Overview
Background
“Once a cesarean, always a cesarean.” From 1916, when these words were spoken to the New York Association of Obstetricians & Gynecologists, through the ensuing 50-60 years, this statement reflected most of US obstetricians’ management of patients with a prior cesarean delivery. By 1988, the overall cesarean delivery rate was 25%, rising from less than 5% in the early 1970s. Only 3% of live-born infants were delivered vaginally after the mother had undergone a prior cesarean delivery.
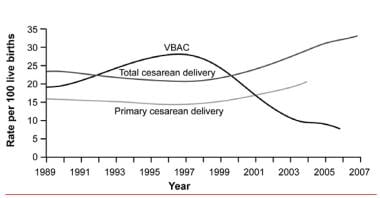
Although attempts at a trial of labor after a cesarean birth (TOLAC) have become accepted practice, the rate of successful vaginal birth after cesarean delivery (VBAC), as well as the rate of attempted VBACs, decreased during a 10-year period (see the image below). Whereas 40-50% of women attempted VBAC in 1996, as few as 20% of patients with a prior cesarean delivery attempted a trial of labor in 2002. This number drifted down toward the 10% mark, with fewer than 10% of women achieving successful VBAC in 2005. More recent data show that from 2016 to 2018, rates of VBAC in the United States rose from 12.4% in 2016 to 12.8% in 2017 and to 13.3% in 2018. [1]
Despite the known risks (0.5-1% rate of uterine rupture), TOLAC remains an attractive option for many patients and leads to a successful outcome in a high proportion of cases. In comparison, the alternative of elective repeat cesarean delivery is not without risks. In addition to the inherent risks that cesarean delivery has over vaginal delivery, patients may experience uterine rupture prior to the onset of labor.
The decision to undergo TOLAC is an individual one that should be based on careful, thorough counseling. [2] Maternal characteristics and obstetric history can provide a patient a rough estimate of her chance of a successful trial of labor. This same obstetric history can be used to estimate a patient’s risk of uterine rupture.
If possible, avoid induction of labor, because induction of labor decreases the probability of success and increases the chance of uterine rupture in a trial of labor after cesarean delivery. Counsel patients who elect to undergo TOLAC to be evaluated early in labor and to manage the pregnancy in a hospital setting in which uterine rupture can be both recognized and managed expediently.
Certainly, counseling should address the question of whether patients are interested in subsequent pregnancies after the current pregnancy. Undergoing 2 prior cesarean deliveries further increases the risks of VBAC in a subsequent pregnancy; thus, for a future pregnancy, having had a successful VBAC offers protection after undergoing the risk in the current pregnancy.
Go to Cesarean Delivery and Perimortem Cesarean Delivery for complete information on these topics.
ACOG guidelines
Several factors contributed to a decline in VBAC. As practitioners experience complications related to managing patients undergoing trials of labor after cesarean delivery, they are less likely to allow new patients to undergo a trial of labor. In addition, 1999 guidelines from the American College of Obstetricians and Gynecologists (ACOG) stated explicitly that patients undergoing TOLAC require the presence of an obstetrician, an anesthesiologist, and/or a staff capable of performing an emergency cesarean delivery throughout the patient’s active phase of labor. [3]
Whereas academic centers and larger community hospitals are able to comply with these requirements, many smaller hospitals do not offer in-house anesthesia or obstetric staff. Furthermore, to meet the financial demands of managed care, many obstetricians now cover more than one hospital simultaneously, making it difficult to comply with the 1999 guidelines.
The impact of these changes can be observed in national birth statistics. The cesarean delivery rate peaked at 25% in 1988 but then declined to 21% overall in 1996. From 1996 to 2004, however, the cesarean delivery rate increased to 29.2%, while the rate of VBAC declined from 28% to 9%. On the assumption that the overall VBAC success rate is about 70%, this correlates with a decline from 40% to 14% in the number of patients choosing to undergo TOLAC.
What once was hailed as a key component of lowering the overall cesarean birth rate (ie, TOLAC) is losing the support it had in the 1980s. Overall, this has led to a rate of cesarean delivery of 31.1% in 2006, which is the highest rate in US history and shows no signs of decreasing.
