Practice Essentials
In the United States, closed head injury, or traumatic brain injury (TBI), has an annual incidence of approximately 500 in 100,000. Around 80% of all TBI cases are categorized as mild head injuries. [1] Approximately 15% of these patients succumb to the injury upon arrival to the emergency department. [2] In 2019, nearly 61,000 deaths were attributed to a TBI. [3] Higher rates of morbidity and mortality resulting from TBI are seen in low-income and middle-income counties, making this a global health challenge. [4]
Penetrating intracranial injuries have worse outcomes than closed head injuries. Data from the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample analyzed by the Centers for Disease Control and Prevention (CDC) show that during 2018, there were 223,050 nonfatal TBI-related hospitalizations. Unintentional falls were the most common mechanism of injury leading to nonfatal TBI-related hospitalization, followed by motor vehicle crashes. Proper and consistent use of recommended restraints (ie, seatbelts, car seats, and booster seats) and, particularly for persons aged ≥75 years, learning about individual fall risk from health care providers are steps the public can take to prevent the most common injuries leading to nonfatal TBI. [5]
Closed head injuries are classified as primary and secondary. A primary injury results from the initial anatomic and physiologic insult, which is usually direct trauma to the head, regardless of cause. A secondary injury results from hypotension, hypoxia, acidosis, edema, or other subsequent factors that can secondarily damage brain tissue. Free radicals are thought to contribute to these secondary insults, especially during ischemia.
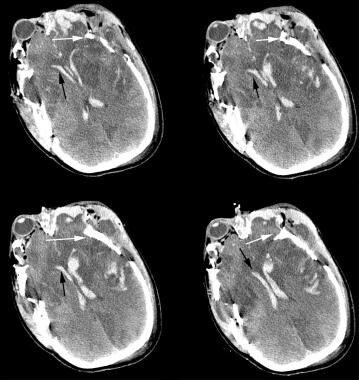
(A computed tomography scan of left frontal acute epidural hematoma is shown below.)
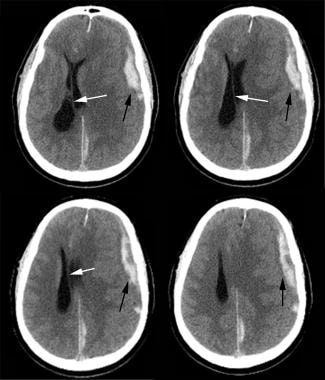 CT scan of left frontal acute epidural hematoma (black arrow) with midline shift (white arrow). Note the left posterior falx subdural hematoma and left frontoparietal cortical contusion.
CT scan of left frontal acute epidural hematoma (black arrow) with midline shift (white arrow). Note the left posterior falx subdural hematoma and left frontoparietal cortical contusion.
Head injury significantly contributes to death from trauma. Traumatic brain injury is increasingly viewed as a chronic condition, bringing long-term needs for patient and caregiver knowledge pertaining to symptom and problem management over time. The authors of a scoping review of TBI education for adult patients and families recommend further exploration of self-management training principles in long-term TBI care to assess the specific effects of education and other treatment elements. [6]
Those who survive are often left with severe neurologic deficits that may include a persistent vegetative state. A great financial burden is associated with head injuries because of lifelong disability. Injuries to the central nervous system tend to be most costly on a per-patient basis because they often result in debilitating physical, psychological, and psychosocial deficits that, in turn, require extensive long-term rehabilitation and care.
Pathophysiology
Primary injuries
Primary injuries are injuries that upon initial impact cause displacement of the brain due to direct impact, rapid acceleration-deceleration, or penetration. [7] Primary closed head injury usually causes structural changes, such as epidural hematoma, subdural hematoma, subarachnoid hemorrhage, intraventricular hemorrhage, or cerebral contusion.
Concussion
Cerebral concussion is defined as an altered mental state that may or may not include loss of consciousness that occurs as a result of head trauma. Concussion is also known as mild traumatic brain injury (MTBI). The American Academy of Neurology Grading Scale is widely used to categorize the degree of concussion.
