Practice Essentials
Patients suffering from lipodystrophies experience reduced body fat, severe insulin resistance, hypertriglyceridemia, and hypoleptinemia, and nonalcoholic fatty liver disease. [1, 2, 3] The depletion of adipose tissue results in excess calories being diverted to the liver, skeletal muscle, and pancreas, impairing insulin action. [2, 4]
An estimated 1-5 million individuals in the United States have a lipodystrophy syndrome, but accurate data are difficult to obtain owing to the rarity of these conditions. [2] However, it is known that millions of US individuals have obesity and type 2 diabetes mellitus. Obesity is characterized by increased body adiposity and leads to insulin resistance. The resemblance between the metabolic abnormalities of these extreme states of adiposity underscores the importance of fat tissue in energy homeostasis. (See the image below.)
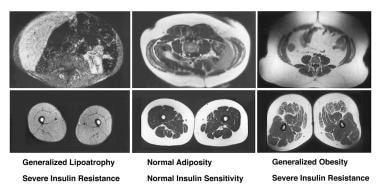 Generalized Lipodystrophy. Clinical spectrum of adiposity. These are T1-weighted magnetic resonance images in which lipid appears white. Transverse sections of the torso are shown at the level of the fifth lumbar vertebra (top panels) and of the midthigh (bottom panels). Note generalized lipoatrophy (top left, bottom left) in a healthy individual with a body mass index (BMI) of 24 kg/m2 (top center, bottom center), and an individual who is obese with a BMI of 38 kg/m2 (top right, bottom right). Note the marked absence of all fat depots in the patient with generalized lipoatrophy, with preservation of marrow fat and a lipid-filled liver. In addition, the bright color of the muscle is indicative of lipid-filled myocytes.
Generalized Lipodystrophy. Clinical spectrum of adiposity. These are T1-weighted magnetic resonance images in which lipid appears white. Transverse sections of the torso are shown at the level of the fifth lumbar vertebra (top panels) and of the midthigh (bottom panels). Note generalized lipoatrophy (top left, bottom left) in a healthy individual with a body mass index (BMI) of 24 kg/m2 (top center, bottom center), and an individual who is obese with a BMI of 38 kg/m2 (top right, bottom right). Note the marked absence of all fat depots in the patient with generalized lipoatrophy, with preservation of marrow fat and a lipid-filled liver. In addition, the bright color of the muscle is indicative of lipid-filled myocytes.
Lipodystrophy, the abnormal distribution of fat, encompasses lipoatrophy, the loss of fat, and other abnormalities of adipose tissue. This article focuses on generalized lipoatrophy, a rare group of syndromes, either acquired (Lawrence-Seip syndrome) or congenital (Berardinelli-Seip syndrome), characterized by a near-complete absence of fat. [3] See the image below.
 Generalized Lipodystrophy. Acquired generalized lipoatrophy is in the differential diagnosis of congenital generalized lipoatrophy. The patient shown, who had completely normal fat distribution at age 3 years and 8 months (left), acutely lost her body fat with a febrile illness at age 6 years and10 months (right).
Generalized Lipodystrophy. Acquired generalized lipoatrophy is in the differential diagnosis of congenital generalized lipoatrophy. The patient shown, who had completely normal fat distribution at age 3 years and 8 months (left), acutely lost her body fat with a febrile illness at age 6 years and10 months (right).
Pathophysiology
Mechanisms for adipocyte deficiency include the following:
-
Defects in adipogenesis pathway
-
Increased destruction of adipocytes (eg, induction of apoptosis)
Potential mechanisms that may explain insulin resistance and other metabolic abnormalities caused by fat loss in lipoatrophy syndromes include the following [5] :
-
Inability to store triglycerides: Leads to abnormal deposition of triglycerides in other tissues (eg, liver, skeletal muscle, and pancreas [lipotoxicity]), resulting in hypertriglyceridemia, insulin resistance, hepatic steatosis (fatty liver), impaired insulin secretion, and, eventually, type 2 diabetes
-
Absent or immature adipocytes: Inability to synthesize and release adipocytokines (eg, leptin, adiponectin) that may be important to maintain normal metabolism
Classification of lipoatrophy syndromes
Lipodystrophies are categorized based on etiology (genetic or acquired) and distribution of lost adipose tissue, affecting the entire body (generalized) or only regions (partial). The four main subtypes are as follows [1] :
-
Congenital generalized lipoatrophy (CGL): Autosomal recessive; near total absence of body fat, generalized muscularity, metabolic complications
-
Familial partial lipodystrophy (FPLD): Autosomal dominant; absence of fat in limbs, metabolic complications
-
Acquired generalized lipodystrophy (AGL): Near total absence of body fat, metabolic complications
-
Acquired partial lipodystrophy (APL): Absence of fat in upper body with increased fat in lower body, mild or no metabolic complications
Additional genetic subtypes include progeroid syndromes, autoinflammatory disorders, and SHORT syndrome. [1] Other acquired subtypes include a localized lipodystrophy seen in injection drug users. Additionally, aggressive treatment of patients infected with human immunodeficiency virus (HIV), cause loss of subcutaneous fat from the face, extremities, and trunk [6] ; increased visceral fat, with buffalo hump, [7, 8, 9] accompanied by insulin resistance and hypertriglyceridemia.
Diagnosis
In 2016, consensus guidelines for the diagnosis and management of lipodystrophy syndromes was published and endorsed by multiple societies globally including the Pediatric Endocrine Society, American Diabetes Association, American Association of Clinical Endocrinologists, Endocrine Society, Japanese Society for Pediatric Endocrinology, Australasian Pediatric Endocrine Group, European Society for Pediatric Endocrinology, Asia Pacific Pediatric Endocrine Society, African Society for Pediatric and Adolescent Endocrinology, and International Society for Pediatric and Adolescent Diabetes.
Diagnostic criteria for lipodystrophy have not been established and no defined serum lipid levels establish or exclude the diagnosis. The guidelines include a diagnostic algorithm along with the following recommendations [1] :
-
Base diagnosis on history, physical examination, body composition, and metabolic status. (Class I, Level B)
-
Genetic testing to confirm diagnosis is helpful in suspected genetic subtypes. (Class I, Level A)
-
Genetic testing should be considered in at-risk family members. (Class IIa, Level C)
-
Serum complement levels and autoantibodies may support diagnosis of acquired lipodystrophy syndromes. (Class IIa, Level B)
In 2021, the Japan Endocrine Society released their practice guideline for lipodystrophy syndromes. [2]
Suspect and evaluate the extent of lipodystrophy (generalized or partial, regional) when patients are examined who have severe insulin resistance, diabetes, hypertriglyceridemia, and metabolic disorders (eg, nonalcoholic fatty liver disease [NAFLD]). Rule out other conditions that can cause leanness and weight loss, as well as evaluate the possibility of progeroid and autoinflammatory syndrome on the basis of the patient's physical features.
A mutational analysis of causative genes is typically needed for a definitive diagnosis (eg, CGL and FPLD for the diagnosis of congenital lipodystrophy syndromes). Other useful diagnostic studies include levels of plasma leptin and whole-body T1-weighted magnetic resonance imaging (MRI).
Management
No curative treatment currently exists for lipodystrophy syndromes, and no cure yet exists for adipose tissue atrophy. The goal of therapeutic strategies is primarily to ameliorate metabolic derangements or conditions that arise from lipodystrophy. If needed, consider plastic surgical approaches.
The clinical problems requiring treatment in lipoatrophy syndromes are diabetes and hypertriglyceridemia. Lifestyle modifications alone may not be sufficient and may need to be implemented along with pharmacotherapy.
Diabetes
Although several classes of antidiabetic drugs are marketed in the United States, achieving good glycemic control (glycated hemoglobin < 6.5%) is difficult for most patients with lipoatrophic diabetes.
Pharmacotherapy for lipoatrophy/lipodystrophy syndromes includes the following:
-
Leptin analogs (eg, metreleptin)
-
Insulin: Extremely high doses (eg, >1000 U/d) are often necessary in patients with various syndromes of lipoatrophy [10]
-
Insulin secretagogues
-
Metformin
Hypertriglyceridemia
The dyslipidemia of severe lipoatrophy is difficult to treat with currently available therapeutic interventions. In addition, lifestyle modifications alone may not be sufficient and may need to be implemented along with pharmacotherapy.
