Overview
The hallmark of acalculous cholecystopathy, frequently called biliary dyskinesia, is recurrent right upper quadrant pain in the absence of gallstones. Acalculous cholecystitis refers to cholecystitis without gallstones. Patients frequently undergo extensive, often invasive and expensive, testing before receiving definitive therapy. Although the treatment of choice is laparoscopic cholecystectomy, the rates of symptomatic improvement are not as favorable as in patients with gallstone-related biliary colic.
Surgeons typically label acalculous cholecystopathy as biliary dyskinesia. For gastroenterologists, biliary dyskinesia is a synonym for sphincter of Oddi dysfunction, which is a distinct disease process. This article discusses only acalculous cholecystopathy.
See Biliary Disease and Acalculous Cholecystitis for more information.
Prevalence
The true incidence of acalculous cholecystopathy in the United States is unknown, although the condition occurs more frequently in females than males and in individuals aged 40-60 years. However, with the advent of laparoscopic cholecystectomy, data exist that suggest an increased rate of cholecystectomy. In general, 10%-15% of patients undergoing laparoscopic cholecystectomy have biliary dyskinesia. Acute acalculous cholecystitis (AAC) can occur in young and middle-aged otherwise healthy individuals. [1]
In a study from a West European trauma unit, 10% of patients with severe multiple injuries developed cholecystitis requiring cholecystectomy. This included acute acalculous cholecystitis in about 40%, chronic acalculous cholecystitis (CAC) in 40% and cholecystitis with cholecystolithiasis in 20%. [2] In other series, chronic acalculous cholecystitis is about 9 times more common than acute acalculous cholecystitis. [3]
Presentation
The presentation of acute acalculous cholecystitis is highly variable—with or without right upper quadrant pain and tenderness, fever, leukocytosis, elevated liver enzymes, lipase or amylase—and may be similar to that of acute calculous cholecystitis (ACC). [4] Nausea is the most commonly associated symptom, although vomiting is unusual.
When pain is present, it characteristically occurs in the right upper quadrant 30-60 minutes after meals, usually lasts 1-4 hours, typically does not radiate, and is often exacerbated by greasy and spicy foods.
Other gastrointestinal symptoms suggest diagnoses other than acalculous cholecystopathy. Acute cholecystitis may occur as a complication of critical illness, such as sepsis or cardiovascular disease.
The physical examination is directed toward ruling out other possible etiologies of the pain. However, usually, there are no abnormal physical examination findings associated with acalculous cholecystopathy, although mild right upper quadrant tenderness may occur.
Infections associated with AAC
Acute acalculous cholecystitis has been described in association with a number of conditions including infections [5] (especially in the immunosuppressed person), such as the following:
-
Hepatitis B [9]
-
Hepatitis A [10, 11]
-
Acute Epstein-Barr viral infection in a person with Gilbert syndrome [14]
-
Granular cell tumor of the common hepatic duct [15]
-
After cardiopulmonary resuscitation [16]
Conditions associated with AAC/CAC
Acute and chronic acalculous cholecystitis are associated with the following:
-
X-linked chronic granulomatous disease [18]
-
Renal cell carcinoma treated with sunitinib [19]
-
Churg-Strauss syndrome with liver involvement [23, 24]
-
Mirizzi syndrome (a gallstone impacted at the neck of the gallbladder or in the cystic duct) [30]
-
Cholestatic hepatitis and hemolytic anemia [31]
-
Polyarteritis nodosa in a patient with or without primary Sjogren syndrome [32, 33]
-
Biliary tract neoplasm causing functional bile stasis [34]
