First Trimester
What are the first symptoms of pregnancy?
Missing a period is usually the first signal of a new pregnancy, although women with irregular periods may not initially recognize a missed period as pregnancy. During this time, many women experience a need to urinate frequently, extreme fatigue, nausea and/or vomiting, and increased breast tenderness. All of these symptoms can be normal. Most over-the-counter pregnancy tests are sensitive 9-12 days after conception, and they are readily available at most drug stores. Performing these tests early helps to allay confusion and guesswork. A serum pregnancy test (performed in a provider's office or laboratory facility) can detect pregnancy 8-11 days after conception.
How long after conception does the fertilized egg implant?
The fertilized conceptus enters the uterus as a 2- to 8-cell embryo and freely floats in the endometrial cavity about 90-150 hours, roughly 4-7 days after conception. Most embryos implant by the morula stage, when the embryo consists of many cells. This happens, on average, 6 days after conception. However, there is great variance in the time of implantation. It can occur on days 16-30 of the menstrual cycle. The new embryo then induces the lining changes of the endometrium, which is called decidualization. It then rapidly begins to develop the physiologic changes that establish maternal-placental exchange. Prior to this time, medications ingested by the mother typically do not affect a pregnancy.
What is the most accurate pregnancy test to use?
All pregnancy tests work by detecting human chorionic gonadotropin (hCG). This hormone is produced by the syncytiotrophoblast beginning on the day of implantation, and it rises in both the maternal blood stream and the maternal urine fairly quickly. It can be detected in both the blood and urine by about 8-9 days after conception.
There are a few types of pregnancy tests that include professional quantitative serum hCG tests, point-of-care qualitative serum hCG tests, and urine tests for hCG. The serum hCG test is the most sensitive and specific, with laboratory published sensitivities of 1, 2 or 5 mIU/mL. Urine pregnancy tests differ in their sensitivity and specificity, which are based on the hCG units set as the cutoff for a positive test result, usually 2-5 mIU/mL.
Urine pregnancy testing kits can produce positive results at the level of 20 mIU/mL, which is 2-3 days before most women expect their next menstrual period. The kits are very accurate, widely available, and can be completed in about 3-5 minutes. The kits all use the same technique—recognition by an antibody of the beta subunit of hCG.
However, falsely high readings of the hCG hormone can occur in cases of hydatidiform molar pregnancies or other placental abnormalities. Also, test results can remain positive for pregnancy weeks after a pregnancy termination, miscarriage, or birth. In addition, false-negative test results can also occur from incorrect test preparation, urine that is too dilute, or interference by several medications.
Further complicating the science of pregnancy detection is that pregnancies which fail to properly implant can lead to brief increases in hCG levels, creating a false-positive result. Many over-the-counter (OTC) tests make claims such as “99% accurate on the first day of your missed periods.” It is important to advise women that these early results should not be considered definitive; when using home pregnancy tests, it is best to wait 1 week after a missed period for a more accurate result. [1]
Serum pregnancy tests can be performed by a variety of methods. The enzyme-linked immunosorbent assay (ELISA) is the most popular in many clinical laboratories. This test is a determination of total beta-hCG levels. It is performed using a monoclonal antibody to bind to the hCG; a second antibody is added that also interacts with hCG and emits color when doing so. This form of ELISA is commonly called a "sandwich" of the sample hCG. Radioimmunoassay (RIA) is still used by some laboratories. This test adds radiolabeled anti-hCG antibody to nonlabeled hCG of the blood sample. The count is then essentially determined by the amount of displacement of the radiolabeled sample.
The hCG level doubles approximately every 2 days in early pregnancy. However, it should be noted that even increases of only 33% can be consistent with healthy pregnancies. These values increase until about 60-70 days and then decrease to very low levels by about 100-130 days and never decrease any further until the pregnancy is over.
Is cramping during pregnancy normal?
Early in pregnancy, uterine cramping can indicate normal changes of pregnancy initiated by hormonal changes; later in pregnancy, it can indicate a growing uterus. Cramping that is different from previous pregnancies, worsening cramping, or cramping associated with any vaginal bleeding may be a sign of ectopic pregnancy, threatened abortion, or missed abortion.
Other physical effects that are normal during pregnancy, and not necessarily signs of disease, include nausea, vomiting, increase in abdominal girth, changes in bowel habits, increased urinary frequency, palpitations or more rapid heartbeat, upheaving of the chest (particularly with breathing), heart murmurs, swelling of the ankles, and shortness of breath. [2]
Why do pregnant women feel tired?
Fatigue in early pregnancy is very normal. Many changes are occurring as the new pregnancy develops, and women experience this as fatigue and an increased need for sleep. Lower blood pressure level, lower blood sugar levels, hormonal changes due to the soporific effects of progesterone, metabolic changes, and the physiologic anemia of pregnancy all contribute to fatigue. Women should check with their health care provider to determine if an additional work up, prenatal vitamin changes, and/or supplemental iron would be beneficial.
Second Trimester
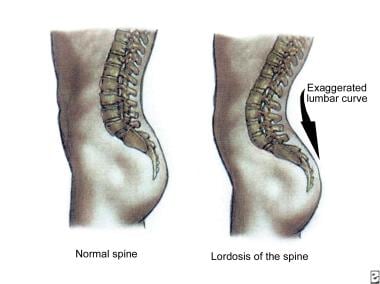
When do the postural changes of pregnancy occur?