In 2010, with these developments in mind, ACOG issued new guidelines that were somewhat less restrictive. [4, 5] The 2010 guidelines, based on consensus and expert opinion, recommend that TOLAC should be undertaken at facilities capable of emergency deliveries. Because of the risks associated with TOLAC and complications such as uterine rupture that may be unpredictable, ACOG recommends that TOLAC be undertaken in facilities with staff immediately available to provide emergency care.
However, when resources for immediate cesarean delivery are not available, health care providers and patients considering TOLAC should discuss the hospital’s resources and availability of obstetric, pediatric, anesthetic, and operating room staffs. Respect for patient autonomy supports allowing patients to accept increased levels of risk; however, patients should be clearly informed of such potential increase in risk and counseled about management alternatives.
Recognizing that TOLAC was decreasing at community and more rural hospitals, ACOG revised these recommendations in 2017 with an apparent goal in softening the recommendation for immediate availability of surgical teams. The language now reads "ACOG recommends that TOLAC be attempted in facilities that can provide cesarean delivery for situations that are immediate threats to the life of the woman and the fetus". This more nuanced statement may result in an increase in attempted TOLAC at these facilities. [6]
On the basis of level A evidence, the 2017 ACOG guidelines make the following recommendations [6] :
-
Most women with a prior cesarean delivery with a low transverse incision are candidates for VBAC and should be offered TOLAC.
-
Epidural anesthesia may be used as part of TOLAC.
-
Misoprostol should not be used for patients who have had a prior cesarean delivery or major uterine surgery.
On the basis of level B evidence, TOLAC may be considered for the following patients [6] :
-
Women with 2 previous low transverse cesarean deliveries
-
Women with 1 previous cesarean delivery with a low transverse incision who are otherwise appropriate candidates for twin vaginal delivery
-
Women with 1 previous cesarean delivery of unknown incision type, unless clinical suspicion of a previous classical uterine incision is high
-
Women with 1 previous cesarean delivery who are otherwise appropriate candidates for twin vaginal delivery.
Level B evidence was also found for the following:
-
Induction of labor during TOLAC is not contraindicated.
-
In women with a prior low transverse uterine incision who are at low risk for adverse maternal or neonatal outcomes from external cephalic version and TOLAC, external cephalic version for breech presentation is not contraindicated.
-
Continuous fetal heart rate monitoring is recommended during TOLAC
A comparison of VBAC in the United States, the United Kingdom, and Canada showed understandable similarities but numerous unexplained differences in recommendations. [7]
Outcomes of interest
Two specific outcomes of interest regarding TOLAC have been well investigated: successful VBAC and uterine rupture. Other outcomes are certainly of interest, including neonatal outcome, hysterectomy, and maternal mortality; however, few studies have focused on these outcomes, and poor outcomes occur too rarely to be well represented in established databases.
In earlier studies, most outcomes were reported after univariate analysis. Risk factors were examined without controlling for potential confounding variables, and results were reported as a relative risk or odds ratio. These ratios represent the risk of the group of individuals who have the risk factor divided by individuals without the risk factor. Over the last decade, several large cohorts have examined predictors and outcomes related to women with a prior cesarean delivery. These studies have ranged from Nova Scotia to Boston to the state of Washington.
Finally, 2 large multicenter studies have been publishing multiple studies on this issue, one out of Pennsylvania and the other out of the Maternal-Fetal Medicine Units. These large studies over the last decade have used multivariate statistics to examine risk factors. This means that other risk factors and confounding factors, such as birth weight, maternal age, obstetric history, and labor management, were controlled for in the analysis.
In this article, factors associated with mode of delivery in the setting of a trial of labor and factors associated with uterine rupture in this same setting are reviewed.
Indications
The predictors of successful TOLAC are extensively described in the existing literature (see the table below). Although no randomized trials have been conducted, relatively large databases have been analyzed (with both univariate and multivariate techniques) to determine risk factors for patients undergoing TOLAC.
