Background
Human cryptosporidiosis is caused by infection with apicomplexan protozoans of the genus Cryptosporidium. [1, 2] Human illness was once believed to be caused by a single species, but molecular studies have demonstrated that it is caused by at least 15 different species. Among the more common species is Cryptosporidium hominis, for which humans are the only natural host, and Cryptosporidium parvum, which infects a range of mammals, including humans. [1, 2, 3] (See Etiology and Pathophysiology.)
Cryptosporidiosis mainly affects children. It causes a self-limited diarrheal illness in otherwise healthy adults. However, it is also recognized as a cause of prolonged and persistent diarrhea in children, which can result in malnutrition. [4, 5] Cryptosporidiosis can manifest as chronic severe diarrhea in persons with acquired immunodeficiency syndrome (AIDS), solid and bone marrow transplants or immunosuppression due to chemotherapy/immunotherapy. [6, 7, 8] (See Prognosis and Presentation.)
Cryptosporidium can also cause waterborne and, less frequently, foodborne outbreaks.(See Epidemiology, Workup, and Treatment.)
The genus Cryptosporidium consists of a group of protozoan parasites within the phylum Apicomplexa. As of 2019, there were at least 35 named Cryptosporidium species, as recognized by host specificity, morphology, and molecular biology studies. [9, 10, 11] Besides humans, the parasite can infect many other species of animals, such as mammals, birds, and reptiles, and is pathogenic to immunocompetent and immunocompromised hosts.
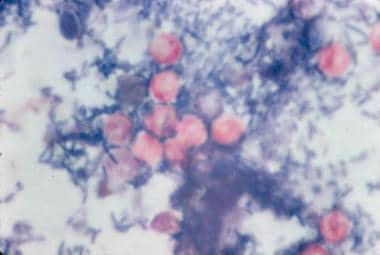 Modified acid-fast stain of stool shows red oocysts of Cryptosporidium parvum against the blue background of coliforms and debris.
Modified acid-fast stain of stool shows red oocysts of Cryptosporidium parvum against the blue background of coliforms and debris.
See Common Intestinal Parasites, a Critical Images slideshow, to help make an accurate diagnosis.
Cryptosporidium species that infect humans replicate in the epithelial cell lining of the GI tract. They can complete their entire life cycle within a single host, but some species can also spread between host species. [12] C hominis and C parvum cause most human infections. Both can spread person to person. C parvum can also be zoonotic.
Transmission
The disease is transmitted via the fecal-oral route from infected hosts. Most sporadic infections occur through person-to-person contact. Nonetheless, transmission can also occur following animal contact, ingestion of water (mainly during swimming), or through food. [12, 13, 14] Waterborne outbreaks have resulted from contamination of municipal water and recreational waters (eg, swimming pools, ponds, lakes).
Animal contact can also be associated with transmission of zoonotic species.(See Etiology and Treatment.)
Cryptosporidium has emerged as the most frequently recognized cause of recreational water–associated outbreaks of gastroenteritis, particularly in treated (disinfected) venues. This is because, in the oocyst stage of its life cycle, Cryptosporidium can resist disinfection, including chlorination, and can survive for a prolonged period in the environment. Foodborne outbreaks also occur but with less frequency.
Life cycle
Cryptosporidium species do not multiply outside the host. [1, 2, 3] Infection is initiated by ingestion of oocysts, which are activated in the stomach and upper intestines to release four infective sporozoites (see the first image below). These motile sporozoites bind to the receptors on the surface of the intestinal epithelial cells (see the second image below) and are ingested into a parasitophorous vacuole near the surface of the epithelial cell, separated from the cytoplasm by a dense layer. Cryptosporidium oocysts are round and measure 4.2-5.4 µm in diameter.
 Cryptosporidium species oocysts are rounded and measure 4.2-5.4 µm in diameter. Sporozoites are sometimes visible inside the oocysts, indicating that sporulation has occurred on wet mount.
Cryptosporidium species oocysts are rounded and measure 4.2-5.4 µm in diameter. Sporozoites are sometimes visible inside the oocysts, indicating that sporulation has occurred on wet mount.
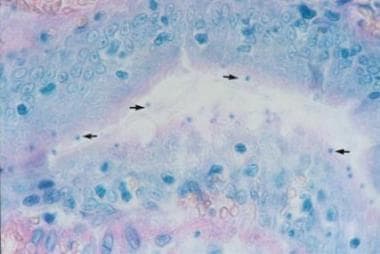 Hematoxylin and eosin stain of intestinal epithelium. The blue dots (arrows) represent intracellular Cryptosporidium organisms along the surface of the epithelial cells. Image courtesy of Carlos Abramowsky, MD, Professor of Pediatrics and Pathology, Emory University School of Medicine.