Troglitazone is remarkable in its ability to improve hypertriglyceridemia in addition to improving glycemia. Some clinicians also prefer to use fibrates and statins rather than niacin because of severe insulin resistance.
In women with lipoatrophy syndromes, oral estrogens should be avoided as they can exacerbate the hypertriglyceridemia and result in acute pancreatitis. [5]
Pathophysiology
Over the last 2 decades, important advances have occurred in understanding the differentiation program of adipocytes. [11] Precursor cells are committed to adipogenesis through transient expression of certain transcription factors such as CCAAT/enhancer-binding protein-beta (C/EBP–beta) and C/EBP-delta and thus become preadipocytes. Preadipocytes gain the ability to store triglycerides and repress cell-cycle genes through the activation of multiple genes controlled by key transcription factors (ie, peroxisome proliferator-activated receptor-gamma [PPAR-gamma] and C/EBT-alpha). Other transcription factors are involved either in activating these key factors or in controlling the synthesis of their ligands (eg, sterol regulatory element binding transcription factor 1 [SREBP1]/adipocyte determination and differentiation factor 1 [ADD1] may regulate synthesis of ligands for PPAR-gamma).
Defects in both of these commitment steps may lead to adipocyte deficiency. Another mechanism for adipocyte deficiency is through increased destruction of these cells (eg, induction of apoptosis). The exact control of adipocyte turnover or constant remodeling in adults is not understood.
A novel molecule called lipin has been cloned as a result of positional cloning efforts to identify the genetic etiology of a naturally occurring mouse model with partial lipoatrophy and fatty liver. This molecule is a novel protein with nuclear localization and is induced during adipocyte differentiation. [12] Its exact role in the adipocyte differentiation pathway remains to be identified.
Adipose tissue is an endocrine organ, an important concept that was proven by the discovery of the hormone leptin. Adipocytes communicate body fat levels to the neuroendocrine system to control food intake and energy expenditure. Leptin has effects (direct or indirect) on the key organs of metabolism, including the liver, muscle, and pancreas.
Another intriguing signal originating from adipocytes is a 30-kd molecule called adipocyte complement–related protein 30 (ACRP 30) [13] or adipoQ. [14] Other independent groups that have cloned this molecule called it adipocyte most abundant gene transcript 1 (APM1). Now it is most commonly called adiponectin. [15] This molecule appears to be important in inducing fat oxidation in the muscle and liver. [13] It promotes insulin sensitivity and is found to be decreased in various forms of insulin resistance. [16] Lack of adipocytes results in deficiency of these signals, contributing to many of the abnormalities observed in persons with syndromes characterized by an absence of fat.
Animal models of lipoatrophy have been engineered via either disruption of adipogenesis or induction of adipocyte death. These models help explain the pathophysiology of fat loss. These models use an adipose-specific promoter/enhancer to introduce a transgene. Reviews of animal models of lipoatrophy can be found elsewhere. [17, 18]
There are two consequences of fat loss that could explain the insulin resistance and other metabolic abnormalities seen in lipoatrophy syndromes. [5] One is that the inability to store triglycerides in adipocytes leads to abnormal deposition of triglycerides in other tissues such as the liver, skeletal muscle, and pancreas (lipotoxicity), resulting in hypertriglyceridemia, insulin resistance, hepatic steatosis (fatty liver), impaired insulin secretion and eventually type 2 diabetes. [2]
Second, adipocytes are either absent or immature and therefore unable to synthesize and release adipocytokines that may be important to maintain normal metabolism. [2] Two such adipocytokines, leptin and adiponectin, have been shown to be low in patients with lipoatrophy syndromes. Leptin acts on the central nervous system to regulate food intake and energy expenditure. Leptin deficiency can lead to decreased metabolic rate and voracious appetite with overconsumption of calories and worsening metabolic state. Cases of dramatic leptin deficiency or receptor nonrecognition of leptin have been described. [19, 20]
Both leptin and adiponectin promote the storage of fat in adipose tissue and inhibit the deposition of excess fat in other tissues such as liver and muscle. These hormones can also promote free fatty acid oxidation in skeletal muscle and liver, increase glucose uptake and decrease hepatic gluconeogenesis. Leptin replacement therapy is currently being used as an investigational therapy in patients with lipoatrophy syndromes. Adiponectin replacement has not yet been studied in humans, although animal studies suggest that it may also have some benefit by significantly improving insulin sensitivity.
Lipoatrophic Diabetes
Lipoatrophy syndromes comprise a heterogeneous cluster in which the common trait is a lack of fat tissue. The deficiency of adipose tissue can be generalized or partial, and the abnormality may be congenital or acquired. In all of these cases, the metabolic consequences are similar, namely, peripheral insulin resistance and hypertriglyceridemia. (See the images below.)
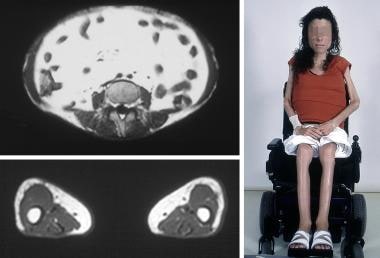 Generalized Lipodystrophy. Congenital generalized lipoatrophy in a 16-year-old girl. In the top left T1-weighted magnetic resonance imaging (MRI) scan, transverse sections of the torso at the fifth lumbar vertebra demonstrate markedly deficient subcutaneous and visceral fat. On the bottom left, transverse sections of the midthigh demonstrate an absence of subcutaneous fat, deep fat, intrafascicular fat, and marrow fat; note light-colored, lipid-filled muscle tissue. Note absence of fat throughout the body in the photograph on the right.
Generalized Lipodystrophy. Congenital generalized lipoatrophy in a 16-year-old girl. In the top left T1-weighted magnetic resonance imaging (MRI) scan, transverse sections of the torso at the fifth lumbar vertebra demonstrate markedly deficient subcutaneous and visceral fat. On the bottom left, transverse sections of the midthigh demonstrate an absence of subcutaneous fat, deep fat, intrafascicular fat, and marrow fat; note light-colored, lipid-filled muscle tissue. Note absence of fat throughout the body in the photograph on the right.
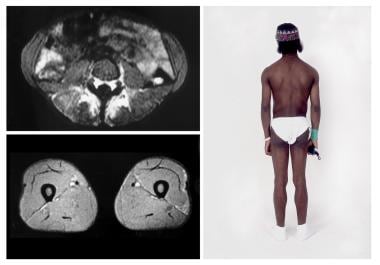
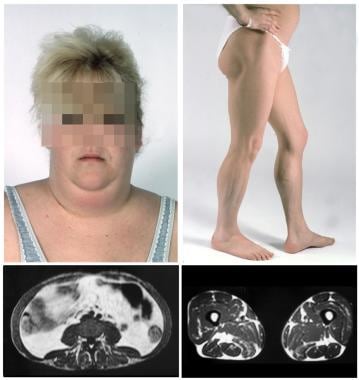 Generalized Lipodystrophy. Dunnigan familial partial lipodystrophy in a 26-year-old woman. Note the increased fat around the face/neck (top left) and deficiency in the gluteal region and lower extremities (top right). T1-weighted magnetic resonance imaging (MRI) scan of transverse sections of the torso at the fifth lumbar vertebra demonstrate markedly deficient subcutaneous fat and increased visceral fat (bottom left). Transverse sections of the midthigh demonstrate absence of subcutaneous fat, with preservation of deep fat, intrafascicular fat, and marrow fat (bottom right).
Generalized Lipodystrophy. Dunnigan familial partial lipodystrophy in a 26-year-old woman. Note the increased fat around the face/neck (top left) and deficiency in the gluteal region and lower extremities (top right). T1-weighted magnetic resonance imaging (MRI) scan of transverse sections of the torso at the fifth lumbar vertebra demonstrate markedly deficient subcutaneous fat and increased visceral fat (bottom left). Transverse sections of the midthigh demonstrate absence of subcutaneous fat, with preservation of deep fat, intrafascicular fat, and marrow fat (bottom right).
In this article, the loss of fat is referred to as lipoatrophy and the abnormal distribution of fat is referred to as lipodystrophy. The term lipoatrophic diabetes refers to diabetes mellitus in association with lipoatrophy. Lipodystrophy encompasses lipoatrophy and other abnormalities of adipose tissue. The focus of this review is on syndromes characterized primarily by adipocyte deficiencies throughout the body.
