Background
To define abnormal labor, a definition of normal labor must be understood and accepted. Normal labor is defined as uterine contractions that result in progressive dilation and effacement of the cervix. By following thousands of labors resulting in uncomplicated vaginal deliveries, time limits and progress milestones have been identified that define normal labor. Failure to meet these milestones defines abnormal labor, which suggests an increased risk of an unfavorable outcome. Thus, abnormal labor alerts the obstetrician to consider alternative methods for a successful delivery that minimize risks to both the mother and the infant.
Dystocia of labor is defined as difficult labor or abnormally slow progress of labor. Other terms that are often used interchangeably with dystocia are dysfunctional labor, failure to progress (lack of progressive cervical dilatation or lack of descent), and cephalopelvic disproportion (CPD).
Friedman's original research in 1955 defined the following three stages of labor [1] :
The first stage starts with uterine contractions leading to complete cervical dilation and is divided into latent and active phases. In the latent phase, irregular uterine contractions occur with slow and gradual cervical effacement and dilation. The active phase is demonstrated by an increased rate of cervical dilation and fetal descent. The active phase usually starts at 3-4 cm cervical dilation and is subdivided into the acceleration, maximum slope, and deceleration phases.
The second stage of labor is defined as complete dilation of the cervix to the delivery of the infant.
The third stage of labor involves delivery of the placenta.
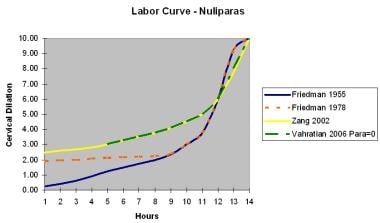
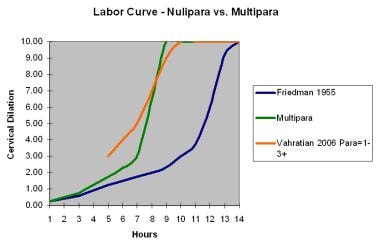
See images below for the normal labor curves of both nulliparas and multiparas. The following table shows abnormal labor indicators.
Table. Abnormal Labor Indicators (Open Table in a new window)
Indication |
Nullipara |
Multipara |
Prolonged latent phase |
>20 h |
>14 h |
Average second stage |
50 min |
20 min |
Prolonged second stage without (with) epidural |
>2 h (>3 h) |
>1 h (>2 h) |
Protracted dilation |
< 1.2 cm/h |
< 1.5 cm/h |
Protracted descent |
< 1 cm/h |
< 2 cm/h |
Arrest of dilation* |
>2 h |
>2 h |
Arrest of descent* |
>2 h |
>1 h |
Prolonged third stage |
>30 min |
>30 min |
*Adequate contractions >200 Montevideo units [MVU] per 10 minutes for 2 hours. (Please refer to the Pathophysiology for information regarding adequate contractions.) |
||
Abnormal labor constitutes any findings that fall outside the accepted normal labor curve. However, the authors hesitate to apply the diagnosis of abnormal labor during the latent phase because it is easy to confuse prodromal contractions for latent labor. In addition, the original labor curve, as defined by Friedman, may not be completely applicable today. [2, 3, 4, 5]
Contemporary practice with supporting data suggest that the duration of labor appears longer today than in the past. For both nulliparous and multiparous women, labor may take longer than 6 hours to progress from 4 cm to 5 cm and longer than 3 hours to progress from 5 cm to 6 cm of dilation. Cervical dilation of 6 cm appears to be a better landmark for the start of the active phase. The 95th percentile for duration of the second stage in a nulliparous woman with conduction anesthesia is closer to 4 hours. [6] Note the charts below.