Table 1. American Academy of Neurology Concussion Grading Scale (Open Table in a new window)
Grade 1 |
Grade 2 |
Grade 3 |
Transient confusion |
Transient confusion |
... |
No loss of consciousness |
No loss of consciousness |
Brief or prolonged loss of consciousness |
Concussive symptoms or mental status change resolving within 15 minutes |
Concussive symptoms or mental status change resolving after 15 minutes |
... |
Mild TBI or brain concussion usually results from closed brain injuries, such as when the head has been struck by an object like a bat or a fist during a fight, or when the head is affected by a nearby blast or explosion. Mild TBI causes a transient altered mental status, which can range from confusion to loss of consciousness. This cannot be diagnosed by routine computed tomography (CT) or magnetic resonance imaging (MRI). Special sequence MRI such as diffusion tensor imaging or functional MRI can lead to earlier diagnosis of concussion. [1]
Concussion is a common injury in childhood, with an estimated 1.4 million children sustaining a concussion annually in the United States. [8]
A systematic review of original research capturing people of all ages in a well-defined population area was conducted to estimate the incidence of sports-related TBI in the general population across injury severities, with the goal of informing injury prevention initiatives. Review authors reported that the incidence of sports-related TBI within hospital-based studies ranged between 3.5 and 31.5 per 100,000. One community-based study using multiple case ascertainment sources identified a higher incidence of 170 per 100,000. Sports-related TBI accounted for 1.2-30.3% of all TBI events. [9]
Sports-related concussions are frequent. The University of Michigan Health Neurosciences website reports that about 3.8 million concussions occur each year in the United States as the result of sports-related injuries. Many of these injuries go unreported and undiagnosed, resulting in mismanagement and premature return to activity, which can lead to prolonged symptoms and long-term consequences. Traumatic brain injury doubles risk of suicide and is the major determinant of acquired seizure disorders. Traumatic brain injury arising from closed head trauma significantly increases the risk of developing Alzheimer disease, Parkinson disease, and chronic traumatic encephalopathy (CTE), the last of which occurs particularly when football players and boxers are exposed to repetitive concussions. [10] Repetitive concussions may result in chronic subclinical motor dysfunction linked to intracortical inhibitory system abnormalities. [11] Parkinsonian cognitive decline due to strionigral degeneration is now a well-known consequence of repetitive concussions; cumulative diffuse axonal injury effects in the midbrain are due to increased vulnerability to shear forces in that region. Increasing a player’s neck strength may be an effective way to minimize the risk of future concussions, as studies with Hybrid III dummies seem to indicate. [12]
Cerebral contusion
Cerebral contusions are commonly seen in the frontal and temporal lobes. They may accompany skull fracture—the so-called fracture contusion. The most worrisome trait of these contusions is their tendency to expand. This usually occurs from 24 hours to as long as 7-10 days after the initial injury. For this reason, cerebral contusions are often followed with a repeat head CT scan within 24 hours after injury.
Coup injuries (contusions), which are caused by direct transmission of impact energy through the skull into the underlying brain, occur directly below the site of injury. Contrecoup injuries are caused by rotational shear and other indirect forces that occur contralateral to the primary injury. Rotational force causes the basal frontal and temporal cortices to impact or sweep across rigid aspects of the skull, the sphenoid wing, and petrous ridges. Delayed enlargement of traumatic intraparenchymal contusions and hematomas is the most common cause of clinical deterioration and death. However, progression of contusion is highly variable, and although most contusions remain unchanged for days, a few enlarge—some quite rapidly.