Another distinction is between syndromes of (1) lipoatrophy, in which an actual insufficiency of adipocytes and/or precursor cells is present and results in metabolic disturbances, and (2) other states of total body fat deficiency, in which the adipocytes are basically normal but are chronically forced to mobilize their stored triglycerides (eg, chronic energy [caloric] depletion, exercise, increased sympathetic drive. [21, 22, 23, 24] In the latter group, the adipocytes are still capable of functioning at a level sufficient to prevent metabolic consequences.
The use of genetic engineering approaches that disturb only triglyceride storage into the adipocytes (eg, by perturbing the insulin receptor specifically in the adipocytes [25] or by disrupting perilipin protein that coats lipid droplets in adipocytes) [26] does not lead to metabolic syndrome.
Perilipin-null mice have a greater lean body mass and are more resistant to diet-induced obesity than wild-type mice, although compared to wild-type mice who weigh over 30 grams, perilipin-null mice who weigh over 30 grams may have an increased tendency to develop glucose intolerance and peripheral insulin resistance. Interestingly, plasma leptin concentrations in perilipin-null mice are greater than expected given the decrease in fat mass. This increased leptin might explain the relative absence of lipoatrophic symptoms, such as severe hyperinsulinemia, elevated blood lipids, fatty liver, and organomegaly, in the perilipin-null mice.
In contrast, the approaches that ablate white adipose tissue do lead to metabolic syndrome, regardless of the strategy. These observations underscore the importance of the adipocyte cell as not only a storage space for triglycerides, but as a fundamental regulator of metabolism. [27]
Etiology and Classification
Lipodystrophies are categorized based on etiology (genetic or acquired) and distribution of lost adipose tissue, affecting the entire body (generalized) or only regions (partial). Three classes of lipodystrophy syndromes are as follows [1] :
-
Congenital lipodystrophy syndromes, including congenital generalized lipoatrophy (CGL) (autosomal recessive; near total absence of body fat, generalized muscularity, metabolic complications) and familial partial lipodystrophy (FPLD) (autosomal dominant; absence of fat in limbs, metabolic complications)
-
Acquired lipodystrophy syndromes, including acquired generalized lipodystrophy (AGL) (near total absence of body fat, metabolic complications) and acquired partial lipodystrophy (APL) (absence of fat in upper body with increased fat in lower body, mild or no metabolic complications), as well as human immunodeficiency virus (HIV)-associated lipodystrophy, regional lipodystrophy, and other acquired lipodystrophy
-
Progeroid and autoinflammatory disorders-associated syndromes
Additional genetic subtypes include SHORT syndrome. [1] (See Table 1 below.)
Other acquired subtypes include a localized lipodystrophy seen in injection drug users. Additionally, aggressive treatment of patients infected with HIV, cause loss of subcutaneous fat from the face, extremities, and trunk [6] ; increased visceral fat, with buffalo hump, [7, 8, 9] accompanied by insulin resistance and hypertriglyceridemia.
An entity exists called focal lipoatrophy, in which the loss of fat involves a single region in the body such as the gluteal area, usually following intramuscular injections, [28] or on the face (ie, Romberg syndrome). [29] Other specific distributions are reported in the literature, and other descriptive terminology is used, including annular or semicircular lipoatrophy [30, 31] (see Localized Lipodystrophy).
Therapy with protein hormones such as insulin [32, 33] and growth hormone [34] also may lead to focal lipoatrophy. Usually, the isolated loss of fat from a limited body region is not associated with metabolic consequences, supporting the hypothesis that a crucial degree of fat loss is required to observe the metabolic abnormalities.
Table 1. Genetic Syndromes of Lipoatrophy (Open Table in a new window)
Syndrome |
Lipoatrophy |
Gene/Locus |
Inheritance |
OMIM* |
Primary Lipoatrophy Syndromes |
||||
Congenital generalized lipoatrophy (Seip-Berardinelli)† |
Generalized See text for details (Congenital generalized lipoatrophy) |
AGPAT2/9q34 seipin/11q13 |
AR |
608594 269700 |
Kobberling-Dunnigan syndrome |
Partial See text for details (Familial partial lipodystrophy) |
1q21-22 Lamin A/C PPAR-gamma AKT2 Others - Unknown |
AD |
151660 604367 164731 |
Others |
Numerous distributions |
Unknown |
AD/AR |
N/A |
Complex Syndrome Associated With Lipoatrophy |
||||
Mandibuloacral dysplasia |
Congenital, partial involving extremities only OR generalized |
Lamin A/C ZMPSTE24 Others-Unknown |
AR |
248370 608612 |
Werner syndrome |
Congenital, partial Involves extremities |
8p12 Werner helicase |
AR |
277700 |
Cockayne syndrome |
Congenital, partial Involves extremities |
5 CSA |
AR |
216400 |
Carbohydrate-deficient glycoprotein syndrome |
Transient, partial Buttocks |
16p.13.3 PMM 1 and 2‡ |
AR |
212065 |
SHORT syndrome |
Congenital, generalized or partial |
Unknown |
AR/AD |
269880 |
AREDYLD§ syndrome |
Generalized, congenital |
Unknown |
– |
207780 |
*Online Mendelian Inheritance of Man; database providing information about genetic syndromes †Evidence for genetic heterogeneity ‡Phosphomannomutase 1 and 2 §Not clear if this is a variation of Berardinelli-Seip syndrome |
||||
Congenital generalized lipoatrophy
Congenital generalized lipoatrophy (CGL), also known as Seip-Berardinelli syndrome, is a genetic disease with heterogeneous causes (see the image below). [35, 36, 37, 38, 39] In this syndrome, children present with a generalized absence of fat within the first year of life. This is followed by insulin resistance, acanthosis nigricans, and diabetes mellitus before adolescence. Hypertriglyceridemia is severe and is accompanied by frequent bouts of pancreatitis. Affected patients have a high basal metabolic rate [40] and an increased appetite. Circulating leptin levels are usually below detection limits. [41, 42] Cardiomyopathy or rhythm disturbances may occur. [1]
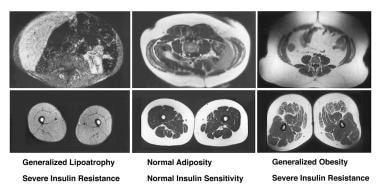 Generalized Lipodystrophy. Clinical spectrum of adiposity. These are T1-weighted magnetic resonance images in which lipid appears white. Transverse sections of the torso are shown at the level of the fifth lumbar vertebra (top panels) and of the midthigh (bottom panels). Note generalized lipoatrophy (top left, bottom left) in a healthy individual with a body mass index (BMI) of 24 kg/m2 (top center, bottom center), and an individual who is obese with a BMI of 38 kg/m2 (top right, bottom right). Note the marked absence of all fat depots in the patient with generalized lipoatrophy, with preservation of marrow fat and a lipid-filled liver. In addition, the bright color of the muscle is indicative of lipid-filled myocytes.
Generalized Lipodystrophy. Clinical spectrum of adiposity. These are T1-weighted magnetic resonance images in which lipid appears white. Transverse sections of the torso are shown at the level of the fifth lumbar vertebra (top panels) and of the midthigh (bottom panels). Note generalized lipoatrophy (top left, bottom left) in a healthy individual with a body mass index (BMI) of 24 kg/m2 (top center, bottom center), and an individual who is obese with a BMI of 38 kg/m2 (top right, bottom right). Note the marked absence of all fat depots in the patient with generalized lipoatrophy, with preservation of marrow fat and a lipid-filled liver. In addition, the bright color of the muscle is indicative of lipid-filled myocytes.
In a cross-sectional study of cardiac autonomic regulation in persons with congenital generalized lipoatrophy, Faria et al found that the persons with congenital generalized lipoatrophy had abnormal autonomic modulation, as demonstrated by an increased heart rate and a pronounced HRV reduction—independent of metabolic and hemodynamic disturbances associated with this form of lipoatrophy. [43] The investigators compared biochemical and physiologic measurements in 18 patients with the condition with those of 19 healthy controls. Blood pressure, plasma glucose, triglyceride, cholesterol, and high-density lipoprotein cholesterol levels were evaluated, along with insulin resistance, left ventricular mass, and 24-hour heart rate variability (HRV). [43]
This syndrome has an autosomal recessive (AR) mode of inheritance and has been described in persons of all ethnic groups.