-
Typhoid fever [39, 40]
-
Human immunodeficiency virus (HIV), antiretroviral therapy, immune restoration syndrome [41]
-
Burns [42]
-
Thermal injury from electrocution [45]
-
EBV-negative T-cell post-transplant lymphoproliferative disorder (PTLD) [46]
-
Acute hepatitis A [49, 50, 51]
-
Dengue fever [52, 53, 54]
-
Snake bite [57]
-
Plasma cell leukemia [58]
-
Lupus and antiphospholipid syndrome [59, 60, 61]
-
Nonalcoholic fatty pancreas disease with steatopancreatitis [63]
-
Plasmodium falciparum malaria [64]
-
Multiseptate gallbladder [65]
-
Neonates [66]
-
Eosinophilic vasculitis [67]
As compared with healthy gallbladders removed from persons having surgery for other reasons (controls), there were significant increases in the rates of gallbladder tissue apoptosis, proliferation, and hypoxia-inducible factor (HIF)-1 alpha in persons with acute acalculous cholecystitis and acute calculous cholecystitis, as compared with controls. [70]
In addition, tight junction proteins are differentially expressed in acute acalculous cholecystitis and acute calculous cholecystitis, as well as compared to normal control gallbladder epithelial cytoplasm, as shown in the table below. [71]
Table. Expression of Tight Junction Proteins Relative to Normal Gallbladders and AAC (Open Table in a new window)
Tight Junction Protein |
AAC (relative to normal gallbladder) |
ACC (relative to normal gallbladder or AAC) |
Occludin |
↓ |
↓ |
Claudin-1 |
↓ |
↓ |
Claudin-2 |
|
↑ |
Claudin-3, -4 |
|
↓ |
Z0-1 |
|
↓ |
| AAC = acute acalculous cholecystitis. | ||
Differential Diagnosis
Choledocholithiasis
Laboratory Tests
No specific laboratory studies for acalculous cholecystopathy exist. Instead, the studies help rule out other conditions that are part of the differential diagnosis (see the Differential Diagnosis section).
-
Liver profile – To rule out hepatitis, acute cholecystitis, and choledocholithiasis
-
Complete blood cell (CBC) count – To rule out acute inflammation as observed in cases of hepatitis or acute cholecystitis
-
Helicobacter pylori serology or breath testing – Helpful in ruling out causes of gastritis and peptic ulcer disease
Ultrasonography
Ultrasonography is also most useful to rule out conditions in the differential diagnosis (see the Differential Diagnosis section), as results are usually normal in patients with acalculous cholecystopathy. Ultrasonography of the right upper quadrant detects abnormalities of the gallbladder, including the presence (or absence) of stones, wall thickening, or pericholecystic fluid, and it is also useful in detecting hepatic masses. Dilatation of the intrahepatic and extrahepatic biliary tree suggests biliary obstruction due to stone, stricture, or malignancy.
Hepatobiliary Scanning
HIDA scanning
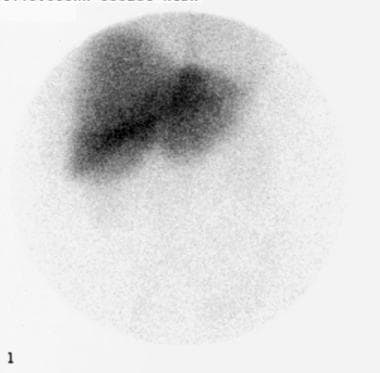
Hydroxy iminodiacetic acid [HIDA]) scanning may have some use in determining which patients with right upper quadrant pain, a lack of gallstones, and no other etiology may benefit from cholecystectomy. See the following images.
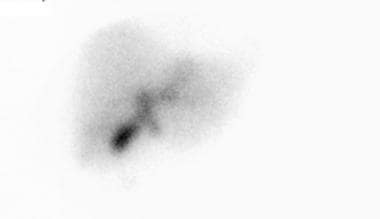
 Hepatobiliary (HIDA) scan showing persistent gallbladder activity despite washout of radioisotope from liver and remainder of the biliary tree, which is suggestive of acalculous cholecystopathy.
Hepatobiliary (HIDA) scan showing persistent gallbladder activity despite washout of radioisotope from liver and remainder of the biliary tree, which is suggestive of acalculous cholecystopathy.
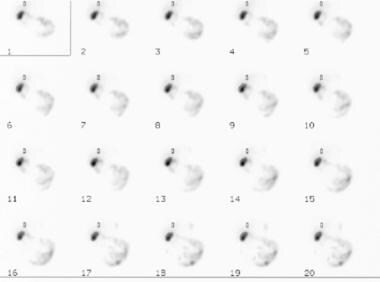
After the gallbladder fills with the radioisotope, a cholecystokinin analog is administered. This analog stimulates emptying of the gallbladder, allowing an ejection fraction to be calculated. A gallbladder ejection fraction of less than 35% is considered abnormal. See the image below.