Several prognostic factors are known to predict contusion enlargement. The strongest of these prognostic factors is the presence of traumatic subarachnoid hemorrhage. The size of the intraparenchymal hemorrhage means that large lesions are probably in an active phase of progression at the time of the initial CT scan. The concurrent presence of a subdural hematoma is also predictive. Clinical features, such as initial Glasgow Coma Scale score (GCS; see the Glasgow Coma Scale calculator) and intracranial pressure (ICP), are not predictive of progression. The ideal time for a re-scan is unclear, although most growth seems to occur within the first 24 hours of injury. [13]
Epidural hematoma
Epidural hematoma accounts for 1% of all head trauma admissions, as depicted in the image below. [14] Epidural hematomas most commonly (85%) result from bleeding in the middle meningeal artery but may occur in locations other than in the distribution of the middle meningeal artery. Such hematomas may develop as the result of bleeding from diploic vessels injured by overlying skull fractures. [15] Epidural hematomas are often associated with a "lucid interval"—a period of consciousness between states of unconsciousness. This lucent period is presumed to end when the hematoma expands to the point that the brainstem is compromised.
 CT scan of left frontal acute epidural hematoma (black arrow) with midline shift (white arrow). Note the left posterior falx subdural hematoma and left frontoparietal cortical contusion.
CT scan of left frontal acute epidural hematoma (black arrow) with midline shift (white arrow). Note the left posterior falx subdural hematoma and left frontoparietal cortical contusion.
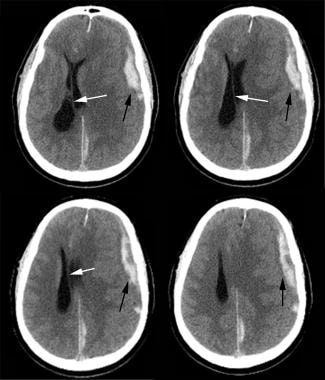
Subdural hematoma
The most common surgical intracranial lesion is the subdural hematoma. This occurs in approximately 20-40% of patients with severe injuries, as depicted in the image below. [2, 16] A surface or bridging vessel (venous) can be torn when the brain parenchyma moves during violent head motion. The bleeding that results causes a hematoma to form in the potential space between the dura and the arachnoid. A lucid interval is less likely to develop with this type of injury than with an epidural hematoma. Subdural hematoma may result from an arterial rupture as well; these hematomas are found in the temporoparietal region and differ in form from those caused by the bridging vein rupture, which typically are seen in the frontoparietal parasagittal region. Hematoma thickness and midline shift of the brain are often analyzed; when midline shift exceeds hematoma thickness (positive displacement factor), the prognosis is poorer. [17]
 CT scan of left frontoparietal acute subdural hematoma (black arrow). Note the moderate amount of midline shift.
CT scan of left frontoparietal acute subdural hematoma (black arrow). Note the moderate amount of midline shift.
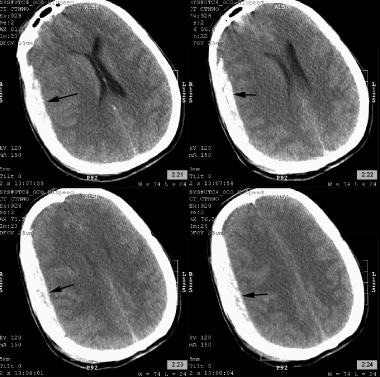
Intraventricular hemorrhage
Intraventricular hemorrhage is another intracerebral lesion that often accompanies other intracranial hemorrhages, as depicted in the image below. Intraventricular blood is an indicator of more severe head trauma. Intraventricular blood predisposes the patient to posttraumatic hydrocephalus and intracranial hypertension, which may warrant placement of an intraventricular catheter (if emergent drainage is needed) or a ventriculoperitoneal shunt for chronic hydrocephalus.
 CT scan of bilateral acute intraventricular hemorrhages (black arrow). Note the comminuted skull fractures that involve bilateral frontal, temporal, and parietal bones (white arrow). Note the ischemic changes in both frontal lobes, subarachnoid hemorrhages in the intrahemispheric fissure and left frontal lobe, and multiple intraparenchymal hemorrhages in both frontal poles.
CT scan of bilateral acute intraventricular hemorrhages (black arrow). Note the comminuted skull fractures that involve bilateral frontal, temporal, and parietal bones (white arrow). Note the ischemic changes in both frontal lobes, subarachnoid hemorrhages in the intrahemispheric fissure and left frontal lobe, and multiple intraparenchymal hemorrhages in both frontal poles.
