire ebolavirus identified in cases in Gabon and the Democratic Republic of the Congo earlier in 2014. [20, 21]
At least 3 Americans in Africa were infected with Ebola in the 2014-2016 outbreak, 1 of whom died of the disease. [22]
Table 1. History of Sudan Ebola Virus Outbreaks (Open Table in a new window)
Year |
Country |
Cases |
Deaths |
Case Fatality Rate |
2012 |
Uganda |
7 |
4 |
57% |
2012 |
Uganda |
24 |
17 |
71% |
2011 |
Uganda |
1 |
1 |
100% |
2004 |
Sudan |
17 |
7 |
41% |
2000 |
Uganda |
425 |
224 |
53% |
1979 |
Sudan |
34 |
22 |
65% |
1976 |
Sudan |
284 |
151 |
53% |
| Data from World Health Organization | ||||
Table 2. History of Zaire Ebola Virus Outbreaks (Open Table in a new window)
Year |
Country |
Cases |
Deaths |
Case Fatality Rate |
2018-2019 |
Democratic Republic of the Congo (DRC) |
Ongoing |
||
2018 |
DRC |
54 |
33 |
61% |
2017 |
DRC |
8 |
4 |
50% |
2015 |
Italy |
1 |
0 |
0% |
2014 |
Spain |
1 |
0 |
0% |
2014 |
UK |
1 |
0 |
0% |
2014 |
USA |
4 |
1 |
25% |
2014 |
Senegal |
1 |
0 |
0% |
2014 |
Mali |
8 |
6 |
75% |
2014 |
Nigeria |
20 |
8 |
40% |
2014-2016 |
Sierra Leone |
14,124* |
3,956* |
28% |
2014-2016 |
Liberia |
10,675* |
4,809* |
45% |
2014-2016 |
Guinea |
3,811* |
2,543* |
67% |
2008 |
DRC |
32 |
14 |
44% |
2007 |
DRC |
264 |
187 |
71% |
2005 |
Republic of the Congo |
12 |
10 |
83% |
2003 (Nov-Dec) |
Republic of the Congo |
35 |
29 |
83% |
2003 (Jan-Apr) |
Republic of the Congo |
143 |
128 |
90% |
2001-2002 |
Republic of the Congo |
59 |
44 |
75% |
2001-2002 |
Gabon |
65 |
53 |
82% |
1996 |
South Africa (ex-Gabon) |
1 |
1 |
100% |
1996 (Jul-Dec) |
Gabon |
60 |
45 |
75% |
1996 (Jan-Apr) |
Gabon |
31 |
21 |
68% |
1995 |
DRC |
315 |
254 |
81% |
1994 |
Gabon |
52 |
31 |
60% |
1977 |
DRC |
1 |
1 |
100% |
1976 |
DRC |
318 |
280 |
88% |
| *Includes suspected, probable, and confirmed EVD cases. Data from World Health Organization. | ||||
Table 3. History of Tai Forest (Ivory Coast, Côte-d’Ivoire) Ebola Virus Outbreaks (No Deaths Reported) (Open Table in a new window)
Year |
Location |
Reported Cases, No. |
1994 |
Côte-d’Ivoire |
1 |
Total |
|
1 |
Data from Centers for Disease Control and Prevention and World Health Organization. |
||
Table 4. History of Reston Ebola Virus Outbreaks (No Deaths Reported) (Open Table in a new window)
Year |
Location |
Proven * Cases Reported, No. |
1989 |
Virginia, Texas, Pennsylvania |
0 |
1990 |
Virginia and Texas |
4 |
1989-1990 |
Philippines |
3 |
1992 |
Italy |
0 |
1990 |
Alice, TX |
0 |
1996 |
Philippines |
0 |
Nov 2008 |
Philippines† |
6 |
Total |
|
13 |
Data from Centers for Disease Control and Prevention and World Health Organization. * Humans with serologic evidence of infection but without clinical disease. |
||
Table 5. History of Bundibugyo Ebola Virus Outbreak (Open Table in a new window)
Year |
Location |
Reported Cases, No. |
Deaths, No. (%) |
Dec 2007 to Jan 2008 |
Uganda |
149 |
37 (25) |
Jun to Nov 2012 |
Democratic Republic of the Congo |
57 |
29 (50.1) |
Total |
|
206 |
66 (32) |
Data from Centers for Disease Control and Prevention and World Health Organization. |
|||
Individuals considered at risk for Ebola hemorrhagic fever include persons with a travel history to sub-Saharan Africa, persons who have recently cared for infected patients, and animal workers who have worked with primates infected with African-derived Ebola subtypes. In 2011, Uganda experienced a reemergence of the disease. [25]
Age-related demographics
In the 1995 outbreak in Kikwit, DRC, infection rates were significantly lower in children than in adults. During this outbreak, only 27 (8.6%) of the 315 patients diagnosed with Ebola virus infection were 17 years of age or younger. This apparent sparing of children occurs even though 50% of the population of the DRC is younger than 16 years. Although definitive evidence is lacking, epidemiologic evidence suggests that children are less likely to come into direct contact with ill patients than adults are.
Other viral hemorrhagic syndromes, such as Crimean-Congo hemorrhagic fever and hantavirus infections, also show a predominance of adult patients and a relative sparing of young children.
Sex-related demographics
Ebola virus infection has no sexual predilection, but men and women differ with respect to the manner in which direct exposure occurs.
Men, by the nature of their work exposure in forest and savanna regions, may be at increased risk of acquiring a primary infection from gathering “bush meat” (primate carcasses) for food, as well as an unknown vector or vectors. Evidence from Africa and the Philippines is compatible with bats being a principal vector of Ebola virus.
Because women provide much of the direct care for ill family members and are involved in the preparation of the bodies of the deceased, they may be at increased risk of acquiring Ebola virus infection through their participation in these activities; however, men and women who are medical healthcare providers seem to share a high and equal risk for infection.
Race-related demographics
Because most cases of Ebola virus infection have occurred in sub-Saharan Africa, most patients have been black. However, no evidence exists for a specific racial predilection.
Prognosis
The overall prognosis for patients with Ebola virus infection is poor. [5] However, those who survive for 2 weeks often make a slow recovery.
With the exception of the Reston strain, Ebola virus is associated with very high morbidity and mortality among patients who present with clinical illness, though these vary according to the causative species. The most highly lethal Ebolavirus species is Zaire ebolavirus, which has been reported to have a mortality rate as high as 89%. Sudan ebolavirus also has high reported mortality, ranging from 41% to 65%.
-
Ebola virus. Courtesy of the US Centers for Disease Control and Prevention.