Background
Cervical cytology by Papanicolaou test (Pap smear) is the basis for cervical cancer screening in the United States. The 2009 American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin on Cervical Cytology Screening recommends that screening be initiated at age 21, regardless of age of onset of sexual intercourse. [1] Screening is recommended every 2 years until age 30. Thereafter, screening frequency may be decreased to every 3 years following 3 consecutive negative Papanicolaou test results for intraepithelial dysplasia and malignancy. Screening may be discontinued in low-risk women at age 65-70. The Bethesda System for reporting cervical and vaginal cytologic diagnoses was revised by the National Cancer Institute in 2001. [2]
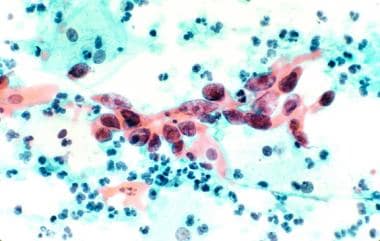
The images below illustrate cell cervical carcinoma.
The American Society for Colposcopy and Cervical Pathology (ASCCP) has developed guidelines for the management of women with cervical cytologic abnormalities. Evaluation following an abnormal finding on a Papanicolaou test may include repeat cytology, colposcopic examination with directed biopsies, endocervical curettage (ECC), and human papillomavirus (HPV) subtyping depending on the abnormal finding.
Biopsy-proven cervical intraepithelial neoplasia (CIN) in the absence of invasive cancer can be treated by destructive or excisional techniques. These techniques include local excision, cryosurgery, laser vaporization, loop electrode excision procedure (LEEP), cone biopsy, trachelectomy, and hysterectomy.
This article will review the role of cryosurgery in the treatment of preinvasive cervical neoplasia.
History of the Procedure
The modern recognition of cervical dysplasia as a premalignant disease of the uterine cervix dates back to the early 1940s, when Papanicolaou and Traut first described how exfoliated cells could be used to screen for cervical cancer and its precursors. The First International Congress of Exfoliative Cytology was convened in the 1960s, and the new age of screening for premalignant cervical disease began. Prior to this time, investigators such as Sir John Williams in the 1880s and T.S. Collen in 1900 recognized that premalignant disease often is found adjacent to invasive cancers of the cervix. Thus, the idea that invasive squamous cell cancers of the uterine cervix develop from precursor lesions was introduced.
Since the 1960s, many advances have been made in both diagnosis and management of premalignant diseases of the uterine cervix. Until the early 1970s, cervical cone biopsy and hysterectomy were the mainstays of treatment. Investigators such as Crisp [3] and Townsend and Ostergard [4] attempted to find methods of treatment that would obviate the need for extensive surgery and hospitalization. These investigators were the first to study the role of cryosurgery in managing selected patients with preinvasive cervical disease.
Problem
Because CIN is a premalignant condition, understanding the risk of progression to malignant disease is important in order to recommend treatment options. These recommendations depend on the abnormality and individual patient risk factors. Management of this spectrum of premalignant conditions may vary by provider and is summarized in an ACOG Practice Bulletin on Management of Cervical Cytology and Histology published in 2008. [5] Rates of progression for biopsy-proven CIN are summarized in the Table.
Table. Rates of Progression of CIN [6] (Open Table in a new window)
CIN |
% Regression |
% Persistence |
% Progression |
CIN 1 |
57 |
32 |
11 |
CIN 2 |
43 |
35 |
22 |
CIN 3 |
32 |
56 |
12 |
More recently, investigators have reported even higher rates of spontaneous regression of CIN1 among young women and adolescents, with 90-100% regression over 24-36 month follow-up. [7, 8, 9]
Epidemiology
Frequency
Worldwide, cervical cancer is the second leading cause of cancer death in women. In the United States, the American Cancer Society predicted 13,170 new cases of invasive cervical cancer and 4,250 deaths due to cervical cancer in 2019. [10] The average age at diagnosis is between ages 35 and 44 years; it is rarely diagnosed in woman younger than 20 years.