Women experience a progressive increase in the anterior convex shape of the lumbar spine during pregnancy. This change, termed lordosis, helps keep the center of gravity stable and over the legs as the uterus enlarges (see below). Late in pregnancy, aching, weakness, and numbness of the arms may occur secondary to compensatory anterior positioning of the neck and hunching of the shoulders in positional response to exaggerated lordosis. These positional responses put traction on the ulnar and median nerves, resulting in the previously mentioned symptoms.
In pregnancy, relaxin is secreted by the corpus luteum, the placenta, and part of the decidual lining of the uterus. It is thought to cause remodeling of the connective tissue of the reproductive tract and especially induce biochemical changes of the cervix.
Although relaxin levels during pregnancy are more than 10-fold higher than nonpregnant levels, experts do not currently believe that this hormone has a direct effect on actual ligamentous loosening. Joint laxity and shifting of the center of gravity can contribute to an increase in gait unsteadiness; these changes are most exaggerated in later pregnancy.
More than 50% of gravid females complain of back pain during pregnancy, which may also be due to sacroiliac joint dysfunction or paraspinous muscle spasm. About 4-6 per 1000 women will have scoliosis. This is not accompanied by any functional osteoporosis, although pregnancy is a very high bone turnover state, approximately equivalent to double the bone loss rates of a menopausal female, reversibly losing about 2% of bone during the first 20 weeks of gestation. Spinal changes are usually not severe enough to affect the pregnancy or the lung's functional capacity. Also, the pregnancy rarely affects the degree of lateral curvature in these cases of scoliosis. If a pregnant patient has had correction with prior Harrington distraction rod insertion, the pregnancy, labor, and delivery are not typically affected. The epidural space may be distorted, and some anesthesiologists may refuse to place epidural anesthetics in these patients.
When do changes in the pelvic contour occur?
The pelvis continues to grow until about 3 years after menarche, which is why it is more common for younger women, and women sooner after menarche to have greater risk for obstructed labor due to the relative size discrepancy between the fetal head and the maternal pelvis. Relaxin was also thought to loosen pelvic ligaments when secreted from the ovaries, contributing to enlargement of the pelvis, but this is not proven in human pregnancies. The symphysis pubis can enlarge from about 3-4 mm in nulliparas to about 4.5 mm (or as much as 8 mm) in multiparas, but during gestation itself the average separation is about 7-8 mm.
When is fetal movement usually felt?
Most women feel the beginnings of fetal movement before 20 weeks' gestation. In a first pregnancy, this can occur around 18 weeks' gestation, and in following pregnancies it can occur as early as 15-16 weeks' gestation. Early fetal movement is felt most commonly when the woman is sitting or lying quietly and concentrating on her body. It is usually described as a tickle or feathery feeling below the umbilical area. The point at which a woman feels the baby move is termed quickening.
Placental location can impact the timing of quickening. An anterior placenta can "cushion" against fetal movement and delay maternal detection of fetal movements. As the fetus grows larger, the fetal movement feelings become stronger, regular, and easier to detect. While there is no absolute number that indicates fetal well-being, typical guidance may include that fetuses should move approximately 4 times an hour as they get larger, and some clinicians advise patients to count fetal movements to follow fetal well-being.
What kind of breast changes are normal during pregnancy?
Pregnancy-related breast changes include growth and enlargement, tenderness, darkening of the nipples, and darkened veins due to increased blood flow. In addition, small raised bumps (Montgomery tubercles) appear around the areola in mid-pregnancy.
Third Trimester
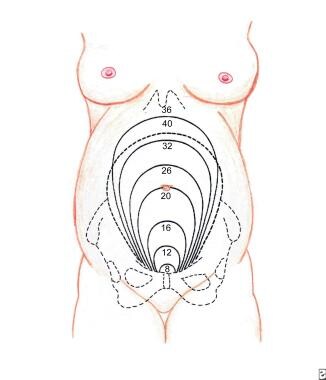
How much does the uterus grow during pregnancy?
The uterus grows from an organ that weighs 70 g with a cavity space of about 1 mL to an organ that weighs more than 1000 g that can accumulate a fluid area of almost 20 L. The shape also evolves during pregnancy from the original pearlike shape to a more round form, and it is almost a sphere by the early third trimester. By full term, the uterus becomes ovoid. The uterus is completely palpable in the abdomen (not just by pelvic examination) at about 12-14 weeks' gestation. After 20 weeks' gestation, most women begin to appear pregnant upon visual examination.
See below.
Is it normal to secrete milk from the breast prior to delivery?
Galactorrhea (milk secretion from the nipple) is the product of the combined effects of prolactin, glucocorticoids, progesterone, and human placental lactogen. Galactorrhea is not uncommon in the first trimester, although it usually does not occur until milk let-down soon after delivery. At that time, the high levels of progesterone, which block milk excretion, drop with the delivery of the placenta. In mid-pregnancy a woman reaches lactogenesis stage I and she is able to secrete colostrum.
Early galactorrhea does not mean that a woman will produce less milk after delivery. Some women notice secretions beginning before the fifth month of pregnancy. Many women find they spontaneously leak or express some fluid by the ninth month.
Early milk secretion, known as colostrum, is watery and pale. Colostrum has more protein and lower fat levels than mature milk.
Lactogenesis stages II and III occur postpartum and form more mature milk.
Physiological Adaptations to Pregnancy
Why do women undergo skin pigmentation changes during pregnancy?