Initial genetic studies using the candidate gene approach were unsuccessful in identifying the genes responsible for this syndrome. Among the excluded genes were those for PPAR-gamma, beta3-adrenergic receptor, leptin, leptin receptor, and lipoprotein lipase. [44, 45, 46] In subsequent genetic studies, the disease was mapped to band 9q34 in some but not all pedigrees. [47] Later this gene was identified as the AGPAT2 or CGL1 gene. [48] This gene encodes the enzyme AGPAT2, which catalyzes the formation of phosphatidic acid, an important intermediate in the synthesis of triacylglycerol and glycerophospholipids. [49]
Magre et al cloned a second gene responsible for congenital generalized lipoatrophy using a large consanguineous pedigree from Lebanon. This CGL2 gene is located on band 11q13 and is a separate gene from the CGL1 gene located on band 9q34. Magre et al called this new gene seipin as a tribute to Seip, who was the first to describe the gene. [50] Several names have been used for the seipin gene in the published literature, including CGL2, BSCL2, and Gng3lg. [51]
The protein product of the seipin gene is most likely a signaling molecule. It has three trans-membrane domains, and the ligand is not known. The mouse ortholog of the gene is a G-protein–related receptor gene. Contrary to the predictions that prevailed prior to the discovery of this gene, seipin is not abundantly expressed in fat cells. It is expressed predominantly in the central nervous system and especially in the pituitary. Another location where it is expressed in high levels is the testes. As evident from these facts, the discovery of the seipin gene has led to many new questions and is likely to change current views on adipocyte differentiation mechanisms. This exciting discovery also underscores the potential link between the central nervous system and the energy storage sites of the body.
Additional causative genes have been identified including CAV1, PTRF, PCYT1A, PPARγ. [1, 52]
The differential diagnosis of congenital generalized lipoatrophy includes acquired generalized lipoatrophy, leprechaunism, Werner syndrome, pubertal-onset generalized lipodystrophy due to LMNA mutations, and neonatal progeroid syndrome. [5] (See the images below.)
 Generalized Lipodystrophy. Werner syndrome in a 37-year-old woman (left). Clinical features evident include premature aging, alopecia, sclerodermalike changes in the skin, and peripheral lipoatrophy (shown). Insulin-resistant diabetes is an associated feature. On the right is mandibuloacral dysplasia in a 14-year-old girl. This rare recessive syndrome is characterized by acroosteolysis, widened sutures, and hypoplastic mandible (shown) and clavicles (shown). Marked peripheral lipoatrophy and insulin resistance are associated features.
Generalized Lipodystrophy. Werner syndrome in a 37-year-old woman (left). Clinical features evident include premature aging, alopecia, sclerodermalike changes in the skin, and peripheral lipoatrophy (shown). Insulin-resistant diabetes is an associated feature. On the right is mandibuloacral dysplasia in a 14-year-old girl. This rare recessive syndrome is characterized by acroosteolysis, widened sutures, and hypoplastic mandible (shown) and clavicles (shown). Marked peripheral lipoatrophy and insulin resistance are associated features.
 Generalized Lipodystrophy. Acquired generalized lipoatrophy is in the differential diagnosis of congenital generalized lipoatrophy. The patient shown, who had completely normal fat distribution at age 3 years and 8 months (left), acutely lost her body fat with a febrile illness at age 6 years and10 months (right).
Generalized Lipodystrophy. Acquired generalized lipoatrophy is in the differential diagnosis of congenital generalized lipoatrophy. The patient shown, who had completely normal fat distribution at age 3 years and 8 months (left), acutely lost her body fat with a febrile illness at age 6 years and10 months (right).
Other genetic lipoatrophy syndromes
There are autosomal dominant (AD) forms of congenital lipodystrophy (characterized by an absence of fat from the face, upper trunk, arms, and below the knees) associated with a progressive neurodegenerative disorder (characterized by progressive spinocerebellar ataxia, pyramidal weakness and spasticity, and autonomic insufficiency) and congenital cataracts. In this small pedigree, affected individuals also have insulin resistance and dyslipidemia, and both the neurodegenerative disorder and dyslipidemia are more severe in affected female members.
Some unusual congenital disorders, such as vitamin D resistance and persistent müllerian ducts, [53] retinal pigmentation abnormalities [54] and sensorineural deafness, [55] have been reported in association with lipodystrophy in isolated cases. These unusual patients present as pediatric patients or young adults.
Other complex monogenic syndromes are not characterized as primary lipodystrophy syndromes but are associated with abnormal body fat distribution, among other complex abnormalities. Progeria syndromes, such as Werner syndrome (adult progeria syndrome, see first image above), [56] Cockayne syndrome (a juvenile progeria syndrome), [57, 58] carbohydrate-deficient glycoprotein syndrome type 1, [59] SHORT (short stature, hyperextensibility, hernia, ocular depression, Rieger anomaly, and teething delay) syndrome, [60, 61] and mandibuloacral dysplasia [62, 63] [see the image above]), are among such conditions. Acral, renal, and ectodermal dysplasia in association with generalized lipodystrophy (AREDYLD) syndrome [64] probably represents another complex progeria syndrome.
Mandibuloacral dysplasia is another genetic disorder with multisystem involvement and AR inheritance. This extremely rare syndrome is characterized by multiple skeletal abnormalities, acroosteolysis, and joint and skin problems and is associated with lipodystrophy and metabolic abnormalities. [62, 63] Two forms of lipodystrophy have been observed in patients with mandibuloacral dysplasia. [5] Type A involves partial loss of subcutaneous adipose tissue from the extremities. Type B involves a more generalized loss of subcutaneous adipose tissue from the face, trunk, and extremities.
Familial partial lipodystrophy
Also referred to as Kobberling-Dunnigan syndrome, familial partial lipodystrophy (FPLD) or Dunnigan syndrome (see the image below) is inherited in an AD fashion. It is observed mostly in white persons of northern European descent, but pedigrees of persons of Asian descent have also been described. Although the condition is rare, pediatricians may be presented with the question of whether a child of an affected parent also has the disease. Distinguishing affected patients from unaffected patients before the onset of puberty is usually impossible.
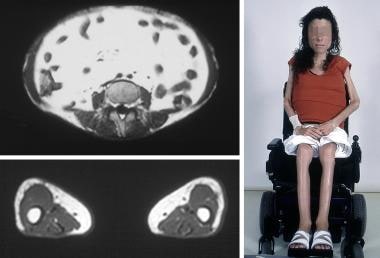 Generalized Lipodystrophy. Congenital generalized lipoatrophy in a 16-year-old girl. In the top left T1-weighted magnetic resonance imaging (MRI) scan, transverse sections of the torso at the fifth lumbar vertebra demonstrate markedly deficient subcutaneous and visceral fat. On the bottom left, transverse sections of the midthigh demonstrate an absence of subcutaneous fat, deep fat, intrafascicular fat, and marrow fat; note light-colored, lipid-filled muscle tissue. Note absence of fat throughout the body in the photograph on the right.
Generalized Lipodystrophy. Congenital generalized lipoatrophy in a 16-year-old girl. In the top left T1-weighted magnetic resonance imaging (MRI) scan, transverse sections of the torso at the fifth lumbar vertebra demonstrate markedly deficient subcutaneous and visceral fat. On the bottom left, transverse sections of the midthigh demonstrate an absence of subcutaneous fat, deep fat, intrafascicular fat, and marrow fat; note light-colored, lipid-filled muscle tissue. Note absence of fat throughout the body in the photograph on the right.
Patients are born with normal fat distribution but notice a loss of subcutaneous fat in the extremities and in some cases also the trunk with early puberty, which produces a muscular appearance with prominent superficial veins. This is followed by increased fat in the face and neck as puberty is completed. [65, 66] The visceral fat and interfascicular intramuscular fat depots are preserved. [47, 67] The Kobberling subtype, sometimes referred to as FPLD1, is characterized by loss of subcutaneous adipose tissue from the extremities only, whereas Dunnigan syndrome, or FPLD2, is characterized by loss of fat from the extremities and trunk.