Traumatic subarachnoid hemorrhage
Subarachnoid hemorrhage is most commonly caused by trauma and results from tearing of small capillaries, with blood subsequently entering into the subarachnoid space. It commonly occurs over the convexity but may be seen in the basal cistern secondary to aneurysmal rupture. [1]
Diffuse axonal injury
One of the consistent pathologies associated with both clinical and experimental TBI is axonal injury, especially following mild TBI (or concussive injury). [18] Despite the absence of any intracranial mass lesion or history of hypoxia, some patients remain unconscious after a TBI. Brain MRI studies have demonstrated a clear correlation between white matter lesions and impairment of consciousness after injury. The deeper the white matter lesion, the more profound and persistent the impairment of consciousness. [19]
The usual cause for persistent impairment of consciousness is the condition referred to as diffuse axonal injury (DAI), as depicted in the image below. Approximately 30-40% of individuals who die from TBI reveal postmortem evidence of DAI and ischemia. [20] This type of injury commonly results from traumatic rotation of the head, with mechanical forces that act on the long axons, leading to axonal structural failure. Diffuse axonal injury is caused by an acceleration injury—not by contact injury alone. The brain is relatively incompressible and does not tolerate tensile or shear strain well. Slow application of strain is better tolerated than rapid strain. The brain is most susceptible to lateral rotation and tolerates sagittal movements best. [21]
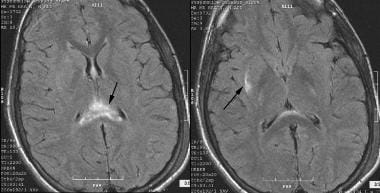 MRI of the brain that shows diffuse axonal injury (DAI) and hyperintense signal in the corpus callosum (splenium), septum pellucidum, and right external capsule.
MRI of the brain that shows diffuse axonal injury (DAI) and hyperintense signal in the corpus callosum (splenium), septum pellucidum, and right external capsule.
Studies suggest that the magnitude of rotational acceleration needed to produce DAI requires the head to strike an object or surface. These factors also increase the likelihood that DAI will be accompanied by other intracranial lesions. [21] Mechanical forces physically dissect the axons into proximal and distal segments. If a sufficient number of axons are involved, profound neurologic deficits and unconsciousness may ensue. Characterization of DAI using diffusion tensor magnetic resonance imaging (DTI) may provide a useful set of outcome measures for preclinical and clinical studies. [22]
One study found that DAI and younger age may contribute to increased risk of developing dysautonomia. [23]
These same forces may act on the cerebral circulation, causing disruption of vessels and various forms of micro–intracerebral hemorrhage and macro–intracerebral hemorrhage, including Duret hemorrhage, which is commonly lethal when it occurs in the brainstem. Duret hemorrhage of the midbrain and pons is a small punctate hemorrhage that is often caused by arteriole stretching during the primary injury, as depicted in the image below. Duret hemorrhage may also occur during transtentorial herniation as a secondary injury when arterial perforators are compressed or stretched.
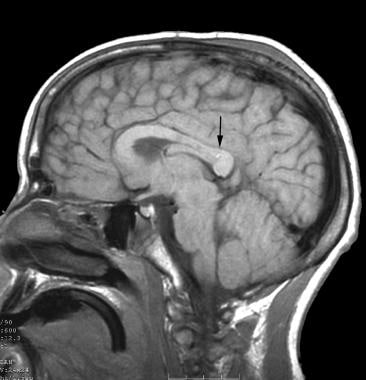 MRI of the brain (sagittal view) that shows a Duret hemorrhage in the splenium of the corpus callosum.
MRI of the brain (sagittal view) that shows a Duret hemorrhage in the splenium of the corpus callosum.
Secondary injuries
Secondary injuries consist of changes that occur after the initial insult. [7] Secondary insult can take many forms.