Pigmentation changes are directly related to melanocyte-stimulating hormone (MSH) elevations during pregnancy. Some evidence suggests that elevated estrogen and progesterone levels cause hyperpigmentation in women. This is typically evident in the nipples, umbilicus, axillae, perineum, and linea alba, which darkens enough to be considered a linea nigra. More than 90% of patients have skin darkening. Facial darkening, called melasma, is a diffuse macular facial hyperpigmentation. When melasma occurs as a result of pregnancy, it is known as chloasma. This is due to the pigment being deposited in the epidermis itself. The distribution is usually malar but can be central or mandibular. Ultraviolet light exposure intensifies melasma and appropriate sunscreen decreases the effect. Because it is related to the hormones of pregnancy, it lessens with delivery.
Other pigmentation changes, such as palmar erythema, pseudoacanthosis nigricans, vulvar or dermal melanocytosis, or postinflammatory hyperpigmentation secondary to specific dermatologic conditions of pregnancy, are fairly common as well.
See Diagnosing Dermatoses in Pregnant Patients: 8 Cases to Test Your Skills, a Critical Images slideshow, for help identifying several types of cutaneous eruptions associated with pregnancy.
Do ocular changes occur in pregnancy?
Physiologic changes of pregnancy create stress to all of the mother's body systems, including the eye and visual system. Pregnant women often report dry eyes, which is thought to be due disruption of the lacrimal acinar cells by pregnancy-enhanced hormones. Some women also find it difficult to wear contact lenses while pregnant as a result of corneal thickening and an increase in curvature. These changes can also affect the corneal refractive index. It is important to advise women these changes are transient, and they should wait several weeks postpartum before seeking a new prescription for glasses or fittings for new contact lenses.
Pregnancy can also impact preexisting ocular diseases. The risk of development and progression of diabetic retinopathy is most common in this setting. Although diabetic retinopathy is associated with a high rate of postpartum regression, it is important to counsel women about the risk. [3]
Why does acne increase during pregnancy?
Studies show a variable effect of acne in pregnancy. If treatment regimens that were working prior to pregnancy were abandoned, the patient can have initial flares that are not directly related to the pregnancy. Some studies show that as many as a third of cases actually improve in pregnancy, but most women will report some worsening. Progesterone, which has some androgenic components, is increased during pregnancy, resulting in more secretions from the skin glands.
Postpartum, some women will get acne for the first time (called postgestational acne). Maintaining hydration should help. Women should consult their doctor if a topical medication is needed. Azelaic acid, topical erythromycin or clindamycin, and oral erythromycin are all safe. Although topical tretinoin has not been reported to cause risk, no studies have established its safety and it should be avoided. Tetracyclines are contraindicated during pregnancy. Appropriate cleansing with mild abrasion aids has been found to be helpful.
Will changes in headache patterns occur during pregnancy?
For most women, headaches remain unchanged during pregnancy. Some women improve, but some may worsen. Because migraines have a hormonal component, many women's migraines improve with increasing estrogen levels, such as those that occur during pregnancy. For women whose conditions remain unchanged or worsen, treatment options are limited, especially in the first trimester. Some clinicians suggest acetaminophen, narcotics, and antiemetics. Nonpharmacologic treatments include relaxation strategies, eliminating stressors, and a good exercise program. These should first be attempted before pharmacologic therapy. Note that women with migraine headaches have almost a 4-fold risk of developing preeclampsia; therefore, close monitoring for signs and symptoms of preeclampsia is essential. [4, 5, 6]
Is feeling the heart racing a common occurrence during pregnancy?
A significant number of cardiovascular changes occur during pregnancy, which may be accompanied by dyspnea, reduced tolerance for endurance exercise, and basal rales that resolve with deep breathing. During pregnancy, women expand their blood volume by approximately 30-50%. This is accompanied by an increase in cardiac output. The heart rate may also increase by 10-20 beats per minute. The changes peak during weeks 20-24 and usually resolve completely within 6 weeks of childbirth.
The blood pressure in the upper extremities should change very little during pregnancy, but pressure in the lower extremities increases. This is accompanied by pedal edema. Because of extra blood flow, variances in the auscultated heart sounds may occur, such as murmurs, a wider split between the first and second heart sounds, or an S3 gallop. Some nonspecific ST-segment changes may occur, and some changes to the cardiac outline may appear on chest radiographs. The following is a summary of cardiovascular changes:
-
Systolic blood pressure level decreases 4-6 mm Hg.
-
Diastolic blood pressure level decreases 8-15 mm Hg.
-
Mean blood pressure level decreases 6-10 mm Hg.
-
Heart rate increases 12-18 beats per minute.
-
Stroke volume increases 10-30%.
-
Cardiac output increases 33-45%.
What are common respiratory system changes during pregnancy?
Pregnant women experience nasal stuffiness due to estrogen-induced hypersecretion of mucus. Epistaxis is also common as a result of increased blood flow to the nasopharynx. The safest treatment of these symptoms is a saline nasal spray.
In pregnancy, the diaphragm elevates and the thoracic diameter increases, creating a barrel shape to accommodate the gravid uterus.
Pregnancy is a state of relative hyperventilation. An increased tidal volume with an unchanged respiratory rate leads to an increase in minute alveolar ventilation. This places the pregnant woman in a state of respiratory alkalosis. The renal system compensates by increasing excretion of bicarbonate.
The following is a summary of respiratory changes in pregnancy [7] :
-
Respiratory rate does not change.
-
Tidal volume increases 0.1-0.2 L, about 40%.
-
Expiratory reserve volume (ERV) decreases 15%.
-
Residual volume decreases.
-
Vital capacity does not change.
-
Inspiratory capacity increases 5%.
-
Functional reserve capacity decreases 18%.