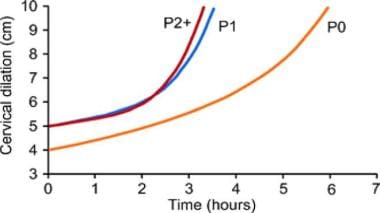 Average labor curves by parity in singleton term pregnancies with spontaneous onset of labor. Reprinted from Seminars in Perinatology, Vol 36(5), El-Sayed YY, Diagnosis and Management of Arrest Disorders: Duration to Wait, pgs 374-8, Oct 2012, with permission from Elsevier.
Average labor curves by parity in singleton term pregnancies with spontaneous onset of labor. Reprinted from Seminars in Perinatology, Vol 36(5), El-Sayed YY, Diagnosis and Management of Arrest Disorders: Duration to Wait, pgs 374-8, Oct 2012, with permission from Elsevier.
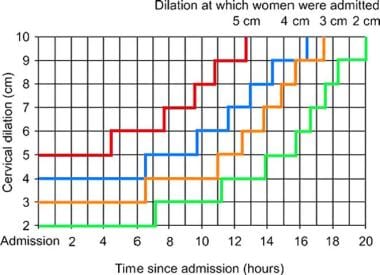 The 95th percentiles of cumulative duration of labor from admission among singleton term nulliparous women with spontaneous onset of labor, vaginal delivery, and normal neonatal outcomes. Reprinted from Seminars in Perinatology, Vol 36(5), El-Sayed YY, Diagnosis and Management of Arrest Disorders: Duration to Wait, pgs 374-8, Oct 2012, with permission from Elsevier.
The 95th percentiles of cumulative duration of labor from admission among singleton term nulliparous women with spontaneous onset of labor, vaginal delivery, and normal neonatal outcomes. Reprinted from Seminars in Perinatology, Vol 36(5), El-Sayed YY, Diagnosis and Management of Arrest Disorders: Duration to Wait, pgs 374-8, Oct 2012, with permission from Elsevier.
First stage of labor
As stated above, first stage of labor is divided into latent and active phases. According to Friedman et al, latent stage considered to be prolonged if takes >20 hours for nulliparous women and >14 hours for multiparous women. However, prolonged latent phase does not usually lead to any clinically significant adverse events for mother or the infant. Therefore, diagnosis of abnormal labor during the latent phase is uncommon and is not relevant for clinical practice.
Around the time uterine contractions cause the cervix to become 3-4 cm dilated, the patient usually enters the active phase of the first stage of labor, according to the traditional definition. Abnormalities of cervical dilation (protracted dilation and arrest of dilation) as well as descent abnormalities (protracted descent and arrest of descent) as described historically are outlined in the Table above.
Both American College of Obstetrics and Gynecology (ACOG) and the Consortium on Safe Labor have proposed extending the minimum period before diagnosing active-phase arrest. The Consortium on Safe Labor defines 6 hours as the 95th percentile of time to go from 4 cm to 5 cm dilation, with the active phase defined as beginning at 6 cm (instead of 4 cm). According to this study, the 95th percentile of rate of dilation in active phase is 0.5 cm/hr to 0.7 cm/hr for nulliparous women and from 0.5 cm/h to 1.3cm/hr for multiparous women. [7] ACOG has also stated that extending the time from 2 to 4 hours with oxytocin augmentation appears effective. Irrespective of the duration, maternal and fetal well-being status must be confirmed. In another study it was found that extending oxytocin augmentation for an additional 4 hours, up to 8 hours total, in patients who were dilated at least 3cm and had unsatisfactory progress resulted in a greater number of vaginal deliveries (38% delivered vaginally) without any evidence of fetal compromise. [8]
According to the most recent evidence, arrest of labor in the first stage should be defined as more than or equal to 6cm dilation with ruptured membranes and one of the following: 4 hours or more of adequate contractions (>200 MVU) or 6 hours or more of inadequate contractions and no cervical change. [9]
The maternal risk of a first stage greater than the 95th percentile (>30 h) is associated with a higher cesarean delivery rate (adjusted odds ratio [aOR]: 2.28) and chorioamnionitis (aOR: 1.58). The neonatal risk is associated with a higher incidence of neonatal ICU admissions in the absence of any other of the major morbidities (aOR: 1.53). [6] These results were again confirmed by another study, which established that prolonged first stage of labor lead to increased risks of a prolonged second stage, maternal fever, shoulder dystocia, and admission to a level 2-3 nursery [10]
Second stage of labor