-
Secondary intracranial insults to the brain include the following: hemorrhage, ischemia, edema, raised intracranial pressure (ICP), vasospasm, infection, epilepsy [24] , hydrocephalus.
-
Secondary systemic insults to the brain include the following: hypoxia, hypercapnia, hyperglycemia, hypotension, severe hypocapnia, fever, anemia, hyponatremia.
Management of acute closed head injury is intended to prevent secondary injuries while preserving neurologic functions that have not been damaged by the primary injury.
Posttraumatic vasospasm can cause ischemic damage after severe TBI; parenchymal contusions and fever are risk factors. Diffuse mechanical injury and activation of inflammatory pathways may be secondary mechanisms for this vasospasm. Patients with parenchymal contusions and fever may benefit from additional screening. [25]
Brain herniation
Herniation of the brain occurs as the result of increased ICP. Types of herniation include the following:
-
Uncal transtentorial: compression of parasympathetic fibers running with the third cranial nerve; seen as ipsilateral fixed and dilated pupil with contralateral hemiparesis.
-
Central transtentorial: midline lesions such as lesions of the frontal or occipital lobes or vertex; seen as bilateral pinpoint pupils, bilateral Babinski signs, and increased muscle tone, followed by fixed midpoint pupils with prolonged hypertension and decorticate posturing.
-
Cerebellar tonsillar: compression on the lower brainstem and upper cervical spinal cord; seen as pinpoint pupils, flaccid paralysis, and sudden death.
-
Upward posterior fossa/cerebellar: displacement of the cerebellum in an upward direction through the tentorial opening; seen as conjugate downward gaze with absence of vertical eye movement and pinpoint pupils. [7]
Cerebral ischemia
Cerebral ischemia refers to inadequate oxygen perfusion to the brain resulting from hypoxia or hypoperfusion. The undamaged brain tolerates low levels of partial pressure of oxygen in arterial blood (PaO2) better than the severely injured brain. Traumatized brain tissues are very sensitive to even moderate hypoxia (90 mm Hg). Gordon and Ponten proposed 2 explanations for this phenomenon: (1) Respiratory alkalosis may shift the oxygen-hemoglobin curve to the left, thereby increasing the affinity of hemoglobin to oxygen and decreasing the ease of oxygen release; and (2) uneven cerebral blood flow (CBF) may result from focal vasospasm with loss of focal autoregulation in the area of injured brain tissue. [21] Approximately one third of patients with severe head injury experience ischemic levels of CBF. [26]
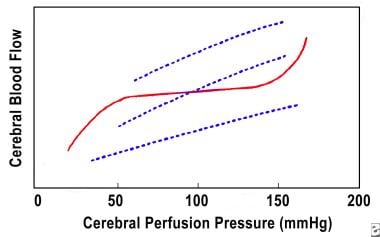
Cerebral blood flow is normally kept constant over a range (about 50-150 mm Hg) of cerebral perfusion pressure, as depicted in the image below. This is made possible by adjustments in vascular tone known as autoregulation (solid line). In patients with brain trauma, this autoregulation may malfunction and CBF may become dependent on cerebral perfusion pressure (CPP) (dashed lines). Autoregulation is absent, diminished, or delayed in 50% of patients with severe head injury. [26] The lowest CBF values occur within the first 6-12 hours after injury. [27, 28, 29, 30] The overall outcome of patients who experience ischemia is much worse than that of initially nonischemic patients. [26, 31, 32] The initial ischemia is thought to cause permanent irreversible damage, even if CBF is eventually optimized. Xenon CT scan is used to measure CBF as part of the armamentarium for diagnosis and treatment of abnormalities in CBF.
Brain edema
Brain edema is another form of secondary injury that may lead to elevated ICP, frequently resulting in increased mortality. Brain edema is categorized as vasogenic or cellular (or cytotoxic) edema.