-
Minute volume increases 40%.
-
Forced expiratory volume (FEV1) does not change.
-
PaO2 levels increase, from 100 to 110 mmHg.
-
PaCO2 levels decrease, from 40 to 27-32 mmHg.
Is gallbladder disease more common during pregnancy?
Gallbladder disease may be more common during pregnancy. Estrogen is an important risk factor for gallstone formation; it increases the concentration of cholesterol in the bile leading to an increased risk of forming gallstones.
Is liver disease more common during pregnancy?
Pregnant women can experience spider angiomata and palmar erythema. About two thirds of white women and only 10% of black women experience these symptoms. In addition, women may have reduced serum albumin concentration, elevated serum alkaline phosphate activity, and elevated cholesterol levels. These are common symptoms of liver disease, but they are not evidence of liver disease if they occur during pregnancy.
Intrahepatic cholestasis of pregnancy occurs when bile flow from the liver is slowed or stopped during pregnancy. The exact mechanism is unclear, but genetic, hormonal, and environmental factors are likely contributory factors. Intrahepatic cholestasis typically occurs in late pregnancy, and it is characterized by intense pruritus and rash over the hands and feet. The maternal prognosis is good, although there may be an increased risk for gallstone disease, hepatic fibrosis, and cholangitis. Fetal consequences are more severe and include meconium ingestion and intrauterine demise. [8]
What hair changes are common during pregnancy?
Hair changes in pregnancy are very common, and body hair changes are common as well. Many women develop mild hirsutism that may be due to levels of male hormone production by the ovary and adrenal gland.
In nonpregnant patients, hair grows in the anagen phase and rests in the telogen phase. About 10%-15% of all hairs are in the telogen phase at any given time. During pregnancy, however, more scalp hairs are in the anagen phase, therefore, more growth is documented. During the telogen resting phase, it is normal for hair to fall out so that new hair can regrow. During late pregnancy, fewer hairs are in the telogen phase; immediately postpartum, more hairs are in the telogen phase. This often results in a dramatic loss of hair immediately postpartum, termed telogen effluvium. Although such an occurrence may be disturbing, it is a normal process.
Normal hair loss is probably in the range of 60-100 hairs a day and most patients do not notice a dramatic loss unless 40% of all hair is lost. This process spontaneously resolves in about 1-5 months, but has been reported to last more than a year. The frontal and parietal areas are usually most affected. No effective treatment is known.
How do sleep patterns change in pregnancy?
Pregnant women have functional changes in their sleep pattern. Although pregnancy-associated sleep disorder is not a specific diagnosis, it has been proposed as a new categorization in the revised International Classification of Sleep Disorders by the American Academy of Sleep Medicine.
Total sleep time increases during the first trimester of pregnancy, normalizes in the second trimester, and decreases in the third trimester with frequent awakening. Changes related to smooth muscle relaxation as a result of circulating progesterone levels include frequent urination, gastric reflux, and nasal congestion—all of which may disrupt sleep. Positional discomfort, leg cramps, breast tenderness, and anxiety can also contribute to poor sleep.
Pregnancy also impacts sleep architecture. In general, the amount of sleep in the rapid eye movement (REM) phase is decreased, and the body spends more time in slow-wave sleep.
Nutrition in Pregnancy
What are the most common dietary complaints during pregnancy?
During early pregnancy, most women experience an increased appetite, with extra caloric needs of approximately 300 kcal/d. Stomach motility decreases, probably due to decreased production of motilin. A decreased incidence of peptic ulcer disease is due to a reduction in gastric acid secretion. Prolonged transit times through the colon are also reported, with transit from the stomach to the cecum occurring in about 58 hours instead of 52 hours.
Some women have nonfood cravings, known as pica. Among US women living in the rural South, the most common nonfood cravings include clay and laundry starch, whereas British women commonly crave coal.
Women who experience nausea or hyperemesis may develop ptyalism (spitting). Reported fluid losses of 1-2 L/d can occur in these women.
See also Prenatal Nutrition.
Should certain foods be avoided during pregnancy?
Pregnant women are at increased risk of bacterial food poisoning. For the safety of both mother and fetus, it is important to take steps to prevent foodborne illnesses, including the following [9] :
-
Properly cook food to kill bacteria. Use a meat thermometer to determine the appropriate temperature, although cooking until well done is safe for most meat. Ground beef should be cooked to at least 160°F, roasts and steaks to 145°F, and whole poultry to 180°F.
-
Cook eggs until they have a firm yolk and are white. Eggnog and hollandaise sauce have raw or partially cooked eggs and are not considered safe.
-
Eat liver in moderation. Liver can contain extremely high levels of vitamin A.
-
Avoid products containing unpasteurized milk, including soft cheeses like brie, feta, and blue cheese. Also avoid unpasteurized juice.
-
Carefully wash all fruits and vegetables to eliminate harmful bacteria. Avoid raw sprouts altogether.
-
Limit caffeine intake. Caffeine crosses the placenta and can affect fetal heart rate. Some clinicians recommend limiting caffeine to less than 200 mg/day (about 2 cups of coffee).
Salmonella species and Escherichia coli (including the dangerous E coli O157:H7) have been associated with raw vegetables, unpasteurized juices, and undercooked meat, poultry, or eggs. There is also the risk of listeriosis from Listeria monocytogenes; it can cause miscarriage, premature delivery, sickness, or death of the newborn. Toxoplasma gondii is a parasite found in a variety of food sources and in dirty cat litter boxes. Infection with this organism can cause hearing loss, intellectual disability, and blindness in the newborn.