The diagnosis may be suspected in nonobese individuals who develop early onset diabetes and hypertriglyceridemia, especially if there is significant loss of fat from the extremities and hips. [5] Differential diagnoses for familial partial lipodystrophy include Cushing syndrome, truncal obesity, multiple symmetric lipomatosis secondary to alcohol intake, acquired partial lipodystrophy, and HIV-associated lipodystrophy. [6, 68]
While the disease affects both sexes, the phenotype is much easier to discern in females, leading to ascertainment bias of female probands. Up to one third of affected women may develop acanthosis nigricans, hirsutism, menstrual irregularities, and polycystic ovaries. [5] Overall, female patients develop diabetes and dyslipidemia earlier and more severely. For example, from one case series, affected females develop diabetes approximately 73% of the time and hypertriglyceridemia 90% of the time. In contrast, the incidence is 36% and 45%, respectively, in affected males. These observations are similar to the published observations of another group. [69]
An exciting advance in the understanding of the syndrome has been the discovery that the disease is caused by mutations in the lamin A/C gene (LMNA) located at band 1q21-23. [70, 71, 72, 73, 74] Lamin A and C are alternatively spliced products of the same gene and are ubiquitously, but not equally, expressed. [75] They belong to a family of intermediate filament proteins that form the nuclear matrix, [76, 77] which is located just inside the nuclear membrane. Lamins dimerize and oligomerize within the structure of the nuclear matrix. [77] Developmental regulation of the expression of lamins occurs in humans.
In addition to Dunnigan syndrome/FPLD, two other diseases are associated with mutations in LMNA. The first is Emery-Dreifuss muscular dystrophy, which is a progressive muscular dystrophy of the upper and lower extremity muscles, with prominent contractures of ankles and elbows and cardiac conduction abnormalities. [78, 79] The other is a familial cardiomyopathy associated with conduction abnormalities [80, 81] The degree of overlap between these two diseases and FPLD is a subject of research. In addition, how the mutations in LMNA result in three different diseases and how the mutations in a ubiquitously expressed gene cause various syndromes with a strong regional distribution are questions that remain unanswered.
A third form of familial partial lipodystrophy, FPLD3, was first identified in a patient who developed diabetes mellitus and hypertriglyceridemia at age 32 and loss of fat from the extremities and face at age 50 years. This patient had a mutation in the PPAR-gamma gene, which encodes peroxisome proliferator-activated receptor-gamma, the target of the thiazolidinedione medications used to treat insulin resistant diabetes. [82] Heterozygous mutations in the PPAR-gamma mutation have since been identified in several other patients with FPLD. In these patients, the onset of lipodystrophy occurred as early as the second decade of life. [5] All affected patients had loss of subcutaneous adipose tissue from the distal extremities. The face was spared in some and affected in others.
More recently, a mutation in the AKT2, or protein kinase B, gene has been identified in a patient with FPLD affecting only the extremities.
Acquired lipoatrophy syndromes
Some cases of acquired lipodystrophy are believed to be autoimmune in nature, as suggested by the presence of a population of circulating autoantibodies or an association with another autoimmune disease (eg, juvenile dermatomyositis). (See the image below.) Chronic (>3 mo), generalized inflammation of the subcutaneous tissue, referred to as panniculitis (either clinically or based on biopsy results), has been described as preceding the fat loss in some cases. [83, 84]
 Generalized Lipodystrophy. Loss of muscle and fat tissue in a 19-year-old woman with severe juvenile dermatomyositis and generalized lipodystrophy. A T1-weighted magnetic resonance imaging (MRI) scan of transverse sections of the patient's torso at the fifth lumbar vertebra demonstrates markedly deficient subcutaneous fat and markedly increased visceral fat (top left). Transverse sections of the midthigh demonstrate asymmetrical absence of subcutaneous fat, with preservation of medial subcutaneous fat and marrow fat (bottom left).
Generalized Lipodystrophy. Loss of muscle and fat tissue in a 19-year-old woman with severe juvenile dermatomyositis and generalized lipodystrophy. A T1-weighted magnetic resonance imaging (MRI) scan of transverse sections of the patient's torso at the fifth lumbar vertebra demonstrates markedly deficient subcutaneous fat and markedly increased visceral fat (top left). Transverse sections of the midthigh demonstrate asymmetrical absence of subcutaneous fat, with preservation of medial subcutaneous fat and marrow fat (bottom left).
A portion of patients with acquired lipodystrophy have low C3 levels, [85] and adipsin, a factor produced by fat cells, is thought to be responsible for alternative activation of the complement pathway. In addition, generalized or partial fat loss has been described in association with familial [86] or acquired [87, 88, 89] hypocomplementemia.
A clear association exists between lipodystrophy and juvenile dermatomyositis. [90, 91, 92, 93] These patients typically present before adolescence. The fat loss can be either generalized or partial. Usually, increased visceral fat is present despite very severe peripheral fat loss and a specific asymmetrical pattern of fat loss on the extremities (see the image below).
 Generalized Lipodystrophy. Acquired generalized lipoatrophy is in the differential diagnosis of congenital generalized lipoatrophy. The patient shown, who had completely normal fat distribution at age 3 years and 8 months (left), acutely lost her body fat with a febrile illness at age 6 years and10 months (right).
Generalized Lipodystrophy. Acquired generalized lipoatrophy is in the differential diagnosis of congenital generalized lipoatrophy. The patient shown, who had completely normal fat distribution at age 3 years and 8 months (left), acutely lost her body fat with a febrile illness at age 6 years and10 months (right).
Two specific eponyms are used in the literature to refer to acquired lipodystrophy syndromes, Lawrence syndrome and Barraquer-Simons syndrome. These eponyms are mostly descriptive and do not necessarily indicate diseases caused by a unique etiology. These terms should perhaps be replaced by acquired generalized or acquired partial lipodystrophy, respectively.
Lawrence first described acquired generalized lipoatrophy (also known as Lawrence syndrome) with the onset of the disease during childhood. [94] Additional case reports in the literature indicate that acquired generalized lipoatrophy can present at any age. [95] Lawrence's original report remains an excellent description of generalized lipoatrophy.
Fat loss is usually a remarkable event leading to a dramatic change in physical features. The median time to develop diabetes after loss of fat tissue is approximately 4 years. Both the basal metabolic rate and hepatic glucose output are increased. While these patients are known to lack fully differentiated adipocytes, whether they also lack adipocyte precursors remains unclear. [96] Patients with this type of lipodystrophy may have very severe fat loss, including retro-orbital fat and supportive fat in their hands, feet, and genital area. Bone marrow fat is lost in some cases, but preserved in others.
The case reports that refer to Barraquer-Simons (or acquired partial lipodystrophy) syndrome describe a wide range of variation with few shared features. Patients are usually women in their second or third decade of life who also have well-described autoimmune disorders such as scleroderma or glomerulonephritis presenting with partial fat loss. [97, 98, 99] Fat loss usually starts in the face and descends to the gluteal line. Usually, increased adiposity is present in unaffected fat depots (lower extremities). The prevalence rate of diabetes and hypertriglyceridemia is approximately 50% in these cases and seems to cosegregate with lower total body fat in this series.
Other causes of acquired lipodystrophy
Some patients who are infected with HIV and are undergoing aggressive treatment, particularly with protease inhibitors, develop a partial lipoatrophy characterized by loss of subcutaneous fat from the face, extremities, and trunk. [6] In contrast, visceral fat increases, and a buffalo hump similar to that observed in persons with Cushing syndrome develops. [7, 8, 9] This is accompanied by the development of insulin resistance and hypertriglyceridemia. The changes in body composition and metabolic parameters are usually apparent within 3-6 months of therapy, and the onset is usually quicker when more than one protease inhibitor is used. The syndrome is recognized in persons of both sexes and in pediatric and adult patients.
The reason why patients with HIV infection who are undergoing treatment develop this characteristic phenotype remains unknown. One hypothesis is that an aspartyl protease (like the HIV protease) may be important in the differentiation of adipocytes. In support of this hypothesis, several groups reported that protease inhibitors blocked preadipocyte differentiation in vitro. [100, 101] Interestingly, some groups reported the development of a similar phenotype when patients infected with HIV were treated aggressively with antiretroviral agents other than protease inhibitors, including nucleoside analogues, [102, 103, 103] This suggests that the lipodystrophy may be related to aggressively treated HIV infection rather than to a specific therapy. [103, 104]
Further details about some specific forms of lipodystrophy can be found elsewhere (see Acquired Partial Lipodystrophy, Lipodystrophy in HIV, and Progressive Lipodystrophy).