In addition, several scoring systems have been devised to help predict which patients are likely to be successful when attempting VBAC. These scoring systems are quite varied and may inform the discussion with the patient about TOLAC. However, there are no prospective studies that demonstrate that these systems improve perinatal outcomes. Examples of these calculators can be found on the ACOG website. The Eunice Kennedy Shriver National Institute of Child Health and Human Development VBAC Calculator was updated in 2021 to remove race and ethnicity as a predictor and to add the variable of chronic hypertension treated with medication. [8] ACOG emphasizes that a VBAC calculator score should not be used as a barrier to TOLAC; it is one of many tools that can be used to inform shared decision-making. [9]
Table 1. Predictors of VBAC Success or Failure (Open Table in a new window)
Increased Chance of Success |
Decreased Chance of Success |
Prior vaginal delivery |
Maternal obesity |
Prior VBAC |
Short maternal stature |
Spontaneous labor |
Macrosomia |
Favorable cervix |
Increased maternal age (>40 y) |
Nonrecurring indication (breech presentation, placenta previa, herpes) |
Induction of labor |
Preterm delivery |
Recurring indication (cephalopelvic disproportion, failed second stage) |
|
Increased interpregnancy weight gain |
|
Latina or African American race/ethnicity |
|
Gestational age ≥41 wk |
|
Preconceptional or gestational diabetes mellitus |
Because no large, prospective, randomized, controlled trials have been conducted, most of the risk factors have been determined from retrospective cohort and case-control studies. These studies have been increasingly analyzed with multivariate techniques to control for confounding factors. However, control for physician practice is difficult, and physician practice can greatly impact the strength of the association between these risk factors and a successful VBAC.
Even when demographic data, obstetric history, birth weight, gestational age, induction of labor, and other variables are controlled for, the bias inherent in nonrandomized and nonblinded trials cannot be eliminated.
Maternal characteristics
Several studies examine prepregnancy weight and height to examine the effect on mode of delivery. Not surprising, women who are shorter and women who are obese are more likely to undergo cesarean delivery. Of note, cesarean delivery has been associated not only with increased prepregnancy weight but also with increased gestational weight gain.
An increasing number of studies have been carried out in the setting of TOLAC, all of which show that women in the morbidly obese range have a higher risk of failing a trial of labor. Interpregnancy weight gain has been shown to increase the risk of failure in a subsequent trial of labor, but unfortunately, interpregnancy weight loss has not demonstrated an improvement in VBAC success.
Maternal age has also been examined in several studies in VBAC literature. With confounding factors adjusted for, women older than 40 years who have had a prior cesarean delivery have an almost 3-fold higher risk for a failed trial of labor than do women younger than 40 years. In 1 scoring system, women younger than 40 years were given an extra point as a predictor for successful VBAC. [10]
Maternal race or ethnicity has been examined as a predictor for VBAC in the setting of trial of labor and has not generally been noted to be a strong predictor. However, in the recent Maternal-Fetal Medicine Unit (MFMU) Cesarean Registry, both Hispanic ethnicity and African American ethnicity were associated with lower rates of successful trial of labor. Whether this association is due to actual biologic reasons or whether ethnicity is acting as a proxy for some other factor or factors remains to be elucidated.
Birth weight
Birth weight greater than 4000 g is associated with an almost 4-fold higher risk of cesarean birth among nulliparous women. Several studies have demonstrated a difference in VBAC rates between patients with a birth weight greater than 4000 g and those with a lower birth weight. In accordance with these findings, several studies have demonstrated a higher failure of a trial of labor with increasing birth weight.
Obstetric history
Obstetric history is enormously important in terms of risk factors for successful TOLAC. Predictors of increased success include a nonrecurring indication for prior cesarean delivery (eg, breech presentation, placenta previa) and prior vaginal delivery. A history of cephalopelvic disproportion (CPD), failure to progress, no prior vaginal deliveries, or a prior cesarean delivery performed in the second stage of labor are negative predictors of success in a subsequent trial of labor.
Several studies have examined indications for prior cesarean delivery as a predictor of outcome in subsequent TOLAC. In all studies, CPD had the lowest VBAC success rate (60-65%). Fetal distress (eg, nonreassuring fetal testing) had the second lowest success rate of VBAC (69-73%). Nonrecurrent indications, such as breech birth, herpes, and placenta previa, were associated with the highest rates of success (77-89%).