In 2007, the FDA warned that Salmonella can be found on the outer skin and shell surfaces of small pet turtles and cautioned those handling turtles without properly washing their hands after handling the animals.
Mad cow disease, Bovine spongiform encephalopathy, has become a growing concern. The disease can be transmitted to humans who eat infected meat, causing Creutzfeldt-Jakob disease. The chances of contracting this disease in the United States is relatively small, but chances can be reduced even further by choosing cuts of meat that are likely to be free of nervous system tissue such as boneless steaks, chops, and roasts. Grass-fed and organic cattle should not have been exposed to any animal products in their feed and are considered to have no known risk. The risk of mad cow disease cannot be lowered by cooking beef more thoroughly because the prions that cause mad cow disease are not destroyed by heat.
Can women safely eat fish while pregnant?
The American College of Obstetricians and Gynecologists (ACOG) issued a warning regarding eating fish in response to the US FDA's consumer advisory about the dangers of eating fish for nursing mothers and women who are or who may become pregnant. The fish themselves are not harmful, but extensive fish consumption increases exposure to the naturally occurring compound methylmercury, levels of which have been increasing in the waters because of industrial pollution. Mercury is very toxic and can cause danger to the fetus and to the newborn nursing infant. Mercury exposure can actually occur via inhalation and/or skin absorption, and all fish contain trace amounts. However, longer-lived and larger fish, such as shark, swordfish, king mackerel, and tilefish, have increased mercury levels and cause the most concern for consumption by pregnant women.
The FDA advises that pregnant or nursing women should not eat shark, swordfish, king mackerel, or tilefish. However, these women can safely eat 12 ounces per week of varieties of fish thought to be low in mercury if they eat a variety of cooked, smaller fish. The safest fish that are low in mercury are shrimp, canned light tuna, salmon, Pollock, and catfish. Specifically, the FDA states that albacore (white) tuna has more mercury than light tuna. So, pregnant women should eat only up to 6 ounces (one average meal) of albacore tuna per week. In addition, the Environmental Protection Agency (EPA) also recommends that pregnant women and young children limit their consumption of freshwater fish caught by family and friends to no more than one meal per week and to follow all local advisories as to fish safety. The EPA specifies no more than 8 ounces of uncooked fish per week for adults.
In June 2014, the FDA released guidelines which encourage the consumption of a variety of low mercury fish in pregnancy. [10] . They recommended 8-12 oz of fish per week which would typically be 2-3 servings. Recommended fish included salmon, pollock, tuna (light canned), tilapia, catfish and cod. Fish to be avoided would be those higher in mercury including tilefish, shard, swordfish and king mackerel.. [10]
Other Questions Related to Pregnancy
What is the recommended weight gain in pregnancy?
After nearly 20 years, the Institute of Medicine released guidelines for weight gain during pregnancy in 2009. The guidelines take into consideration the welfare of the infant and the health of the mother. Important variables to consider regarding weight gain recommendations include the presence of twin or triplet pregnancies, maternal age, and maternal prepregnancy weight. These variables can add to the burden of chronic disease for the mother and baby; excessive weight gain is associated with an increased risk for gestational diabetes, pregnancy-associated hypertension, and delivery of large-for-gestational-age (LGA) infants. [11]
Guidelines for weight gain during pregnancy* are as follows:
-
Underweight women (BMI < 18.5) should gain 28-40 pounds.
-
Normal-weight women (BMI, 18.5-24.9) should gain 25-35 pounds.
-
Overweight women (BMI, 25-29.9) should gain 15-25 pounds.
-
Obese women (BMI, 30 or higher) should gain 11-20 pounds.
*Weight gain guidelines are for singleton pregnancy; weight gain should be higher for multiple pregnancies but the ideal amounts are unknown.
Clinicians are urged to supplement these guidelines with individualized counseling about diet and exercise, and preconception counseling should emphasize the importance of conceiving when the mother is at a normal body mass index (BMI). To help mothers attain these goals, dietary, lifestyle, and exercise interventions have been shown to be safe and effective at reducing excessive weight gain in pregnancy. In an analysis of 44 studies that evaluated the efficacy of these 3 types of interventions, a balanced, low-glycemic diet with a maximum of 30% fat and 15-20% protein and an emphasis on unprocessed whole grains, fruits, beans and vegetables was the most effective. This dietary intervention decreased the incidence of gestational diabetes, gestational hypertension, preterm birth, and intrauterine fetal demise (IUFD). [12]
Dietz et al found that prepregnancy body mass index (BMI) modifies the relationship between pregnancy weight gain and newborn weight for gestational age. In a population-based cohort study of 104,980 singleton, term births from 2000-2005, women who gained 36 lb or more during pregnancy were more likely to bear an infant who was large for gestational age (birthweight >90th percentile) if the mother was lean before pregnancy than if she was overweight or obese. Compared with women who gained 15-25 lb, the adjusted odds ratio (aOR) for a gain of 26-35 lb was 1.5 (95% confidence interval [CI], 1.2-1.9); for a gain of 36-45 lb, the aOR was 2.1 (95% CI, 1.7-2.7); and for a gain of 46 lb or more, the aOR was 3.9 (95% CI, 3.0-5.0). The risk of macrosomia (birthweight 4500 g or more) was not modified by prepregnancy BMI. [13]
Do older fathers have an increased risk of fathering children with birth defects?