The Consortium on Safe Labor also addressed the 95th percentile for the second stage for nulliparous women; it was 2.8 hours (168 min) without regional anesthesia and 3.6 hours (216 min) with regional anesthesia. For multiparous women, the 95th percentiles for second-stage duration with and without regional anesthesia remained around 2 hours and 1 hour, respectively. [6, 7] However, other studies demonstrate the risks of both maternal and perinatal adverse outcomes rising with increased duration of the second stage, particularly for durations longer than 3 hours in nulliparous women and 2 hours in multiparous women. [11] One study found that if nulliparous women delivered after prolonged second stage, they were twice as likely to have operative vaginal delivery, three times as likely to develop chorioamnionitis, have higher odds of having episiotomy and 3rd or 4th degree lacerations, and one day longer median hospital stay. [12] .Thus, careful clinical assessment of fetal and maternal well-being must be confirmed when extending the duration of the first and second stages of labor.
Third stage of labor
The third stage of labor is the time from delivery of the infant to placental delivery. Historically, the duration of a normal third stage of labor was defined as less than 30min. This threshold was established by the study conducted by Combs et al. in 1991, in which 75% of placentas were delivered by 10 minutes and maternal morbidity and mortality increased if the third stage was increased beyond 30 min. However, a recently published article by Frolova et al, puts this definition into a question. In this study, the researchers found that in a modern cohort, 90% of placentas are delivered within 10 minutes and the risk of postpartum hemorrhage almost doubles by the time the duration of third stage reaches twenty minutes. [13] Therefore, the traditional definition of prolonged third stage being >30 min, may be outdated and in need of revision.
Pathophysiology
In general, abnormal labor is the result of problems with one of the following three P' s:
-
Passenger (infant size, fetal presentation [occiput anterior, posterior, or transverse])
-
Pelvis or passage (size, shape, and adequacy of the pelvis)
-
Power (uterine contractility)
A prolonged latent phase may result from oversedation or from entering labor early with a thickened or uneffaced cervix. It may be misdiagnosed in the face of frequent prodromal contractions. Protraction of active labor is more easily diagnosed and is dependent upon the 3 P' s.
The first P, the passenger, may produce abnormal labor because of the infant's size (eg, macrosomia) or from malpresentation.
The second P, the pelvis, can cause abnormal labor because its contours may be too small or narrow to allow passage of the infant. Both the passenger and pelvis cause abnormal labor by a mechanical obstruction, referred to as mechanical dystocia.
With the third P, the power component, the frequency of uterine contraction may be adequate, but the intensity may be inadequate. Disruption of communication between adjacent segments of the uterus may also exist, resulting from surgical scarring, fibroids, or other conduction disruption. Whatever the cause, the contraction pattern fails to result in cervical effacement and dilation. This is called functional dystocia. Uterine contractile force can be quantified by the use of an intra-uterine pressure catheter. Use of this device allows for direct measurement and calculation of uterine contractility per each contraction and is reported in Montevideo units (MVUs). For uterine contractile force to be considered adequate, the force produced must exceed 200 MVUs during a 10-minute contraction period. Arrest disorders cannot be properly diagnosed until the patient is in the active phase and had no cervical change for 2 or more hours with the contraction pattern exceeding 200 MVUs. Uterine contractions must be considered adequate to correctly diagnose arrest of dilation. [14]
Etiology
Prolonged latent phase
The latent phase of labor is defined as the period of time starting with the onset of regular uterine contractions and ending with the onset of the active phase (usually 3-4 cm cervical dilation).