Failure to progress, CPD, or dystocia as indications for prior cesarean delivery are also associated with a higher proportion of patients not attempting a trial of labor after cesarean birth. In a meta-analysis of the existing literature prior to 1990, Rosen et al demonstrated that women whose prior cesarean delivery was performed for CPD were twice as likely to have an unsuccessful trial of labor. [10]
Patients with a prior vaginal delivery have higher rates of successful VBAC than patients without a prior vaginal birth. Furthermore, women with a successful VBAC have a higher success rate in a subsequent trial of labor compared with women whose vaginal delivery was prior to cesarean delivery.
In an unadjusted comparison, patients with 1 prior vaginal delivery had an 89% VBAC success rate compared with a 70% success rate in patients without a prior vaginal delivery. In comparable comparisons controlling for confounding factors, odds ratios of 0.3-0.5 for rate of cesarean delivery are found. Among patients with a prior VBAC, the success rate is 93%, compared with 85% in patients with a vaginal delivery prior to their cesarean birth but no prior VBAC. These findings have been repeatedly validated by multiple studies.
Only 1 study carefully examines cervical dilation at prior cesarean delivery. In this study, the degree of cervical dilation in the prior delivery is directly associated with the likelihood of success in a subsequent trial of labor. For example, 67% of patients who were dilated 5 cm or less at the time of their delivery had a successful VBAC, compared with 73% of patients who were dilated 6-9 cm.
The success rate is much lower for patients whose labor arrested in the second stage: only 13% of patients who were fully dilated at the time of their prior delivery had a successful VBAC. In a similar study, patients who had their prior cesarean delivery in the first stage of labor had a lower rate of cesarean delivery than those who had their prior cesarean delivery in the second stage of labor. However, in this study, 66% of patients who had a cesarean delivery for dystocia in the second stage had a successful VBAC.
Induction of labor
Patients who undergo induction of labor are at a higher risk of cesarean delivery than women who experience spontaneous labor. This finding has also been observed in women with a prior cesarean delivery. Several studies have demonstrated that women who are induced in TOLAC have a 2- to 3-fold increased risk of cesarean delivery compared with those who present with spontaneous labor.
One study demonstrated that patients who could be induced with oxytocin had a significantly lower cesarean delivery rate compared with those induced with a Foley bulb.
The 2017 ACOG guidelines state that induction of labor for maternal or fetal indications remains an option in women undergoing TOLAC. [6]
Gestational age
Increasing gestational age is associated with a decreased rate of successful VBAC. Three potential factors are related to the association of increasing gestational age with an increased rate of cesarean delivery: increasing birth weight, increased risk of fetal intolerance of labor, and increased need for induction of labor. However, in a recent study that controlled for both birth weight and induction/augmentation of labor, gestational age of greater than 41 weeks was still associated with failed VBAC.
Cervical examination on admission
Not surprisingly, patients who present to labor and delivery with advanced cervical examination findings have a greater success rate of vaginal birth. Several components of the cervical examination have been investigated, including cervical dilation and cervical effacement. Not surprisingly, the more advanced the cervical examination finding is upon initial presentation, the higher the rate of successful VBAC. A 1997 Flamm et al study demonstrated that patients presenting with dilation greater than or equal to 4 cm had an 86% rate of VBAC. [11]
Interpregnancy interval
The timing between pregnancies has recently become an interesting predictor for a number of obstetric outcomes, VBAC success among them. In 1 analysis, women who had an interpregnancy interval of more than 18 months had an 86% chance of VBAC success, while women whose interpregnancy interval was less than 18 months had a VBAC success rate of 79%. This difference was not statistically significant, and it remains unclear whether the interpregnancy interval actually affects the success rate or whether it affects only the risk of uterine rupture.