No medical information exists to support the hypothesis that increased paternal age causes increased numerical chromosomal abnormalities in the manner that increased maternal age does. However, as males age, structural spermatozoa abnormalities increase, and affected sperm usually cannot fertilize eggs.
The literature suggests a 0.3%-0.5% risk of autosomal dominant disease in offspring of fathers aged 40 years or older. [14, 15] Autosomal dominant disorders include neurofibromatosis, Marfan syndrome, achondroplasia, and polycystic kidney disease.
Paternal age has been identified as a significant predictor of schizophrenia. [16] Studies have also indicated a possible association between advanced paternal age and offspring with autism spectrum disorders. [17] The American Society of Reproductive Medicine recommends an age limit of 50 years for semen donors.
Any family with a history of birth defects should seek individual genetic counseling. To determine whether an individual has a family history of risk, patients should inform their clinician or genetic counselor about any birth defects that have occurred in the past 3 generations.
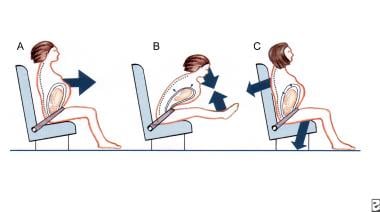
Should women wear seatbelts during pregnancy?
Seatbelts should absolutely be worn during pregnancy. [18] Trauma to the mother is more devastating to the child than any potential entrapment of the pregnant abdomen in the seatbelt. The seatbelt should be placed low, across the hip bones and under the pregnant abdomen. The shoulder strap should be placed to the side of the abdomen, between the breasts, and over the midportion of the clavicle. No information indicates that air bags are unsafe during pregnancy. Pregnant women should try to keep their abdomen 10 inches from the airbag. [19]
See the image below.
Should travel be restricted during pregnancy?
The most recent guidelines primarily focus on the patient’s individual risks and the likelihood of acute problems during the travel segment. [20] The second trimester is considered the safest time to travel, because the risks of miscarriage and preterm labor are the lowest. Prolonged sitting in pregnancy is more restrictive, because the gravid uterus contributes to the risk of thrombosis and it can cause lower extremity venous stasis. Gravid women should promote circulation by ambulating or frequently flexing and extending the lower extremities at the ankles. Air travel can additionally increase the risks of travel in pregnancy because of factors that contribute to dehydration, such as low oxygen tension, low humidity, and recirculated air.
Being pregnant has been estimated to increase the risk of thrombosis about 10 times, to a rate of about 10:100,000; air travel further increases this rate between 2-4 times. Most planes are pressurized to around 8000 feet, so altitude is not an issue.
The International Commission on Radiological Protection recommends a maximum radiation exposure of 1 mSv per year for members of the general public; the same limit is recommended for a conceptus, but over a 40-week pregnancy. Air travel exposes passengers to less than 15% of this limit, even on the longest international flight. Occasional travelers are unlikely to exceed these limits, but frequent flyers should be informed of exposure to radiation and its health risks.
Maternal adaptions to altitude itself vary but could include elevated blood pressure, increased maternal heart rate, and lower oxygen saturation. A fetus can physiologically adapt to these conditions and is typically protected during these flights.
Drinking water and avoiding alcohol and caffeine is important to avoid dehydration. Additional risks may be due to communicable diseases, but those typically depend on to the destination. Traveler's diarrhea is common; pregnant women have an increased risk because of slower gastric and intestinal transit times. Pregnant women should be informed of travel risks and told to wear compression stockings. [21]
Many pregnant women have questions regarding TSA screening devices. TSA conducts a variety of tests to ensure the devices used are safe for all passengers, including pregnant women. TSA’s Advanced Imaging Technology and walk through metal detector systems do not use X-rays to produce the image, but instead use non-ionizing electromagnetic waves that are reflected off the body. According to research conducted by the Food and Drug Administration's Center for Devices and Radiological Health, it is safe for everyone, including pregnant women, to go through these machines. [22]
How can pregnant women best avoid exposure to the Zika virus?
The Zika virus is transmitted by mosquito bites and through intercourse with individuals who have a Zika virus infection. The infection has been linked to severe birth defects including microcephaly. Current CDC recommendations include avoiding travel to countries with known Zika outbreaks and decreasing sexual transmission by avoiding intercourse when the partner has recently traveled to endemic areas. High risk areas include Africa, the Pacific Islands, Latin America, and the Caribbean, but it is a good idea to check the CDC website to see when additional areas are added. It is also important to avoid mosquito bites whenever possible as the mosquito that carries the virus is present in many portions of the USA and it is a matter of time before these mosquitos will become carriers. It is recommended to use an insect repellent that contains DEET, wear a hat, long-sleeved shirt, and long pants where possible, and stay in places that have air-conditioning or screens on windows and doors. Use a bug spray that has been registered with the Environmental Protection Agency. Removing all sources of still water including flowerpots, animal water bowls, and children's pools can also be an important source of protection. [23]
What is the risk of mother-to-infant transmission of coronavirus disease (COVID-19) during pregnancy?
It is uncertain whether there is a risk of vertical mother-to-infant transmission of coronavirus disease (COVID-19). Limited data suggest no evidence of intrauterine infection caused by vertical transmission in women who developed COVID-19 pneumonia in late pregnancy. No data are available on perinatal outcome when the infection is acquired in the first and early second trimesters of pregnancy; these pregnancies should be monitored carefully after recovery. Guidelines on COVID-19 infection control during pregnancy and the puerperium were released by the International Society of Ultrasound in Obstetrics and Gynecology. [24]
Can pregnant women go to the dentist?