A prolonged latent phase is defined as exceeding 20 hours in patients who are nulliparas or 14 hours in patients who are multiparas.
The most common reason for prolonged latent phase is entering labor without substantial cervical effacement.
Power
Power is defined as uterine contractility multiplied by the frequency of contractions.
Montevideo units (MVUs) refer to the strength of contractions in millimeters of mercury multiplied by the frequency per 10 minutes as measured by intrauterine pressure transducer.
The uterine contraction pattern should repeat every 2-3 minutes.
The uterine contractile force produced must exceed 200 MVUs/10 min for active labor to be considered adequate. For example, 3 contractions in 10 minutes that each reach a peak of 60 mm Hg are 60 X 3 = 180 MVUs.
An arrest disorder of labor cannot be diagnosed until the patient is in the active phase and the contraction pattern exceeds 200 MVUs for 2 or more hours with no cervical change. Extending the minimum period of oxytocin augmentation for active-phase arrest from 2 up to 4 hours may be considered as long as fetal reassurance is noted with fetal heart rate monitoring.
Pelvis or the size of the passageway inhibiting delivery
The shape of the bony pelvis (eg, anthropoid or platypelloid) can result in abnormal labor.
A patient who is extremely short or obese, or who has had prior severe trauma to the bony pelvis, may also be at increased risk of abnormal labor.
Size and/or presentation of the infant
Abnormal labor could also be secondary to the passenger, the size of the infant, and/or the presentation of the infant. In addition to problems caused by the differential in size between the fetal head and the maternal bony pelvis, the fetal presentation may include asynclitism or head extension. Asynclitism is malposition of the fetal head within the pelvis, which compromises the narrowest diameter through the pelvis. Fetal macrosomia and other anomalies (including hydrocephalus, encephalocele, fetal goiter, cystic hygroma, hydrops, or any other abnormality that increases the size of the infant) are likely to cause deviation from the normal labor curve.
Other factors
Other factors include either a low-dose epidural or combined spinal-epidural anesthetics that minimize motor block and may contribute to a prolonged second stage. These have also been associated with an increase in oxytocin use and operative vaginal delivery. However, use of epidural for analgesia during labor does not result in a statistically significant increase in cesarean delivery. [15] Intravenous oversedation has also been implicated as prolonging labor in both the latent and active phases.
Epidemiology
United States statistics
Of all cephalic deliveries, 8-11% are complicated by an abnormal first stage of labor. Dystocia occurs in 12% of deliveries in women without a history of prior cesarean delivery. Dystocia may account for as many as 60% of cesarean deliveries.
Prognosis
The prognosis of subsequent pregnancies depends on the cause for abnormal labor. For example, if abnormal labor occurs from macrosomia, the next infant may not be macrosomic. However, if the abnormal labor was secondary to a contracted pelvis with a normal-sized or small infant, then the likelihood for a recurrence of abnormal labor is high.
In an attempt to determine whether increasing maternal age is more commonly associated with dystocia, a study by Treacy et al demonstrated that the incidences of oxytocin augmentation, prolonged labor, instrument delivery, and intrapartum cesarean delivery (including cesarean for dystocia) all increased significantly and progressively with increasing maternal age. [16] This study used an established active management protocol, and oxytocin augmentation proved a generally effective intervention in all age categories. These findings have implications for the analysis of intervention rates by health care providers, particularly in developed countries where the proportion of older nulliparas is increasing.
A study by Zhu et al revealed that, with increasing interpregnancy intervals, the risk for labor dystocia increases. [17] Both functional and mechanical dystocia were more prevalent in first births than in subsequent births. In singleton births to multiparous mothers, labor dystocia was associated with the interpregnancy interval in a dose-response fashion. Compared with an interpregnancy interval of less than 2 years, the adjusted odds ratios that was associated with interpregnancy intervals of 2-3, 4-5, 6-7, 8-9, and 10+ years were 1.06, 1.15, 1.25, 1.31, and 1.50, respectively, when controlled for other reproductive risk factors. Functional dystocia was associated more strongly with interpregnancy interval than mechanical dystocia.