Vasogenic edema occurs when a breach in the blood-brain barrier allows water and solutes to diffuse into the brain. Most of this fluid accumulates in the white matter and can be observed on head CT scan as hypodense white matter (on T1-weighted images) or on T2-weighted MRI as a bright signal area. The mechanism of cellular (cytotoxic) edema is less clear. Theories include increased uptake of extracellular potassium by injured brain cells or transport of bicarbonate (HCO3-) and hydrogen (H+) for chloride (Cl-) and sodium (Na+) by injured brain tissue as the mechanism of insult. [21]
Diffusion-weighted MRI has been used to evaluate the apparent diffusion coefficient (ADC). Higher ADC values are associated with vasogenic edema, and lower ADC values with a predominantly cellular form of edema. Regional measurements of ADC have been computed for patients with focal and diffuse injury. Researchers have concluded that the brain swelling observed in patients with TBI appears to be predominantly cellular, as signaled by low ADC values in brain tissue with high levels of water content. [33]
Epidemiology
The male-to-female ratio for TBI is 2:1. The Centers for Disease Control and Prevention (CDC) has estimated that annually, about 1.5 million US individuals survive a TBI. Among these, approximately 230,000 are hospitalized. In the year 2000, 10,958 cases of TBI were diagnosed. By 2015, this number had jumped to 344,030. Mortality across all TBI severities is approximately 3%, and morbidity is more difficult to estimate. [1] Although only 10% of TBI cases occur in the elderly population, it accounts for up to 50% of TBI-related deaths. [7]
In the United States, closed head injury, or TBI, has an annual incidence of approximately 500 in 100,000. Around 80% of all TBI cases are categorized as mild head injuries. [1] Approximately 15% of these patients succumb to the injury upon arrival to the emergency department. [2] In 2019, nearly 61,000 deaths were attributed to TBI. [3] Higher rates of morbidity and mortality resulting from TBI are seen in low-income and middle-income counties, making this a global health challenge. [4]
Data from the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample analyzed by the CDC show that, during 2018, there were 223,050 nonfatal TBI-related hospitalizations; rates for persons aged 75 years or older were approximately 3 times higher than that for persons aged 65-74 years, and the age-adjusted rate for males was approximately double that for females. Unintentional falls were the most common mechanism of injury leading to nonfatal TBI-related hospitalization, followed by motor vehicle crashes. Proper and consistent use of recommended restraints (ie, seatbelts, car seats, and booster seats) and, particularly for persons aged 75 years or older, learning about individual fall risk from health care providers are steps the public can take to prevent the most common injuries leading to nonfatal TBI. [5]
The CDC estimates that 166 TBI-related deaths occur every day in the United States. [34]
Traumatic injuries remain the leading cause of death in children and in adults aged 45 years or younger. Traumatic brain injury resulting from military combat, sports, violence, falls, and vehicular accidents is a major cause of long-term physical, cognitive, and psychiatric dysfunction. Psychiatric disorders associated with TBI include depression, anxiety, and substance use disorder—all with significant implications for post-TBI recovery and rehabilitation. [35]
Head injury is an important cause of morbidity and mortality in children and young adults. Head injury, even closed head injury without visible violation of the globe or orbits, is associated with multiple sight-threatening complications. One such entity is traumatic optic neuropathy. [36]
Incidence varies by age, but children and young people experience closed head trauma more often than older populations. Older adults are more likely to die from a TBI than are those in other age groups. Although falls are the leading cause of nonfatal TBI, fall-related TBI deaths have increased, particularly in adults older than 75 years. [34]
In the United States, around 1.7 million people suffer TBI; older adolescents (aged 15-19 yr) and older adults (aged ≥65 yr) are most likely to sustain a TBI. Moderate to severe TBI is a primary cause of injury-induced death and disability. [1]
Prognosis
The prognosis for TBI is affected by many factors, including (1) type of injury (penetrating vs blunt), (2) severity of injury and accompanying neurologic deficit, (3) patient age, (4) comorbid conditions, and (5) secondary injuries.