In the United States, cervical cancer incidence and mortality rates have declined dramatically with the use of Pap test screening and treatment of preinvasive disease. [11, 12] In a 2001 study, an encouraging 88.3% of women aged 18-44 years reported having had a Pap test in the past 3 years. [13]
The frequency of abnormal Papanicolaou test results and CIN varies by the population tested and the methodology of testing, and ranges from 1.5-6%. [14] The frequency of dysplasia based on the Kaiser Pemanente Northwest database is 1.2 per 1,000 women for CIN 1 and 1.5 per 1,000 women for CIN 2/3. [15]
Etiology
Risk factors for preinvasive neoplastic lesions of the cervix include the following:
-
HPV infection (especially 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, 73, which are known high-risk subtypes [16] )
-
History of abnormal Pap test results or dysplasia
-
Cigarette smoking
-
Early age at first coitus
-
Multiple sexual partners
-
History of sexually transmitted diseases
-
Immunodeficiency, including HIV infection
-
Oral contraceptive use
-
Low socioeconomic status
-
Multiparity
-
African American, Hispanic, and Southeast Asian heritage
Pathophysiology
The concept of a continuum of squamous cell carcinoma precursors is the basis for the CIN classification for abnormal cervical histology results. [17] Importantly, both CIS and dysplasia are known to consist of monoclonal cell lines with an aneuploid nuclear content. [18]
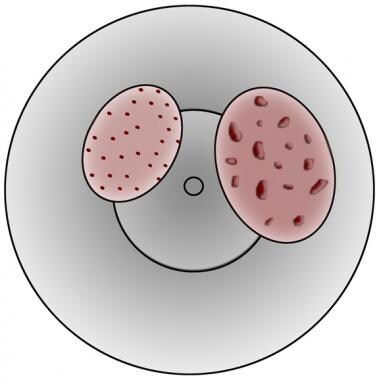
The CIN system differentiates mild (CIN 1), moderate (CIN 2), and severe dysplasia/CIS (CIN 3) based on the proportion of abnormal cells relative to the full epithelial thickness. The Bethesda System simplifies this to describe low-grade squamous intraepithelial lesion (LSIL) and high-grade squamous intraepithelial lesion (HSIL), combining CIN 2 and CIN 3 into a single category due to similar risk of progression and prognosis. The image below illustrates both fine and coarse punctation in cervical lesions.
The impact of HPV on cervical dysplasia and squamous cell carcinoma is an area of active clinical and research interest. HPV is an epitheliotropic double-stranded DNA virus. The HPV DNA is integrated into host chromosomes at specific loci. The E7 early protein binds to inactivate the retinoblastoma susceptibility gene, and the E6 early protein binds to p53. The affected epithelial cell then undergoes unregulated mitosis. [19] HPV subtypes 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, and 58 are the types most frequently isolated from carcinomas and severe dysplasia. [20] These HPV subtypes generally are not isolated from condyloma or CIN 1 lesions. [21] On this basis, investigators use HPV genotyping as a method to determine treatment options for patients with abnormal Pap tests results and colposcopic findings.
Indications
Candidates for cryotherapy include patients with squamous CIN on biopsy who meet the following requirements:
-
Satisfactory colposcopic examination, with complete visualization of the transformation zone
-
Lesion identified and fully visualized
-
Biopsy consistent with cytology
-
Invasive carcinoma ruled out by biopsy
-
Negative ECC
Relevant Anatomy
The uterine cervix (from the Latin cervix, meaning neck) is the most distal portion of the uterus and extends into the upper vagina. The portio vaginalis is the location of the external os, the opening to the cervical canal and uterine cavity. The cervix consists of fibrous, muscular, and elastic tissue. It is lined by both columnar and squamous epithelium.
The squamocolumnar junction is found at the delineation between the stratified squamous epithelium and the columnar epithelium of the endocervix. Over time the columnar epithelium, which may be found on the ectocervix, is replaced by the metaplastic squamocolumnar junction. This junctional area is termed the transformation zone and is the site where most squamous neoplasia arises.
The purpose of cryosurgery is to destroy dysplastic cells that arise in this transformation zone by effecting cryonecrosis.
Contraindications
See the list below:
-
Unsatisfactory colposcopy
-
Lesion not fully visible or extending beyond the range of the cryotherapy probe
-
Colposcopically directed biopsy not consistent with cytology
-
ECC positive for CIN
-
Biopsy consistent with or suspicious for invasive carcinoma [22]
-
Glandular epithelial dysplasia or adenocarcinoma in situ
-
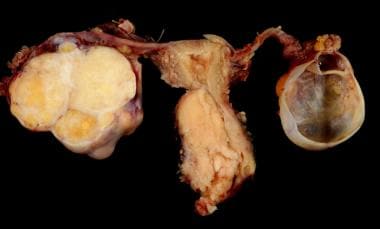
Cervical carcinoma with adnexa.
-
Squamous cell cervical carcinoma.
-
Punctation in cervical lesions. Left is fine, right is coarse (likely high grade or invasive).