Morbidity/mortality
Both maternal and fetal mortality and morbidity rates increase with abnormal labor. This is probably an effect-effect relationship rather than a cause-effect relationship. Nonetheless, identification of abnormal labor and initiation of appropriate actions to reduce the risks are matters of some urgency.
A meta-analysis by Pergialiotis et al found that a prolonged second stage of labor was associated with a higher risk of postpartum hemorrhage, chorioamnionitis, endometritis, postpartum fever, and obstetric anal sphincter injury. In addition, the risk of neonatal sepsis was higher, as was the likelihood of admission to the neonatal intensive care unit. [18]
Complications
Maternal infection is a risk, especially when rupture of membranes occurs for more than 18 hours. Administer antibiotics for signs and symptoms of chorioamnionitis.
Fetal compromise can occur from the inability to tolerate labor (eg, uterine hyperstimulation) or infection, and it must be closely evaluated. Fetal heart monitoring often reveals signs of compromise with decelerations, and fetal scalp pH is an option when indicated.
Probably the most common complication of the medical induction of labor is hyperstimulation of the uterus. If unrecognized and untreated, excessive stimulation of the uterus can result in fetal compromise, cord compression, and uteroplacental insufficiency. Uterine rupture, postpartum uterine atony, and postpartum hemorrhage may occur and can be life-threatening complications requiring emergent action.
Allen et al found that increased duration of the second stage of labor—in particular, duration longer than 3 hours in nulliparous women and longer than 2 hours in multiparous women—increases the risk of both maternal and perinatal adverse outcomes. In their population-based cohort study in 121,517 women (52% nulliparous), women with a prolonged second stage were at increased risk for obstetric trauma, postpartum hemorrhage, puerperal febrile morbidity, and composite maternal morbidity, while their infants were at increased risk for low 5-minute Apgar score (see the Apgar Score calculator), birth depression, admission to the neonatal intensive care unit, and composite perinatal morbidity. Method of delivery modified the effect of duration of second stage among nulliparous women only. [11]
Nerve injury is more common in nulliparous women and is associated with long labor, fetal macrosomia, and certain positions that women assume during labor. Peripheral nerve injuries typically manifest as weakness or numbness in the distribution of the affected nerve(s), and most authors describe an uncomplicated resolution of the neuropathy within approximately 6 months. The development of a complex regional pain syndrome has also been described. [19]
Patient Education
The patient must be aware of all risks involved with labor, including the potential for emergent cesarean delivery if the fetus appears compromised. Furthermore, she should be kept informed of her status throughout the labor course, especially if a change in management is anticipated. Counsel patients early in pregnancy that maternal weight gain correlates with fetal weight gain, and excessive gain and prepregnancy obesity are risk factors for abnormal labor.
For patient education resources, see Women's Health Center and Pregnancy Center, as well as Labor Signs.
-
Labor curve for nulliparas.
-
Labor curve for nulliparas versus multiparas.
-
Abnormal labor curve.
-
Average labor curves by parity in singleton term pregnancies with spontaneous onset of labor. Reprinted from Seminars in Perinatology, Vol 36(5), El-Sayed YY, Diagnosis and Management of Arrest Disorders: Duration to Wait, pgs 374-8, Oct 2012, with permission from Elsevier.
-
The 95th percentiles of cumulative duration of labor from admission among singleton term nulliparous women with spontaneous onset of labor, vaginal delivery, and normal neonatal outcomes. Reprinted from Seminars in Perinatology, Vol 36(5), El-Sayed YY, Diagnosis and Management of Arrest Disorders: Duration to Wait, pgs 374-8, Oct 2012, with permission from Elsevier.