Preterm delivery
Preterm labor and delivery deserves attention as an opportunity to recounsel women about the risks and benefits of a trial of labor after cesarean delivery. In a large study by Quinones et al, 12,463 attempted a trial of labor, and the VBAC success rates for the term and preterm groups were 74% and 82%, respectively. [12] Additionally, a trend toward decreased risk of uterine rupture among preterm delivery gestations was found. These data can certainly be used to counsel women with a prior cesarean who are in preterm labor.
Gestational or pregestational diabetes
Only 1 study of patients undergoing a trial of labor after cesarean delivery has examined the rate of success in patients with diabetes mellitus (DM). This study demonstrated that patients with either gestational DM or pregestational DM had a lower rate of successful trial of labor. These findings are not particularly surprising; however, further studies are needed to sort out the differences between gestational and pregestational DM and the interaction between DM and birth weight.
Contraindications
One of the most significant risks women face when considering a trial of labor is that of uterine rupture. This potentially fatal event may have significant maternal and neonatal sequelae.
A threshold of acceptable risk has been established between the risk reported in women with 1 prior cesarean delivery (0.5-1%) and that seen in women with a history of a prior classic cesarean delivery (6-12%). The latter patients, along with women who have undergone metroplasties for uterine anomalies or myomectomies that have entered the uterine cavity, are discouraged from attempting VBAC.
Other patients who are at increased risk for uterine rupture include those who have had 2 or more hysterotomies, those who are treated with prostaglandin agents, and those undergoing induction of labor (see the table below).
Table 2: Predictors of Uterine Rupture (Open Table in a new window)
Increased Rate of Uterine Rupture |
Decreased Rate of Uterine Rupture |
Classic hysterotomy |
Spontaneous labor |
Two or more cesarean deliveries |
Prior vaginal delivery |
Single-layer closure |
Longer interpregnancy interval |
Induction of labor |
Preterm delivery |
Use of prostaglandins |
|
Short interpregnancy interval |
|
Infection at prior cesarean delivery |
|
Nature of hysterotomy
Unquestionably, practitioners do not feel safe allowing a patient who has had a prior classical hysterotomy (ie, a vertical incision that has extended above the insertion of the round ligaments) to undergo TOLAC. Patients with a prior classical hysterotomy have a higher rate of uterine rupture in subsequent pregnancies. Because these patients can sustain a uterine rupture prior to labor, they are often delivered at 36-37 weeks’ gestation. Although available data are limited, the risk of uterine rupture in this group of patients is estimated at 6-12%.
Retrospective cohort studies have demonstrated that the risk of uterine rupture is no greater for patients who have had a vertical incision in the lower uterine segment than for those who have had a transverse incision. The rate of uterine rupture from these studies is 0.8-1.3%. When comparing patients with prior Krönig hysterotomies to patients with low transverse incisions, no statistical difference exists in either univariate or multivariate analyses controlling for the confounding factors of obstetrical history, induction of labor, birth weight, and length of labor.
Most babies delivered abdominally are delivered through a transverse incision in the lower uterine segment (Kerr hysterotomy). In several large retrospective cohort studies, the reported rate of uterine rupture is 0.3-1% (see the table below). [13, 14, 15, 16, 17, 18] Rates of 0.5-1% (1 in 200 to 1 in 100) are commonly used to counsel patients with no other additional risk factors.
Table 3: Rates of Uterine Rupture (Open Table in a new window)
Study |
Sample Size (N) |
No. of Uterine Ruptures (Rate) |
|
Miller (1994) |
10,880 |
63 (0.6%)* |
|
Flamm (1994) |
5,022 |
39 (0.8%) |
|
McMahon (1996) |
3,249 |
10 (0.3%) |
|
Shipp (1999) |
2,912 |
28 (1%) |
|
Landon (2004) |
17,898 |
124 (0.7 %) |
|
Macones (2005) |
13,331 |
128 (0.9%) |
|
*Includes unknown |
|||
When an operative report of a patient’s prior cesarean delivery is unavailable, the obstetric history may be helpful in determining the type of uterine incision. For example, a patient who underwent a cesarean delivery for a breech presentation at 28 weeks’ gestation has a much higher risk of a vertical uterine incision than the patient at term with arrest of dilation. Because most cesarean deliveries are via low transverse hysterotomies, the risk of uterine rupture for patients with an unknown uterine scar is usually similar to that of patients with a prior transverse incision.