However, there are discrepant results with HIDA scanning in determining which patients with acalculous cholecystopathy may benefit from cholecystectomy. In one study, the sensitivity was less than 60%, and the specificity was less than 70%, with a positive predictive value (PPV) of 91.3% and a negative predictive value (NPV) of only 22.5%. [72]
This controversy may be because no consensus exists regarding the dose and the infusion rate of cholecystokinin or regarding the definition of an abnormal ejection fraction. Some patients with a normal ejection fraction may respond to surgical therapy. It remains unknown if there is a causal overlap between a low ejection fraction and sphincter of Oddi spasm, and it is controversial whether an ejection fraction of less than 35% in a patient with the appropriate symptom complex may benefit from laparoscopic cholecystectomy. [73] Administration of the analog also may recreate the pain experienced by the patient.
However, HIDA scanning has high sensitivity and specificity to help establish the diagnosis of acute cholecystitis.
Fatty meal cholescintigraphy
Fatty meal cholescintigraphy (CS) is also used to diagnose chronic acalculous cholecystitis. Of all the measurement variables related to cholescintigraphy (such as latent period, the pattern of gallbladder emptying, onset of gallbladder filling, and the biliary-to-bowel transit time), only the gallbladder ejection fraction (GBEF) is of diagnostic value in chronic acalculous cholecystitis. [74] A GBEF of less than 50% is considered to be abnormal. [75]
Technetium-99m disofenin imaging
In persons with right upper quadrant or abdominal pain, technetium-99m (99m Tc)-disofenin hepatobiliary imaging with the ingestion of 3 mL corn oil emulsion after gallbladder filling, and calculating the ejection fraction at 60 minutes provided high diagnostic accuracy for chronic acalculous cholecystitis. [76] Receiver-operating-characteristic analysis showed that the 60-minute GBEF best distinguished between chronic acalculous cholecystitis and non-gallbladder disease (based on clinical follow-up). An ejection fraction of 20% or less had 100% sensitivity and 97% overall accuracy for the diagnosis of chronic acalculous cholecystitis. [76]
Computed Tomography Scanning
Although computed tomography (CT) scanning of the abdomen, with or without contrast, is generally recommended to assess most causes of intra-abdominal pathology, the exceptions to this rule are the use of magnetic resonance imaging (MRI) to detect abscesses and abdominal ultrasonography to detect gallbladder pathology such as acalculous and calculous cholecystitis. [77]
Unfortunately, CT scanning is rarely useful in diagnosing acalculous cholecystopathy. Instead, this modality helps to rule out (when indicated) other conditions in the differential diagnosis (see the Differential Diagnosis section).
Histopathologic Findings
There is an overlap in the histopathology of acute acalculous cholecystitis and acute calculous cholecystitis in critically ill patients, [78] and it has been suggested that based on the comparison between the two conditions that acute acalculous cholecystitis "is largely a manifestation of systemic critical illness, whereas [acute calculous cholecystitis] is a local disease of the gallbladder." In acute acalculous cholecystitis, the following findings are observed:
-
Bile infiltration in the gallbladder muscle layer is more common, deeper, and wider.
-
Epithelial degeneration is prominent.
-
Inflammatory cells are widespread.
-
Necrosis in the muscle layer is more common and wider and deeper.
Endoscopy
Additional investigative procedures are used, when indicated, to rule out other conditions in the differential diagnosis (see the Differential Diagnosis section).
Upper endoscopy is the most commonly performed procedure; findings are normal in patients with acalculous cholecystopathy. However, endoscopy is very accurate in detecting gastritis and peptic ulcer disease, which should be treated appropriately before considering cholecystectomy for acalculous cholecystopathy.
Medical Treatment
No effective medical treatment of acalculous cholecystopathy exists. However, some authors suggest that in patients with acute acalculous cholecystitis without overt peritonitis, antibiotics may be useful before cholecystectomy. In addition, postoperative pain medications are provided, but these agents are usually only required for 7-10 days in progressively decreasing amounts.