Dental care during pregnancy is an important part of overall healthcare. [25, 26] During pregnancy, the gums naturally become more edematous and may bleed after brushing. Epulis gravidarum, a type of gingivitis with violaceous pedunculated lesions, can occur. If treatment of cavities, surgery, or infection care is required, be sure the dentist is aware of the pregnancy. Most antibiotics and local anesthetics are safe to use during pregnancy. Radiographs can be obtained with abdominal shielding but are best avoided during pregnancy because a small, but statistically significant, increase in childhood malignancies exists in children exposed to in-utero radiographic irradiation.
See also Psychosocial and Environmental Pregnancy Risks.
Why is heartburn more common during pregnancy?
Stomach emptying was thought to be retarded during pregnancy, but hormonal influences of increased progesterone and/or decreased levels of motilin may be more responsible for pyrosis (heartburn) than the actual mechanical obstruction in the third trimester. Some studies have also shown decreased lower esophageal sphincter tone, which can lead to an excess of gastric acid in the esophagus.
Why is back pain prevalent during pregnancy and can it be treated?
Half of women report having back pain at some point during pregnancy. The pain can be lumbar or sacroiliac. The pain may also be present only at night. Back pain is thought to be due to multiple factors, which include shifting of the center of gravity caused by the enlarging uterus, increased joint laxity due to an increase in relaxin, stretching of the ligaments (which are pain-sensitive structures), and pregnancy-related circulatory changes.
Treatment is heat and ice, acetaminophen, massage, proper posturing, good support shoes, and a good exercise program for strength and conditioning. Pregnant women may also relieve back pain by placing one foot on a stool when standing for long periods of time and placing a pillow between the legs when lying down.
In a randomized, placebo-controlled trial, Licciardone et al studied the effect of osteopathic manipulative treatment of back pain during pregnancy. No statistically significant differences were achieved between treatment and control groups; however, back pain decreased in the usual obstetric care and osteopathic manipulative treatment group, remained unchanged in the usual obstetric care and sham ultrasound treatment group, and increased in the usual obstetric care only group. [27]
Is sexual intercourse safe during pregnancy?
Research indicates that sexual intercourse is safe in the absence of ruptured membranes, bleeding, or placenta previa, but pregnant women engage in sex less often as their pregnancy progresses. No studies have suggested that any particular position is unsafe, although a 1993 study demonstrated a 2-fold increased incidence of preterm membrane rupture with the male-superior position compared to other positions. [28] ACOG states that sexual activity during pregnancy is safe for most women right up until labor, unless there is a specific contraindication.
ACOG specifically cautions that a woman should limit or avoid sex if she has a history of preterm labor or birth, more than one miscarriage, placenta previa, infection, bleeding, and/or breaking of the amniotic sac or leaking amniotic fluid. ACOG discusses that, as part of natural sexuality, couples may need to try different positions as the woman's stomach grows. Vaginal penetration by the male is not as deep with the male facing the woman's back, and this may be more comfortable for the pregnant woman.
Why do women get varicose veins during pregnancy?
Varicose veins are more common as women age; weight gain, the pressure on major venous return from the legs, and familial predisposition increase the risk of developing varicose veins during pregnancy. These can occur in the vulvar area and be fairly painful. Rest, leg elevation, acetaminophen, topical heat, and support stockings are typically all that is necessary. Determining that the varicosities are not complicated by superficial thrombophlebitis is important. Having a venous thromboembolism in association with superficial thrombophlebitis is rare. Hemorrhoids, essentially varicosities of the anorectal veins, may first appear during pregnancy for the same reasons and are aggravated by constipation during pregnancy.
Why are urinary tract infections more common during pregnancy?
Pregnancy predisposes women with bacteriuria, which in the nonpregnant state is usually self-limiting, to developing urinary tract infections (UTIs). Normal pregnancy-related physiologic changes contribute to UTIs, including dilatation of the upper collecting systems, hypotonic renal pelvises, increases in urinary tract dead space and vesicoureteral reflux, and reductions in the natural antibacterial activity in the urine and in the phagocytic activity of leukocytes at the mucosal surfaces. UTIs in pregnant women usually do not present with typical symptoms, and they may be asymptomatic. All of these factors increase the likelihood for infections to ascend to the kidneys; pyelonephritis is a serious complication of UTIs.
How can stretch marks be prevented?
Unfortunately, striae (stretch marks) cannot be prevented. The degree to which a woman experiences stretch marks is determined genetically. Stretch marks usually occur when weight is lost or gained quickly. Using creams and gels rarely make a difference. Fortunately, striae fade with time and marks become silvery white, but they do not tan. Striae managed early can be reduced with new medical laser technology. [29]
Work and Exercise During Pregnancy
What kind of exercise can women engage in during pregnancy?
Regular physical activity during pregnancy is felt to improve or maintain physical fitness as well as assisting with weight management, decreasing gestational diabetes in obese women and enhancing well-being. A goal for pregnancy exercise would include working up to moderate-intensity exercise for at least 20-30 minutes daily on most days of the week. Although some preexisting conditions such as chronic bronchitis and heavy smoking call for cautionary increases in activity, the majority of women in pregnancy would benefit from becoming or remaining active. Contact sports such as boxing as well as those with a high risk of falling (such as downhill snow skiing) should be avoided. Care should be taken not to overheat and hot yoga and hot Pilates is not recommended. Walking, swimming, stationary cycling, modified yoga and Pilates are well suited to pregnancy. Running, racquet sports and strength training can be safe in pregnancy, especially when these were done regularly prior to pregnancy. Women doing these for the first time should use caution due to the pregnancy causing a change in their center of balance and more laxity in their joints.