Presentation and Diagnosis
Diagnosis is based on history, physical examination, body composition, and metabolic status. [3] (See Table 2 below.)
In general, the more severe the lack of fat, the more severe the metabolic abnormalities. Circulating free fatty acid levels are increased in most patients studied at the US National Institutes of Health. Because of the relative paucity of adipose tissue, triglycerides accumulate excessively in multiple locations, most notably in the liver and in the muscles.
In addition, the respiratory quotient (RQ) has been observed to be elevated in patients with lipoatrophy/lipodystrophy. The RQ is the ratio of carbon dioxide production to oxygen consumption and reflects the relative contributions of carbohydrates and fat in providing fuel for metabolism. The elevated RQ suggests that either the rate of fat oxidation is decreased or the rate of lipogenesis is increased; both of which might contribute to the observed elevation in the levels of free fatty acids and triglycerides. [105]
Table 2. Characteristics of Patients With Generalized and Partial Lipoatrophy (Open Table in a new window)
General Characteristics |
Generalized |
Partial |
|
Male/female |
2/8 |
4/23 |
|
Age range, y |
6-19 |
26-65 |
|
Genetic/other |
4/6 |
10/17 |
|
Clinical Characteristics |
|||
Diabetes/IGT*/IR† |
9/1/0 |
15/5/3 |
|
Acanthosis nigricans, % |
70 |
56 |
|
Hyperandrogenism, % |
50 |
70 |
|
Central hypogonadism, % |
50 |
0 |
|
NASH, % |
70 |
33 |
|
Laboratory Characteristics |
Reference Range |
||
HbA1c, % |
9.9 ±3.5 |
7.2 ±0.8 |
< 6.2 |
Triglycerides‡, mg/dL |
2015 ±1463 |
426 ±164 |
35-155 |
Free fatty acids, µmol/L |
926 ±156 |
693 ±115 |
50-550 |
HDL cholesterol§, mg/dL |
21.4 ±10.3 |
22.7 ±11.9 |
35-85 |
Leptin||, ng/mL |
1.8 ±1.0 |
10.5 ±6.3 |
Variable |
Body fat by DEXA¶, % |
7.7 ±2.6 |
23.8 ±2.5 |
Variable |
*Impaired glucose tolerance †Insulin resistance ‡Conversion factor to mmol/L: 0.01129X §Conversion factor to mmol/L: 0.02586X ||Conversion factor to nmol/L: 0.08X ¶Dual-energy x-ray absorptiometry |
|||
Patients with congenital generalized lipoatrophy present with generalized absence of fat tissue within the first year of life. The musculature is typically well-defined with prominent superficial veins due to the paucity of adipose tissue. [5] Severe hypertriglyceridemia may be present early on and result in eruptive xanthomas and recurrent pancreatitis. Insulin resistance is also present early on and acanthosis nigricans and type 2 diabetes usually occurs by adolescence.
The accumulation of triglycerides in hepatocytes may somehow cause the injury associated with nonalcoholic steatohepatitis (NASH). [106] NASH is observed in approximately one third of patients with lipoatrophy and may progress to end-stage liver failure with childhood death from bleeding esophageal varices. The insulin resistance leads to hyperinsulinemia, and clinical features of hyperinsulinemia (eg, acanthosis nigricans, hyperandrogenism in female patients) are common.
Patients with the early-onset hyperinsulinemia in combination with congenital generalized lipoatrophy develop acromegaloid features (large hands, feet, and jaw) with soft tissue hyperplasia, somatomegaly, and bony abnormalities. This is believed to be caused by insulin cross-reacting with the IGF-1 receptor. The kidneys may also be affected and renal failure is a common cause of death. Hypertrophic cardiomyopathy and mild intellectual disability may also occur in some forms of congenital lipoatrophy. [5]
Another notable finding in patients who are the most severely fat-deficient is food-seeking behavior. They may consume large amounts of food (similar to patients with bulimia) and may have the urge to eat frequently. They have low levels of circulating leptin, which may contribute to their increased appetite.
Females with congenital lipoatrophy may exhibit clitoromegaly, hirsutism, or both at birth. The hirsutism usually increases with age. Reproductive abnormalities are common. Some women have hypogonadotropic amenorrhea, probably due to leptin deficiency. Many have a form of polycystic ovary syndrome, with irregular or infrequent menstrual cycles, hyperandrogenism, and ovarian cysts. [5] Affected men usually have normal reproductive function.
Acquired generalized lipoatrophy presents with widespread loss of adipose tissue in persons of any age. It has been reported to occur in persons as old as 74 years. [95] Acquired forms of lipodystrophy are typically preceded by an illness, often an infection. A female preponderance appears to exist. Many of the same metabolic abnormalities that occur in the congenital lipodystrophies are also found in the acquired forms of generalized lipoatrophy, including insulin resistance, diabetes mellitus, hypertriglyceridemia, hypermetabolism, and low leptin levels. Mild hirsutism, prominent musculature and superficial veins, acanthosis nigricans, hepatomegaly and cirrhosis may also be present. Autoimmune disorders are common. Some patients may have an increased susceptibility to infection due to C3 deficiency.
Treatment
Currently, there is no drug that effectively cures lipodystrophy. [2, 3] Multidisciplinary management is essential for treatment of lipodystrophy syndromes, including management of metabolic derangements, use of dietary measures, and physical exercise. [2, 3]
The clinical problems requiring treatment in lipoatrophy syndromes are diabetes and hypertriglyceridemia; antidiabetic and antidyslipidemia agents are used in the management of these conditions. Although several classes of antidiabetic drugs are marketed in the United States, achieving good glycemic control (glycated hemoglobin < 6.5%) is difficult for most patients with lipoatrophic diabetes.
See also the Guidelines section.
Leptin analogs
In February 2014, the FDA approved metreleptin (Myalept), a recombinant leptin analog, as replacement therapy to treat the complications of leptin deficiency, in addition to diet, for congenital or acquired generalized lipodystrophy in children and adults. [107, 108] The approval was based on results from a National Institutes of Health open-label, single-arm study of 48 patients with congenital or acquired generalized lipodystrophy who also had diabetes mellitus, hypertriglyceridemia, and/or elevated levels of fasting insulin, in which metreleptin reduced levels of HbA1C, fasting glucose, and triglycerides. [107, 108, 109] Hypoglycemia, headache, abdominal pain, decreased weight were the most common side effects reported. [107] In a study monitoring patients over one year, metreleptin improved insulin sensitivity and increased insulin secretion rate in response to glucose infusion, and these benefits were sustained for the duration of the study. [110]
Clinicians should use caution in considering metreleptin therapy in patients with significant hematologic abnormalities and/or acquired generalized lipodystrophy. [107, 108, 111, 112] In addition, metreleptin is contraindicated in patients with general obesity, and it is not approved for the treatment of HIV-related lipodystrophy or metabolic disease (including diabetes and hypertriglyceridemia) without concurrent evidence of generalized lipodystrophy. [3, 107, 108]
Metreleptin is available only through the Myalept Risk Evaluation and Mitigation Strategy (REMS) Program due to the risk associated with the development of neutralizing antibodies and lymphoma; prescribers and pharmacies must undergo certification and fulfill documentation and/or training requirements. [107, 108, 113, 114] Postmarketing studies are ongoing, including a long-term prospective observational study, to assess for immunogenicity (final report estimated in December 2022), and (2) an assessment and analysis of spontaneous reports of potential serious risks related to the use of metreleptin (study completion around May 2024; final report submission around July 2024).
The following are three trials actively recruiting:
Insulin
Because of their extreme insulin resistance, extremely high doses (eg, >1000 U/d) are often necessary in patients with various syndromes of lipoatrophy. [10] The volume of injections is more difficult to tolerate for younger patients. Nevertheless, insulin remains the only approved medication for the treatment of children with diabetes.
Insulin secretagogues
The principal mechanism of action for this class of drugs is to promote insulin secretion by beta cells. [115] Because patients with isolated insulin resistance may not have an independent defect in insulin secretion, sulfonylureas are frequently ineffective in patients with lipoatrophic diabetes.