Several studies examining this issue have demonstrated that the rate of rupture for patients with an unknown uterine incision is approximately 0.6%. A case-control study of patients with and without uterine rupture did not find unknown hysterotomy to be a risk factor compared with low transverse hysterotomy. [19]
According to the 2017 ACOG guidelines, TOLAC is not contraindicated for women with previous cesarean delivery with an unknown uterine scar type unless clinical suspicion of a previous classical uterine incision is high. [6]
Number of prior cesarean deliveries
Patients with more than 1 prior cesarean delivery are at increased risk of uterine rupture. The unadjusted rate of uterine rupture for patients with 2 prior uterine incisions ranges from 1.8% to 3.7%.
One analysis demonstrated that when potential confounding variables (eg, prior vaginal delivery) are controlled for, patients who have had 2 prior cesarean deliveries have 5 times the risk of uterine rupture compared with patients who have had only 1 prior cesarean delivery. This finding contradicted several earlier studies that did not control for confounding factors, most importantly prior vaginal delivery.
More recently, a study that examined major complications overall found that while there was a statistically significant increase, the adjusted odds ratio was only 1.6.
Type of uterine closure
Whereas the uterine hysterotomy had traditionally been closed in several layers, in the 1990s physicians at many institutions began closing the Kerr hysterotomy in a single layer. Because the lower uterine segment is quite thin, a single layer often afforded adequate hemostasis. Several recent studies have compared women whose hysterotomy was closed in a single layer with those whose hysterotomy was closed in 2 layers. Adjusted odds ratios of 3 to 4 for uterine rupture have been estimated for women who have a single-layer closure.
Prior vaginal delivery
Prior vaginal delivery appears to be protective for subsequent uterine rupture. A 2000 study by Zelop et al demonstrated that patients with a prior vaginal delivery had a 0.2% rate of rupture compared with 1.1% for patients with no prior vaginal delivery. An adjusted odds ratio controlling for confounding factors was 6.2. [20]
No studies have compared the rate of uterine rupture in patients with a prior VBAC with those with a vaginal delivery before their prior cesarean delivery. These findings have been validated in subsequent studies, though the effect size has not been quite as large.
Prior infection
A recent study demonstrated that women who had an infection at the time of the cesarean delivery have an increased rate of uterine rupture in a subsequent trial of labor. The assumed causal mechanism is poor healing of the hysterotomy secondary to the infection.
Labor
While labor appears to be a risk factor for uterine rupture, many patients experience a uterine rupture prior to the onset of labor. In a large study using birth certificate data, one study found that the rate of uterine rupture before the onset of labor was 0.5%. Patients at greatest risk are those with prior classical hysterotomies. As a result of this potential risk, these patients are usually scheduled for delivery at 36-37 weeks’ gestation.
When counseling this group of patients, however, mentioning that scheduling an early repeat cesarean delivery does not eliminate the risk of uterine rupture entirely is important.
Induction of labor
Induction of labor as a risk factor for uterine rupture has been examined over only the past 5 years. One large study, which did not control for confounding factors, demonstrated a uterine rupture rate of 2.3% in patients who had experienced induced labor. In several studies controlling for confounding factors, adjusted odds ratios were 2-4 for patients who were induced compared with those who presented in spontaneous labor.
Despite these analyses, discerning whether induction of labor itself leads to uterine rupture or whether another risk factor (as yet unmeasured) is associated with both induction of labor and uterine rupture is difficult. When patients have an indication for induction of labor, the best course of management is to discuss the increase over their baseline risk of uterine rupture.
Use of oxytocin
In the only prospective randomized trial in women with a prior cesarean delivery, oxytocin augmentation in early labor was compared with expectant management; 5 uterine ruptures occurred in the augmentation group (5%), and none occurred in the expectant management group. Excessive use of oxytocin has been described as leading to an increased risk of uterine rupture.
A 1993 study by Leung et al demonstrated an odds ratio of 2.7 for uterine rupture in patients who used oxytocin compared with those without oxytocin augmentation. [19] However, this study included inductions and augmentation in both the latent and active phases. These confounding factors may have contributed to much of the difference because induction of labor alone has an increased risk.