Hematoxylin and eosin stain of intestinal epithelium. The blue dots (arrows) represent intracellular Cryptosporidium organisms along the surface of the epithelial cells. Image courtesy of Carlos Abramowsky, MD, Professor of Pediatrics and Pathology, Emory University School of Medicine.
Once inside the epithelial cell, the parasites enlarge, divide, and reinvade other cells in a series of sexual and asexual multiplication steps, eventually leading to the production of oocysts. Two morphologic forms of the oocysts have been described: thin-walled oocysts (asexual stage) excyst within the same host (causing self-infection), whereas the thick-walled oocysts (sexual stage) are shed into the environment. Oocyst shedding can continue for weeks after the host experiences clinical improvement.
Etiology and Pathophysiology
Cryptosporidium oocysts are highly infectious, requiring fewer than 10 oocysts to cause human disease for some isolates. [15, 16] The oocysts are infectious immediately after excretion, and the life cycle of the parasite produces forms that reinvade the intestine. The location of the parasite in the intestine is intracellular but extracytoplasmic, which may contribute to the marked resistance of Cryptosporidium species to treatment. Large numbers of oocysts are excreted and are resistant to harsh conditions, including chlorine at levels usually applied in water treatment.
Cryptosporidiosis typically presents with watery diarrhea. The mechanism by which Cryptosporidium causes diarrhea includes a combination of increased intestinal permeability, chloride secretion, and malabsorption, which are all thought to be mediated by the host response to infection. [2, 17, 18] Severe disease is characterized by villous atrophy and crypto-hyperplasia. [18] In immunocompetent persons, the infection is usually limited to the small intestine. In persons with AIDS or certain congenital immunodeficiencies, the biliary and respiratory tracts may be involved. [19]
Risk factors
Among healthy individuals, cryptosporidiosis is primarily a childhood disease. Daycare center–related outbreaks have a high infection rate (30%-60%). Risk groups include childcare workers; parents of infected children; international travelers, including backpackers and hikers who drink unfiltered untreated water; swimmers who swallow contaminated recreational water; people who handle infected animals; and people exposed to human feces through sexual contact. [1, 2, 12, 13, 14, 20, 21]
Individuals with compromised cellular immunity are at an increased risk of symptomatic cryptosporidiosis, particularly severe disease. Immunodeficiency may be congenital (especially in individuals with hyper–immunoglobulin M [IgM] syndrome) or may result from HIV infection, malnutrition, cancer, immunotherapy or organ transplantation. [7, 8] Pregnancy is another predisposing factor for cryptosporidiosis. In resource-limited countries, the prevalence of Cryptosporidium infection is significantly higher than in industrialized countries because of a lack of clean water and sanitary facilities, crowding, and animal reservoirs in close proximity to residences. In a systematic review, overcrowding, diarrhea in household, and animal contact were the major risk factors for infection in low- and middle-income countries. [5, 22] No increased risk with water source was observed.
Epidemiology
Occurrence in the United States
The frequency of cryptosporidiosis has not been well-defined in the United States. Many laboratories do not routinely test for Cryptosporidium. Laboratories that test for Cryptosporidium often use insensitive tests. [1, 2] The number of reported cases has risen with increased awareness and improved diagnostic testing. From 2006-2010, the rate was between 2.3 and 3.9 cases per 100,000 population, with 13,453 cases reported in 2016. [23, 24] However, estimates suggest that the frequency of infection is likely to be 100-fold higher than the number of reported cases. [25]
Studies in the United States have documented cryptosporidiosis in about 4% of stools sent for parasitologic examination. Seroprevalence studies suggest that 25%-35% of the population in industrialized countries (including the United States) have had cryptosporidiosis at some time in their life. Cryptosporidium species also cause waterborne outbreaks of diarrhea. In 1993, more than 400,000 cases of diarrheal illness due to Cryptosporidium infection were reported in Milwaukee, Wisconsin. [26] Waterborne outbreaks continue to be common worldwide. [12, 13, 27, 28]
Cryptosporidium parasites are ubiquitous, except in Antarctica, and infection is more common in warm, moist months. [1, 2, 3] In the United States, the incidence peaks from July through September. In England, there are separate peaks, in the spring (associated with C parvum and farm animals) and the fall (associated with C hominis and recreational water). [13, 14] Outbreaks in daycare centers with incidence rates of 30%-60% have been reported. [29]
Prior to the availability of combination antiretroviral therapy, approximately 10%-15% of patients with AIDS developed cryptosporidiosis over their lifetime. As with other opportunistic infections, the prevalence of cryptosporidiosis in patients with AIDS has dropped dramatically. [30]
International statistics
Cryptosporidiosis is a notifiable disease at the European Union level, and surveillance data are collected through the European Basic Surveillance Network. [31] The crude incidence rate was similar to that in the United States, although considerable differences in the rates of cryptosporidiosis were observed between countries and over time. In resource-limited countries, most infections occur in children.