Surgical Treatment
Gastroenterologists and surgeons are the specialists usually involved in the care of these patients. Patients undergoing surgical therapy have been reported to be 2.8 times more likely to have symptomatic relief versus nonoperative therapy.
Laparoscopic cholecystectomy is indicated for the treatment of biliary dyskinesia after all of the other conditions in the differential diagnosis have been ruled out with a reasonable degree of certainty (see Differential Diagnosis). [79, 80] The procedure is usually performed as an outpatient operation.
A meta-analysis of 10 studies confirmed that in persons with right upper quadrant pain, absence of gallstones, and low gallbladder ejection fraction (GBEF) on hydroxy iminodiacetic acid (HIDA) scans, cholecystectomy was much more likely (96%) than medical treatment (4%) to result in symptom improvement. [81]
Intraoperative cholangiography is performed at the discretion of the operating surgeon.
High-risk patients
In the critically-ill patient with either acute acalculous cholecystitis or acute calculous cholecystitis, ultrasound-guided percutaneous cholecystotomy [82] or endoscopic retrograde cholangiopancreatography (ERCP), [83] sphincterotomy, stone extraction, and nasobiliary drainage and lavage are the treatment options that may be used. [4, 83]
Percutaneous transhepatic gallbladder drainage with the use of gallbladder stenting is palliative therapy for acute calculous cholecystitis as well as acute acalculous cholecystitis in high-risk persons. [84] The mortality rate was reported to be less than 5% if the diagnosis was made early and cholecystectomy was performed within 24 hours.
Postoperative monitoring
In the absence of complications, the patient usually is seen 2-4 weeks after the operation.
Complications
Complications of acalculous cholecystopathy are those related to cholecystectomy. In addition to the morbidities inherent in any procedure (eg, bleeding, infection, damage to adjacent structures), several morbidities are unique to laparoscopic cholecystectomy. The rate of bile duct injury is approximately 3 cases per 1000 procedures.
Complications related to carbon dioxide pneumoperitoneum, such as acidosis and shoulder pain, may also occur. These complications usually resolve rapidly in most healthy patients.
Prognosis
The mortality and morbidity of acalculous cholecystopathy are related to the invasive diagnostic tests that frequently are performed and to the treatment of the condition (ie, cholecystectomy). Biliary dyskinesia does not progress to more serious conditions, such as acute cholecystitis.
The prognosis of acute acalculous cholecystitis is good if the condition is diagnosed early and treated with cholecystectomy. However, most cases of acute acalculous cholecystitis occur in persons with serious comorbidities (eg, cardiopulmonary disease, trauma, or extensive burns), [85] and these persons have a high morbidity and mortality, [86] especially from multiorgan failure. [86] In fact, in a Swedish study, patients with acalculous gallbladder disease had double the mortality risk compared with patients with calculous disease, and patients with acute cholecystitis had double the mortality risk as compared to those with chronic cholecystitis. [87] The postoperative crude mortality within 30 days was 0.4%. [87]
Laparoscopic cholecystectomy provides symptomatic relief in 90%-95% of cases of biliary colic associated with gallstones. In contrast, despite appropriate patient selection, only approximately 80% of patients with acalculous cholecystopathy experience resolution of their symptoms (see Special Concerns).
Special Concerns
The main pitfall is failure to consider and evaluate the patient for other conditions in the differential diagnosis, especially malignancy (see the Differential Diagnosis section). The other potential source of problem and patient dissatisfaction is the failure to inform patients of the possibility of persistent symptoms following the operation. Although most patients will experience relief or improvement in their symptoms, approximately 15%-20% will continue to experience the same pain they felt preoperatively.
-
Hepatobiliary (HIDA) scan showing liver uptake of the radioisotope.
-
Hepatobiliary (HIDA) scan showing biliary excretion of the radioisotope.
-
Hepatobiliary (HIDA) scan showing persistent gallbladder activity despite washout of radioisotope from liver and remainder of the biliary tree, which is suggestive of acalculous cholecystopathy.
-
Impaired gallbladder emptying despite injection of cholecystokinin analog.