Practice Essentials
Rectal prolapse was described as early as 1500 BCE. Rectal prolapse occurs when a mucosal or full-thickness layer of rectal tissue protrudes through the anal orifice. [1, 2] Problems with fecal incontinence, constipation, and rectal ulceration are common.
Three different clinical entities are often combined under the umbrella term rectal prolapse:
-
Full-thickness rectal prolapse
-
Mucosal prolapse
-
Internal prolapse (internal intussusception)
Treatment of these three entities differs.
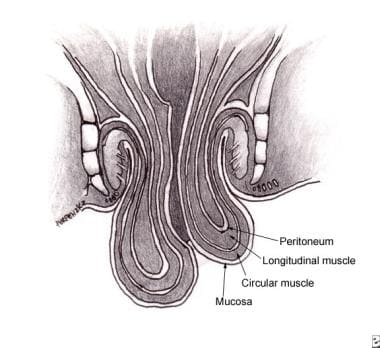
Full-thickness rectal prolapse (see the image below) is defined as protrusion of the full thickness of the rectal wall through the anus; it is the most commonly recognized type. Mucosal prolapse, in contrast, is defined as protrusion of only the rectal mucosa (not the entire wall) from the anus. Internal intussusception may be a full-thickness or a partial rectal wall disorder, but the prolapsed tissue does not pass beyond the anal canal and does not pass out of the anus.
Most of this article focuses on full-thickness rectal prolapse, which will be referred to as rectal prolapse.
In adult patients, treatment of rectal prolapse is essentially surgical; no specific medical treatment is available. [3] (See Treatment.) Children, however, can usually be treated nonsurgically and by managing the underlying condition. There is no widespread agreement as to which repair constitutes the best treatment. Laparoscopic approaches have been developed that have outcomes as good as those of open abdominal procedures but are associated with shorter hospital stays and greater patient comfort.
Anatomy
The rectum is the distal 12-15 cm of the large intestine between the sigmoid colon and the anal canal. It primarily serves as a reservoir for fecal material. The mucosa is the inner lining of the intestinal tract. The dentate line is the junction of the ectoderm and endoderm in the anal canal.
The internal anal sphincter is a smooth muscle that is the most distal extension of the inner circular smooth muscle of the colon and the rectum. It is 2.5-4 cm long and normally 2-3 mm thick. The internal sphincter is not under voluntary control and is continuously contracted to prevent unplanned loss of stool.
The external anal sphincter is striated muscle that forms a circular tube around the anal canal. Moving proximally, it merges with the puborectalis and the levator ani to form a single complex. Control of the external anal sphincter is voluntary.
Pathophysiology
The pathophysiology of rectal prolapse is not completely understood or agreed upon. There are two main theories, which essentially are different ways of expressing the same idea.
The first theory postulates that rectal prolapse is a sliding hernia through a defect in the pelvic fascia. The second theory holds that rectal prolapse starts as a circumferential internal intussusception of the rectum beginning 6-8 cm proximal to the anal verge. With time and straining, this progresses to full-thickness rectal prolapse, though some patients never progress beyond this stage.
The pathophysiology and etiology of mucosal prolapse most likely differ from those of full-thickness rectal prolapse and internal intussusception. [4] Mucosal prolapse occurs when the connective tissue attachments of the rectal mucosa are loosened and stretched, thus allowing the tissue to prolapse through the anus. This often occurs as a continuation of long-standing hemorrhoidal disease and is treated as such.
Often, prolapse begins with an internal prolapse of the anterior rectal wall and progresses to full prolapse.
Etiology
The precise cause of rectal prolapse is not defined; however, a number of associated abnormalities have been found. As many as 50% of prolapse cases are caused by chronic straining with defecation and constipation.