Metformin
Metformin primarily works by inhibiting hepatic glucose output. This drug may help decrease insulin requirements in some patients with lipoatrophy/lipodystrophy. To this author's knowledge, no systematic trials are investigating the efficacy of this drug in patients with lipoatrophy/lipodystrophy. Metformin is approved by the US Food and Drug Administration (FDA) for the treatment of type 2 diabetes in adults and children older than 10 years. Use of metformin in younger children is best administered by clinicians who have prior experience with treatment with this drug, ideally in facilities specialized in treating children with unusual forms of diabetes.
Thiazolidinediones
Guidelines recommend that thiazolidinediones be used with caution in generalized lipodystrophy. [1]
Members of this class of medications are agonists of PPAR-gamma, thereby stimulating adipocyte differentiation. [116] In vivo, this class of drugs functions as insulin sensitizers, and they increase insulin-stimulated glucose uptake by the muscle. [117, 118] These effects of thiazolidinedione compounds seem ideally suited to treat the problems encountered in lipoatrophy/lipodystrophy syndromes. In addition, troglitazone has exerted favorable effects in an animal model of lipoatrophy. [119] Several case reports have suggested a beneficial effect from treatment with rosiglitazone or pioglitazone on fat distribution in acquired partial lipodystrophy; however, preferential fat gain was in the lower body.
The Food and Drug Administration issued an alert on May 21, 2007, to patients and health care professionals warning that rosiglitazone could potentially cause an increased risk of myocardial infarction (MI) and heart-related deaths. A thiazolidinedione derivative, rosiglitazone is an antidiabetic agent that improves glycemic control by improving insulin sensitivity. The drug is highly selective and is a potent agonist for PPAR-gamma. Activation of PPAR-gamma receptors regulates insulin-responsive gene transcription involved in glucose production, transport, and utilization, thereby reducing blood glucose concentrations and hyperinsulinemia. Potent PPAR-gamma agonists have been shown to increase the incidence of edema.
In September 2010, the FDA required a restricted access program to be developed for rosiglitazone under a risk evaluation and mitigation strategy (REMS). Patients currently taking rosiglitazone and benefiting from the drug were able to continue if they choose to do so. Rosiglitazone was only to be available to new patients if they were unable to achieve glucose control on other medications and were unable to or did not wish to take pioglitazone, the only other thiazolidinedione.
However, in 2013, the FDA removed some of the 2010 prescribing and dispensing restrictions for diabetes drugs that contain rosiglitazone (eg, Avandia, Avandamet, Avandaryl) on the basis of data that did not show an increased risk of heart attack versus metformin and sulfonylurea. In 2015, after analyzing data from the large-scale phase III trial (Rosiglitazone Evaluated for Cardiac Outcomes and Regulation of Glycaemia in Diabetes [RECORD] trial) to study the cardiovascular outcomes of rosiglitazone relative to placebo, the FDA completely eliminated REMS for rosiglitazone-containing diabetes drugs, indicating it was no longer necessary to ensure the benefits of these drugs benefits outweighed their risks as there did not appear to be an increased risk of myocardial infarction associated with rosiglitazone use. [134]
For more information, see the FDA’s Safety Communication on Avandia here, here, here, and here. Additionally, responses to the controversy, including the following articles, from Medscape Medical News):
Insulin-like growth factor 1 (IGF-1)
IGF-1 promotes cell growth and differentiation, but produces a glucose-lowering effect similar to insulin at higher concentrations. [2] However, IGF-1 doesn't affect enhanced appetite and has the potential risk of exacerbating lipodystrophy syndromes-associated cardiomyopathy (due to positive effects on cell growth).
Treatment of dyslipidemia in lipoatrophic diabetes
The dyslipidemia of severe lipoatrophy is difficult to treat with currently available therapeutic interventions. This problem causes significant morbidity and mortality. Patients with triglyceride levels greater than 1000 mg/dL are at risk of developing acute pancreatitis. Recurrent episodes lead to pancreatic insufficiency. Chronically elevated triglyceride levels in the setting of hyperinsulinemia and low high-density lipoprotein (HDL) levels increase the predisposition for coronary artery disease. Severely elevated triglyceride levels may lead to painful cutaneous eruptive xanthomata.
Troglitazone is remarkable in its ability to improve hypertriglyceridemia in addition to improving glycemia. This author prefers to use fibrates and statins as opposed to niacin because of severe insulin resistance. These two classes may need to be used in combination, with careful monitoring for adverse effects. Again, the pediatric experience with these medications is extremely limited. Limitation of energy (caloric) intake may be useful for short-term results, but continuing this for long-term treatment is not possible. Medium-chain triglycerides and fish oil have not been tested in a systematic fashion, but they may prove useful. This author has attempted to use intestinal lipase inhibitors in a few severely affected pediatric patients, with some positive results. Another study showed marked improvement with intensive plasma exchange therapy in a 15-year-old girl with acquired generalized lipoatrophy and severe hypertriglyceridemia that was refractory to medical therapy. [120]
In women with lipoatrophy syndromes, oral estrogens should be avoided as they can exacerbate the hypertriglyceridemia and result in acute pancreatitis. [5]
Role of diet and lifestyle
There is no evidence supporting the use of a specific diet for lipodystrophy. [5] Total calories, saturated fat, and simple carbohydrates are typically restricted. A low fat diet is especially important if hypertriglyceridemia is present. In children, care must be taken to ensure that the energy intake is sufficient for normal growth and development. Alcohol should be avoided in patients with hypertriglyceridemia and fatty liver. Regular exercise should be encouraged to improve metabolic status. Lifestyle modifications alone may not be sufficient and may need to be implemented along with pharmacotherapy.
Guidelines
2021 Japan Endocrine Society (JES) guidelines
The JES released their practice guideline for lipodystrophy syndromes in September 2021. [2] Select recommendations are outlined below.
Diagnosis
Suspect and evaluate the extent of lipodystrophy (generalized or partial, regional) when patients are examined who have severe insulin resistance, diabetes, hypertriglyceridemia, and metabolic disorders (eg, nonalcoholic fatty liver disease [NAFLD]).
Rule out other conditions that can cause leanness and weight loss. These diseases include but are not limited to anorexia nervosa, poorly controlled diabetes, hyperthyroidism, adrenocortical insufficiency, cachexia of cancer, malabsorption syndrome, and severe infections.
Evaluate the possibility of progeroid and autoinflammatory syndrome on the basis of the patient's physical features.
Evaluate the time of onset (eg, observed at birth or from infancy, childhood, adolescence) as well as the extent of lipodystrophy using physical and imaging examinations.
A mutational analysis of causative genes is typically needed for a definitive diagnosis (eg, CGL and FPLD for the diagnosis of congenital lipodystrophy syndromes). Other useful diagnostic studies include levels of plasma leptin and whole-body T1-weighted magnetic resonance imaging (MRI).
Management
No curative treatment currently exists for lipodystrophy syndromes. The goal of therapeutic strategies is primarily to ameliorate metabolic derangements or conditions that arise from lipodystrophy. If needed, consider plastic surgical approaches.
The basis for managing lipodystrophy-related metabolic derangements (eg, insulin resistance, diabetes, hypertriglyceridemia, fatty liver disease) is diet and exercise therapy, and, potentially, pharmacotherapy such as antidiabetic and antidyslipidemia agents (eg, metreleptin/leptin replacement therapy, insulin secretagogues, fibrates, statins, eicosapentaenoic acid, insulinlike growth factor 1).
Unfortunately, no cure yet exists for adipose tissue atrophy. Although thiazolidinedione does induce hypertrophy of adipose tissue in nonatrophic anatomic regions, the atrophied body areas remain unaffected. However, in acquired lipodystrophy syndrome, strategies aimed at the causative condition, subcutaneous panniculitis, or autoimmune disease may be effective.
Plastic surgery approaches include facioplasty via autologous transplantation of subcutaneous fat tissue free flap or implantation of silicone or other implants that substitute for fat tissue. Soft-tissue expansion with adipose tissue-derived stem cells remain under investigation, with its safety and efficacy yet to be determined.