In the past, it was felt that pulse rates should not exceed 140 bpm during pregnancy exercise. Newer recommendations use ratings of perceived exertions a more effective means to monitor the intensity of exercise. For moderate intensity one should find the exercise "somewhat hard" on the Borg Rating of Perceived Exertion Scale. Women should remain well hydrated, avoid lying on their backs for long periods and stope if they have vaginal bleeding, painful contractions, amniotic fluid leakage, headache, or chest or calf pain.
Should women restrict work during pregnancy?
Maintaining an active and productive lifestyle helps make time pass faster and adds to a feeling of accomplishment. Working during pregnancy is usually not a problem unless a woman has risk factors or a complicated pregnancy. Women should check with their healthcare providers for specific restrictions. With an uncomplicated pregnancy, working close to or near the due date should not be a problem. Pregnant women should wear comfortable clothing, move around frequently if sedentary, drink plenty of fluids, and have time to rest and take breaks. Women with strenuous jobs, those who work with heavy machinery, or those who work with toxic chemicals should consult their healthcare providers and their job's occupational department for restrictions or concerns.
Labor and Delivery
Which form of psychoprophylaxis is the best and what are their differences?
Appropriate childbirth preparation varies according to each birthing woman. It is recommended that women learn a variety of coping techniques, because one philosophy may not be what is needed during labor. Some of the most popular methods include Lamaze, Bradley, HypnoBirthing, and Birthing from Within.
Lamaze is generally regarded as breathing focused. This method involves focal points, relaxation, and partner coaching. The Lamaze International organization concentrates on education to empower women to make informed choices in their health care. The organization supports birth as a normal, natural experience that is guided by a woman's innate wisdom and ability to give birth.
The Bradley approach largely focuses on "husband-coached childbirth" and teaches coaching and coping techniques aimed at supporting unmedicated childbirth. The Bradley method supports deep abdominal breathing, body awareness, and relaxation techniques.
Hypnobirthing teaches that labor does not have to involve severe pain. Through relaxation techniques and environment modification, Hypnobirthing aims to eliminate fear and tension during labor. The premise of this method is that the fear of pain is what causes the pain itself.
Birthing from Within is both a book and an approach to childbirth education that sees birth as a rite of passage. The lessons, artwork exercises, and reflections are aimed at celebrating the spiritual, psychological, and emotional growth that comes with birth and motherhood. This method provides a variety of coping techniques for labor with the goal of reducing the fear and anxieties surrounding childbirth.
What is the ACOG's position on home births?
While the Committee on Obstetrics Practice believes that hospitals and birthing centers are the safest areas for birthing, it respects the rights of a woman to make medically informed decisions about her place of birth. It feels that women investigating the option of home birth should be told of its risks and benefits using the latest available evidence. They should know that the absolute risk is low but can still have a twofold increased risk of neonatal death. To help increase the safety of these experience for those mothers who choose this option, they should be encouraged to use certified nurse-midwives, certified midwives or a physician practicing within a health system. Timely transport to a nearby hospital would also increase the safety of this birthing option. [30]
What are the benefits of water birth?
The ACOG Committee on Obstetric Practice has addressed the issue of warm-water immersion for women in labor and for delivery of infants. The committee indicated that there are "insufficient data, especially concerning rates of infection, to render an opinion on whether warm-water immersion is a safe and appropriate birthing alternative." The committee also felt that "this procedure should be performed only if the facility can be compliant with OSHA [Occupational Safety and Health Act] standards regarding infection," which would include the specific tub and water recirculation systems used.
Note that warm water exposure over time can cause hypotension, and careful attendance by an assistant is necessary to prevent drowning. The American College of Nurse-Midwives has no current position on either hydrotherapy or water births.
What is the ACOG's position on "role of allied personnel"?
Continuous support during labor from caregivers, including nurses, midwives, or lay individuals, has a number of benefits for women and their newborns, with no apparent harmful effects. The continuous presence of a support person may reduce the likelihood of the use of medication for pain relief, operative delivery, and patient dissatisfaction. [31]
Postpartum
When will the uterus return to normal size?
The uterus returns to prepregnancy size after approximately 6 weeks. This is accomplished through a process called involution. During involution, the uterus has contractions that women may be able to feel, especially during breastfeeding.
When can women resume sexual intercourse after pregnancy?
Women usually can resume sexual intercourse when they feel ready, typically 4-6 weeks after delivery and when bleeding has substantially decreased. Clinically, this is the period when the cervix has closed, which usually occurs at 4 weeks postpartum, and when uterine bleeding is minimal.
The following are other issues to consider:
-
Breastfeeding may cause increased vaginal dryness due to slightly decreased estrogen levels.
-
Women who have had an episiotomy need at least 2-3 weeks to heal before intercourse.
-
An ACOG bulletin indicated that some women may find that they do not have much interest in sex after giving birth because of fatigue, stress, fear of pain, lack of opportunity, and/or lack of desire. This lack of postpartum sexual interest is usually temporary.
Pregnancy Information Sources
A wealth of pregnancy information is available in books, booklets, and on the Internet. The American College of Obstetricians and Gynecologists text Planning Your Pregnancy and Birth and the popular press book What to Expect When You're Expecting are probably the 2 most popular and complete guides for pregnant women.
-
Lumbar lordosis of pregnancy.
-
Uterine fundal size and relative position on abdomen throughout gestation.
-
Correct use of seat belts in pregnancy.