In 2 subsequent studies, oxytocin augmentation was associated with uterine rupture. [21, 13] In the first study, although the odds ratio was 2.3, it was not statistically significant, probably because of inadequate statistical power. In the latter study, a similar odds ratio of 2.4 existed.
Because labor and delivery units use oxytocin widely, this oxytocin–uterine rupture relationship deserves careful consideration; the relationship directly affects management of patients. At this point, using oxytocin for induction and augmentation is probably advisable only when absolutely necessary.
Use of prostaglandins
Evidence regarding the use of prostaglandins for induction of labor remains scant. However, in the few trials that have been conducted, the trend is toward an increase in the rate of uterine rupture. In 1999, the use of prostaglandin E2 was demonstrated to have an adjusted odds ratio of 3.2. This study controlled for induction of labor, which appears to be an independent risk factor.
In 2001, Lydon-Rochelle et al demonstrated a 3-fold increase in the risk for uterine rupture when comparing patients induced with prostaglandins with those induced with oxytocin. [22] In the 2004 study by Landon et al, this effect of prostaglandin induction versus other means was smaller—less than 2-fold (odds ratio of 3.95 with prostaglandin, 2.48 without prostaglandin). [13]
As in studies examining the risk of uterine rupture in patients undergoing induction of labor, patients who were treated with prostaglandins were likely to have other confounding variables that were not controlled.
In particular, the prostaglandin misoprostol has been examined in small studies. In 1998, Wing et al reported a case series of 17 patients who were induced with misoprostol, in which 2 uterine ruptures occurred. These findings have led to the decreased use of prostaglandins for induction, particularly misoprostol. [23]
Use of transcervical Foley bulb
Only one small study exists of patients with a prior cesarean being induced with the transcervical Foley bulb. In that study, the rate of uterine rupture was 1.1% with spontaneous labor, 1.2% with induction with amniotomy, and 1.6% with use of a transcervical Foley bulb. This rate is lower than some of the reported rates with prostaglandins, but it is unclear whether the increase seen in patients requiring cervical ripening is due to the need for cervical ripening or to the agents themselves.
Interpregnancy interval
Several studies have demonstrated that the shorter the amount of time between the cesarean delivery and the subsequent delivery, the higher the rate of uterine rupture. Commonly, thresholds of 18 and 24 months have been examined. Adjusted odds ratios range from 2.5 to 3 for an increased rate of uterine rupture in the women with less time between deliveries. The biologic plausibility of this effect is related to the amount of time required for the uterine scar to heal completely.
Twin gestations
A study by Cahill et al revealed that whereas women with twin gestations are less likely to undergo a trial of labor after prior cesarean, they appear to be at no increased risk for uterine rupture. [24]
Other smaller studies examined the rate of uterine rupture in patients with twin gestation undergoing a trial of labor after cesarean delivery, and none of them demonstrated a frank rupture—though when their data were combined, 5 asymptomatic dehiscences in 151 patients were identified. [25, 26, 27]
The rate of asymptomatic uterine dehiscence in patients undergoing a trial of labor after cesarean delivery is difficult to assess because it is not commonly investigated. Thus, although the overall statistical power of the studies examining this issue in twins is not overwhelming, there is certainly no evidence suggesting a higher risk of uterine rupture in these women.
The 2017 ACOG guidelines state that TOLAC may be considered in women with one previous cesarean delivery with a low transverse incision, who are otherwise appropriate candidates for twin vaginal delivery. [6]
Mullerian anomalies
In 1999, a small series by Ravasia et al examined patients with müllerian anomalies undergoing a trial of labor after cesarean delivery and reported 2 uterine ruptures among 25 patients (8%). [28] However, both patients with uterine rupture had undergone induction with prostaglandins; therefore, it is difficult to reach any firm conclusions about the relative risk of uterine rupture in this group of patients. The sample size in this study was certainly too small to consider particular types of uterine anomalies.