In a large multicenter study of moderate to severe diarrhea in sub-Saharan Africa and South Asia, Cryptosporidium was second only to rotavirus as a cause of diarrhea in children younger than 2 years and was associated with 200,000 deaths. [32] A multicenter birth cohort study from Asia, Africa, and Latin America (the malnutrition and enteric disease study) also found Cryptosporidium to be among the top causes of diarrheal disease, and nondiarrheal infection was associated with malnutrition. [5, 33] Studies suggest that the burden of disease related to malnutrition may be greater than that due to diarrhea. [4, 34]
Reported rates are often higher when molecular tests such as polymerase chain reaction (PCR) are used. [35] For example, investigations using PCR assays have found Cryptosporidium species in 6% of American travelers to Mexico. [36]
In persons with AIDS, cryptosporidiosis is more common in developing countries, affecting 12%-48% of persons with AIDS who have diarrhea. [1, 34, 37, 38]
Data about incidence and prevalence of infection in solid and bone marrow organ transplant are limited. A few retrospective case reports in renal transplant recipients report a prevalence between 4.5 and 53%. [39]
Age-related demographics
The peak incidence of cryptosporidiosis is in children younger than 5 years. [24] Infection is infrequently diagnosed in immunocompetent adults in resource-limited countries. A second peak includes women of childbearing age (likely due to contact with infected children). [24] Cryptosporidiosis can occur in persons with AIDS of any age.
Children younger than 2 years may be more susceptible to infection, possibly because of increased fecal-oral transmission in this age group and because of a lack of protective immunity. Waterborne epidemics in industrialized countries affect all ages.
Prognosis
In most healthy individuals, Cryptosporidium infection–induced diarrhea is usually self-limited. However, diarrhea is often prolonged (>1 week) or persistent (>2 weeks). In patients who are immunocompromised, cryptosporidiosis may be chronic, severe, sometimes fatal, and with extraintestinal manifestations.
Individuals with AIDS and cryptosporidiosis tend to develop chronic symptoms more often, and about 10% have a fulminant course. [1, 18] Antiretroviral treatment improves outcomes.
Immunocompetent children with Cryptosporidium infection generally fare well. However, persistent abdominal pain, loose stools, and extraintestinal sequelae (eg, joint pain, eye pain, headache, dizzy spells, fatigue) have been reported, especially with C hominis infection. [13]
Morbidity and Mortality
Complications of cryptosporidiosis include the following:
-
Respiratory tract involvement has been described in patients with AIDS and in children with intestinal cryptosporidiosis who are otherwise healthy. [41]
Patient Education
Thorough hand washing should be practiced by patients with diarrhea to avoid the spread of the disease. The effectiveness of alcohol-based hand sanitizers has not been well studied, and their use should not be recommended.
Subjects with diarrhea should avoid using public swimming pools during their illness and at least 2 weeks after diarrhea has subsided.
Encourage immunocompromised patients to consider using 1-μm water filters when drinking tap water. Also consider boiled or bottled drinking water for patients who are immunocompromised, particularly those with HIV who have fewer than 200 CD4 cells/µL. Persons living in countries with a high risk of transmission should also be encouraged to use bottled or filtered water.
Immunocompromised patients (eg, patients with AIDS or solid organ transplant recipients) should avoid newborn animals (eg, calves, lambs), including domestic animals, and people with diarrhea. They should also consider avoiding communal recreational water such as public swimming pools. New pets for patients with AIDS should be older than 6 months and should not have diarrhea.
Instruct patients with AIDS, daycare workers, food handlers, and healthcare workers to avoid fecal-oral spread by wearing gloves and washing their hands after contact with human feces. Spread can occur after activities such as changing diapers.
-
Modified acid-fast stain of stool shows red oocysts of Cryptosporidium parvum against the blue background of coliforms and debris.
-
Hematoxylin and eosin stain of intestinal epithelium. The blue dots (arrows) represent intracellular Cryptosporidium organisms along the surface of the epithelial cells. Image courtesy of Carlos Abramowsky, MD, Professor of Pediatrics and Pathology, Emory University School of Medicine.
-
Cryptosporidium species oocysts are rounded and measure 4.2-5.4 µm in diameter. Sporozoites are sometimes visible inside the oocysts, indicating that sporulation has occurred on wet mount.
-
Cryptosporidium parvum oocysts revealed with modified acid-fast stain. Against a blue-green background, the oocysts stand out with a bright red stain. Image courtesy of CDC DPDx parasite image library.
-
Cryptosporidium oocysts revealed with modified acid-fast stain.