2016 Multisociety consensus guidelines
In 2016, consensus guidelines for the diagnosis and management of Lipodystrophy Syndromes was published and endorsed by multiple societies globally including the Pediatric Endocrine Society, American Diabetes Association, American Association of Clinical Endocrinologists, Endocrine Society, Japanese Society for Pediatric Endocrinology, Australasian Pediatric Endocrine Group, European Society for Pediatric Endocrinology, Asia Pacific Pediatric Endocrine Society, African Society for Pediatric and Adolescent Endocrinology, and International Society for Pediatric and Adolescent Diabetes. [1]
Diagnosis
Diagnostic criteria for lipodystrophy have not been established and no defined serum lipid levels establish or exclude the diagnosis. The guidelines include a diagnostic algorithm along with the following recommendations [1] :
-
Base diagnosis on history, physical examination, body composition, and metabolic status. (Class I, Level B)
-
Genetic testing to confirm diagnosis is helpful in suspected genetic subtypes. (Class I, Level A)
-
Genetic testing should be considered in at-risk family members. (Class IIa, Level C)
-
Serum complement levels and autoantibodies may support diagnosis of acquired lipodystrophy syndromes. (Class IIa, Level B)
Screening for comorbidities
Following diagnosis, the guidelines recommend all patients be screened for diabetes, dyslipidemia, liver disease, and cardiovascular and reproductive dysfunction. Recommended timing for screening are as follows [1] :
-
Diabetes: Annually
-
Triglycerides: At least annually or if abdominal pain or xanthomata are present
-
Fasting lipid panel: Annually after age 10
-
Gonadal steroids, gonadotropins, and pelvic ultrasonography: As clinically indicated
-
Pubertal staging: Annually in children
-
Blood pressure: At least annually
-
Electrocardiogram and echocardiogram: Annually in CGL; as clinically indicated in AGL
-
Urine protein: Annually
-
Alanine aminotransferase and aspartate aminotransferase: Annually
-
Liver ultrasound: As clinically indicated
-
Liver biopsy: As clinically indicated
The guidelines note that patients with CGL are at high risk for early cirrhosis, and those with AGL may have autoimmune hepatitis in addition to non-alcoholic fatter liver (NAFL). [1]
Diet and exercise
There is no cure of lipodystrophy and the goal of therapy is to prevent and treat comorbidities. A diet consisting of 50–60% carbohydrate, 20–30% fat, and approximately 20% protein is recommended with restriction of simple sugars. High-fiber complex carbohydrates should be distributed evenly among meals and snacks and consumed with protein or fat. Dietary fat should be primarily cis-monounsaturated fats and long-chain omega-3 fatty acids. The guidelines include the following additional treatment recommendations10:
-
Energy-restricted diets improve metabolic abnormalities and may be appropriate in adults. (Class I, Level C)
-
Very-low-fat diets should be used in chylomicronemia-induced acute pancreatitis. (Class I, Level C)
-
A dietician should be consulted for specialized dietary needs, especially in infants and young children. Overfeeding should be avoided. (Class IIa, Level C)
-
Medium-chain triglyceride oil formulas can provide energy and reduce triglycerides in infants. (Class IIa, Level C)
-
Exercise should be encouraged in the absence of specific contraindications. (Class IIa, Level C)
Medications
The guidelines consider metreleptin (with diet) as a first-line treatment for metabolic and endocrine abnormalities in generalized lipodystrophies. A dosing algorithm is included in the published guidelines. Additional recommendation for medical management include [1] :
-
Metreleptin may be considered for prevention of metabolic and endocrine comorbidities in children. (Class IIb, Level C)
-
Metformin is a first-line agent for diabetes and insulin resistance. (Class IIa, Level C)
-
In some patients, concentrated preparations and high-doses of insulin may be required to treat hyperglycemia. (Class IIa, Level C)
-
Thiazolidinediones should be used with caution in generalized lipodystrophy. (Class IIb, Level B)
-
Statins should be used concomitantly with lifestyle modification. (Class 1, Level C)
-
Fibrates and/or long-chain omega-3 fatty acids should be used for triglycerides >500 mg/dL and may be considered for triglycerides >200 mg/dL. (Class IIb, Level C)
-
Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers are first-line treatments for hypertension in patients with diabetes. (Class IIa, Level C)
Cosmetic treatments
Because changes in physical appearance can cause psychological distress and physical discomfort, the guidelines recommend that patients be assessed for distress related to lipodystrophy and referred to mental health professionals and/or plastic surgeons as needed. [1]
Contraception and pregnancy
Oral estrogens are contraindicated due to the risk of risk of severe hypertriglyceridemia and acute pancreatitis. The guidelines recommend progestin or non-hormonal contraceptives. Transdermal estrogens has less hepatic exposure and may be used if estrogen replacement is needed. [1]
During pregnancy, management of women with extreme insulin resistance is difficult. Metreleptin withdrawal has been associated with rebound hypertriglyceridemia with increased risk for pancreatitis, endangering both mother and fetus. The guidelines recommend women receive prenatal care from an obstetrician experienced in managing diabetes and a physician experienced in managing lipodystrophy. Additionally, clinicians may consider continuing metreleptin if withdrawal would harm the mother and fetus and the patient chooses to continue with the understanding that the effects of metreleptin on the fetus are unknown. [1]
-
Generalized Lipodystrophy. Clinical spectrum of adiposity. These are T1-weighted magnetic resonance images in which lipid appears white. Transverse sections of the torso are shown at the level of the fifth lumbar vertebra (top panels) and of the midthigh (bottom panels). Note generalized lipoatrophy (top left, bottom left) in a healthy individual with a body mass index (BMI) of 24 kg/m2 (top center, bottom center), and an individual who is obese with a BMI of 38 kg/m2 (top right, bottom right). Note the marked absence of all fat depots in the patient with generalized lipoatrophy, with preservation of marrow fat and a lipid-filled liver. In addition, the bright color of the muscle is indicative of lipid-filled myocytes.
-
Generalized Lipodystrophy. Congenital generalized lipoatrophy in a 16-year-old girl. In the top left T1-weighted magnetic resonance imaging (MRI) scan, transverse sections of the torso at the fifth lumbar vertebra demonstrate markedly deficient subcutaneous and visceral fat. On the bottom left, transverse sections of the midthigh demonstrate an absence of subcutaneous fat, deep fat, intrafascicular fat, and marrow fat; note light-colored, lipid-filled muscle tissue. Note absence of fat throughout the body in the photograph on the right.
-
Generalized Lipodystrophy. Dunnigan familial partial lipodystrophy in a 26-year-old woman. Note the increased fat around the face/neck (top left) and deficiency in the gluteal region and lower extremities (top right). T1-weighted magnetic resonance imaging (MRI) scan of transverse sections of the torso at the fifth lumbar vertebra demonstrate markedly deficient subcutaneous fat and increased visceral fat (bottom left). Transverse sections of the midthigh demonstrate absence of subcutaneous fat, with preservation of deep fat, intrafascicular fat, and marrow fat (bottom right).
-
Generalized Lipodystrophy. Werner syndrome in a 37-year-old woman (left). Clinical features evident include premature aging, alopecia, sclerodermalike changes in the skin, and peripheral lipoatrophy (shown). Insulin-resistant diabetes is an associated feature. On the right is mandibuloacral dysplasia in a 14-year-old girl. This rare recessive syndrome is characterized by acroosteolysis, widened sutures, and hypoplastic mandible (shown) and clavicles (shown). Marked peripheral lipoatrophy and insulin resistance are associated features.
-
Generalized Lipodystrophy. Acquired generalized lipoatrophy is in the differential diagnosis of congenital generalized lipoatrophy. The patient shown, who had completely normal fat distribution at age 3 years and 8 months (left), acutely lost her body fat with a febrile illness at age 6 years and10 months (right).
-
Generalized Lipodystrophy. Loss of muscle and fat tissue in a 19-year-old woman with severe juvenile dermatomyositis and generalized lipodystrophy. A T1-weighted magnetic resonance imaging (MRI) scan of transverse sections of the patient's torso at the fifth lumbar vertebra demonstrates markedly deficient subcutaneous fat and markedly increased visceral fat (top left). Transverse sections of the midthigh demonstrate asymmetrical absence of subcutaneous fat, with preservation of medial subcutaneous fat and marrow fat (bottom left).