Other predisposing conditions include the following:
-
Pregnancy
-
Previous surgery
-
Diarrhea
-
Benign prostatic hypertrophy
-
Chronic obstructive pulmonary disease (COPD)
-
Cystic fibrosis
-
Pertussis (ie, whooping cough)
-
Pelvic floor dysfunction
-
Parasitic infections – Amebiasis, schistosomiasis
-
Neurologic disorders - Previous lower back or pelvic trauma/lumbar disk disease, cauda equina syndrome, spinal tumors, multiple sclerosis
-
Disordered defecation (eg, stool withholding)
Certain anatomic features found during surgery for rectal prolapse are common to most patients. These features include a patulous or weak anal sphincter with levator diastasis, deep anterior Douglas cul-de-sac, poor posterior rectal fixation with a long rectal mesentery, and redundant rectosigmoid. Whether these anatomic features are the cause or result of the prolapsing rectum is not known. [5]
In children, rectal prolapse is probably related to the vertical orientation of the rectum, the mobility of the sigmoid colon, the relative weakness of the pelvic floor muscle, mucosa that is poorly fixed to submucosa, and redundant rectal mucosa.
Epidemiology
United States statistics
Rectal prolapse is uncommon; however, the true incidence is unknown because of underreporting, especially in the elderly population. Peaks in occurrence are noted in the fourth and seventh decades of life, and most patients (80-90%) are women. [6]
The condition is often concurrent with pelvic floor descent and prolapse of other pelvic floor organs, such as the uterus or the bladder. Although multiple pregnancies are often implicated in the etiology, 35% of patients are nulliparous. A small subset of children is affected, usually before the age of 3 years. Evaluation and treatment of children with rectal prolapse is addressed elsewhere.
International statistics
The annual incidence of rectal prolapse in Finland was found to be 2.5 per 100,000 population. [7]
Age-related demographics
Although all ages can be affected, peak incidences are observed in the fourth and seventh decades of life. Pediatric patients usually are affected when younger than 3 years, with the peak incidence in the first year of life. Mucosal prolapse is more common than complete prolapse (possibly because of poor fixation of the submucosa to the mucosa in pediatric patients). The incidence of prolapsed rectum in children with cystic fibrosis approaches 20%.
Sex-related demographics
In the adult population, the male-to-female ratio is 1:6. Although in the adult population, women account for 80-90% of cases, in the pediatric population, the incidence of rectal prolapse is evenly distributed between males and females. [8]
Prognosis
The prognosis generally is good with appropriate treatment. Spontaneous resolution usually occurs in children. Of patients with rectal prolapse who are aged 9 months to 3 years, 90% will need only conservative treatment. Continence usually is initially worse after surgical treatment, but in most patients it improves over time; however, the degree of improvement is unpredictable.
Untreated rectal prolapse can lead to incarceration and strangulation (rare). More commonly, increasing difficulties with rectal bleeding (usually minor), ulceration, and incontinence occur.
Postoperative mortality is low, but the recurrence rate can be as high as 15%, regardless of the operative procedure performed (see below). The most common postoperative complications involve bleeding and dehiscence at the anastomosis. Other complications include mucosal ulceration and necrosis of the rectal wall. Operative complications are higher for abdominal operations, with a lower recurrence rate; the opposite is true for perineal operations, which have a much lower complication rate but a higher recurrence rate.
Recurrence
The recurrence rate for anterior resection without sacral fixation is about 7-9%, with a morbidity of 15-29%. This recurrence rate is higher than that for other abdominal procedures.
The recurrence rate for Marlex rectopexy ranges from 2% to 10%, with a morbidity of 3-29%. Continence is improved in 50-70% of patients. Constipation, however, is not improved and may worsen after this operation. The results of suture rectopexy are comparable.
The recurrence rate for resection and rectopexy is 3-4%, with several studies reporting a 0% recurrence rate. Morbidity ranges from 4% to 23%. Because the redundant colon is also resected, constipation improves in 60-80% of patients, and continence improves in 35-60%.
The recurrence rate for Delorme mucosal sleeve resection ranges from 5% to 26%, with a variable morbidity that is usually related to the patient’s underlying comorbidities. Fecal incontinence and constipation improve in about 50% of patients.
The recurrence rate for Altemeier perineal rectosigmoidectomy ranges from 0% to 50%, with an average of approximately 10%. Continence may be improved if a levator plication is added to the procedure. A study by Altomare et al indicated that restoration of continence with this procedure can be unpredictable. [9]
-
Rectal prolapse.
-
Full-thickness rectal prolapse.
-
Marlex rectopexy for rectal prolapse.
-
Delorme mucosal sleeve resection for rectal prolapse.
-
Altemeier perineal rectosigmoidectomy for rectal prolapse.