Preparation
Patients with prior cesarean deliveries require special management, both antenatally and in labor and delivery. Early in their prenatal care, catalogue patients’ preexisting risk factors for both successful vaginal birth after cesarean delivery (VBAC) and uterine rupture. If uncertain about the prior hysterotomy facts, obtain the operative notes from patients’ cesarean delivery.
When a full obstetric history has been obtained, counsel patients regarding the risks and benefits of undergoing a trial of labor after cesarean delivery (TOLAC), and plan the particular mode of delivery with patients. Some providers and hospitals have particular consent forms for TOLAC that must be signed at this point.
Technique
Overview
Once the patient presents to the labor and delivery unit and is in labor, it is advisable to go through the risks and benefits of a trial of labor after cesarean delivery (TOLAC) once again. Because of possible changes in the patient’s status, these risks may have changed from the prenatal setting.
For example, if the patient presents in active labor, it seems that both her chances of failed vaginal birth after cesarean delivery (VBAC) and her risk of uterine rupture decrease. In contrast, if she is presenting for induction of labor, her chances of failed VBAC and uterine rupture both increase.
Regarding management on labor and delivery, several practices can help minimize the maternal and neonatal risk. In accordance with the guidelines of the American College of Obstetricians and Gynecologists (ACOG), have an obstetrician, anesthesiologist, and operating room team immediately available to carry out an emergency delivery.
Clinically, observe the patient closely for signs of uterine rupture. Harbingers of uterine rupture include the following:
-
Acute abdominal pain, persistent beyond contractions
-
A popping sensation
-
Palpation of fetal parts outside the uterus upon Leopold maneuvers
-
Repetitive or prolonged fetal heart rate deceleration
-
High presenting part upon vaginal examination
-
Vaginal bleeding
Treat any of these findings as a possible uterine rupture until another source for the finding has been identified. Rupture necessitates immediate delivery.
Post-Procedure
Expected outcomes
In counseling a patient with respect to the tradeoffs between a trial of labor after cesarean delivery (TOLAC) and an elective repeat cesarean delivery, several factors should be weighed. The rate of success is important: it has been demonstrated that maternal outcomes are better with successful TOLAC than with elective repeat cesarean delivery but are worse with a cesarean delivery after failed TOLAC.
A 2004 study by Landon et al found that the overall measure of morbidity was higher among women who underwent TOLAC. [13] However, among the 15,801 women who elected to have a repeat cesarean delivery, 2 maternal deaths were reported. Among the 17,898 who underwent a trial of labor, no maternal deaths due to TOLAC or uterine rupture were reported. This difference was too small to be statistically significant; however, the risk of repeat cesarean delivery to maternal morbidity and mortality should be considered.
The other important factor to consider in the setting of TOLAC or a uterine rupture is the neonatal outcomes. A large population-based study from Scotland determined that among 15,515 patients who underwent TOLAC, 7 perinatal deaths occurred as a result of uterine rupture, for a rate of 4.5 per 10,000 women. In comparison, there were no perinatal deaths due to uterine rupture among women undergoing elective repeat cesarean delivery, and the mortality rate was 0.5 per 10,000 among women laboring with no prior cesarean delivery.
A subsequent study demonstrated that among 15,338 patients at term undergoing TOLAC, there were 2 neonatal deaths and 7 cases of hypoxic-ischemic encephalopathy, for rates of 1.4 per 10,000 and 4.6 per 10,000, respectively. [13] In this series, 114 uterine ruptures occurred among these patients, yielding a neonatal death rate of 1.8% and a hypoxic-ischemic encephalopathy rate of 6.2% in patients with uterine rupture.
Finally, an important individual factor that may tip the scales for many women making the decision about whether to undergo TOLAC is whether they wish to have future pregnancies beyond the current one. Once a vaginal birth has been achieved, both the chances of future success and the risks of uterine rupture are higher.
Furthermore, with each subsequent cesarean delivery, the risks of maternal morbidity and, potentially, maternal mortality increase. Thus, for a woman who wants more children, opting for TOLAC in the current pregnancy may hold more long-term benefits than it would for a woman who is planning on a tubal ligation after delivery.
-
Vaginal birth after cesarean delivery rates.