Each year in the United States, nearly 52,000 deaths occur as the result of TBI. Individuals who arrive for treatment with low Glasgow Coma Scale (GCS) scores have the worst outcomes. Even those who survive have prolonged recovery, and some are left with residual neurologic deficits. Complete recovery can take months or even years. [1]
It is interesting to note that many questions continue to demand answers. These include prognosis, permanency of symptoms, best short-term and long-term treatment strategies, and whether literature on sports-related TBI can be used as a guide. Imaging and therapeutic intervention research are under way in the hope of delivering better patient outcomes. The prognosis for patients with TBI depends on initial GCS score and neurologic deficits at presentation. Patients with a GCS less than 12 usually have a long recovery, and many continue to have residual neuropsychiatric deficits. [1]
The GCS has been reported to be most predictive of neurologic outcomes at 1 year after severe head injury, and 24-hour GCS score is the strongest predictor of cognitive recovery at 2 years after injury in patients with moderate to severe head injury. [37, 38]
In a study of mortality including 44 elderly patients (aged ≥75 yr) who underwent an operation for acute subdural hematoma, patients who were independent had 1-year mortality of 42% versus 69% for dependent patients (median follow-up, 4.2 yr; range, 2.5-6.4 yr). Patients taking antithrombotics had 56% mortality after the first postoperative year versus 30% for those not taking antithrombotics. All patients with an admission GCS score of 3-8 died within the first postoperative year if they had used antithrombotics or were dependent before the injury. [39]
Patients in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) treated via craniotomy or craniectomy for subdural hemorrhage were studied for mortality, other adverse outcomes, and length of hospital stay. The most common individual adverse events were death (18% of patients died within 30 days of surgery) and intubation longer than 48 hours (19%). In total, 34% experienced a serious adverse event other than death, 8% returned to the operating room, and average hospital length of stay was 9.8±9.9 days. Increased mortality was associated with gangrene, ascites, American Society of Anesthesiologists (ASA) physical status class 4 or higher, coma, and bleeding disorders. Reduced mortality was associated with age younger than 60 years. [40]
A study of patients with chronic subdural hematoma found that neurologic status on admission was the best predictor of outcome. In addition, age, brain atrophy, thickness and density of hematoma, subdural accumulation of air, and antiplatelet and anticoagulant therapy were found to correlate significantly with prognosis. [41]
Pupillary function before and after resuscitation has some predictive value. In patients who initially have bilateral unreactive pupils (and whose pupils do not regain function), approximately 85% die or remain in a persistent vegetative state, as compared to 15% of those who regain pupillary function. [21]
Age also influences overall outcome. Infants and very young children tend to have a higher mortality rate. This is most likely due to the nature of their injuries and associated prolonged episodes of apnea. The mortality rate from closed head injury remains relatively constant until after the age of 35 years, at which time it begins to rise dramatically. [42]
The development and duration of fever is clearly associated with worse prognoses. [14]
Insulin deficiency due to diabetes mellitus (DM) has been found to impart increased risk for mortality in patients with moderate to severe TBI compared to patients without DM (14.4% vs 8.2% ). [43]
-
CT scan of left frontal acute epidural hematoma (black arrow) with midline shift (white arrow). Note the left posterior falx subdural hematoma and left frontoparietal cortical contusion.
-
CT scan of left frontoparietal acute subdural hematoma (black arrow). Note the moderate amount of midline shift.
-
CT scan of bilateral acute intraventricular hemorrhages (black arrow). Note the comminuted skull fractures that involve bilateral frontal, temporal, and parietal bones (white arrow). Note the ischemic changes in both frontal lobes, subarachnoid hemorrhages in the intrahemispheric fissure and left frontal lobe, and multiple intraparenchymal hemorrhages in both frontal poles.
-
MRI of the brain that shows diffuse axonal injury (DAI) and hyperintense signal in the corpus callosum (splenium), septum pellucidum, and right external capsule.
-
MRI of the brain (sagittal view) that shows a Duret hemorrhage in the splenium of the corpus callosum.
-
Cerebral blood flow/cerebral perfusion pressure chart.