Practice Essentials
The initial evaluation of a person who is injured critically from multiple trauma is a challenging task, and every minute can make the difference between life and death.
Over the past 50 years, assessment of trauma patients has evolved because of an improved understanding of the distribution of mortality and the mechanisms that contribute to morbidity and mortality in trauma.
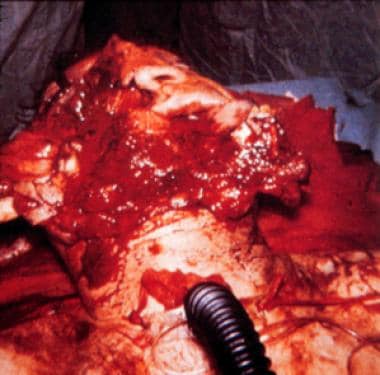
Mortality can be grouped into immediate, early, and late deaths. Immediate deaths are caused by a fatal injury of the great vessels, heart, or neurologic system. [1] Immediate mortality occurs at the scene of injury, as shown in the image below.
 Immediate mortality in trauma occurs at the scene of the injury. Prevention of these deaths requires a multidisciplinary public health systems approach. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
Immediate mortality in trauma occurs at the scene of the injury. Prevention of these deaths requires a multidisciplinary public health systems approach. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
Early deaths may occur minutes to hours after the injury. Injured patients frequently arrive at a hospital before death which usually occurs because of hemorrhage and cardiovascular collapse. Late trauma mortality peaks from days to weeks after injury and is primarily due to sepsis and multiple organ failure. Organized systems of trauma care are focused on the salvage of a patient from early trauma mortality; whereas, critical care is designed to avert later trauma mortality. [2, 3] The location of injury is an important predictor of outcome. A study by Newgard et al evaluated 53,487 EMS transported trauma patients and found that only 29.4% of critically injured rural patients were initially transported to major trauma centers versus 88.7% of urban patients. This study found that 89.6% of rural deaths took place within 24 hours of injury compared to 64% of urban deaths which occurred within 24 hours of injury. [4]
Early deaths result from failed oxygenation of vital organs, massive central nervous system injury, or both. Mechanisms of failed tissue oxygenation include inadequate ventilation, impaired oxygenation, circulatory collapse, and insufficient end organ perfusion. Massive central nervous system trauma leads to inadequate ventilation and/or disruption of brain stem respiratory centers. Injuries that cause early trauma mortality occur in predictable patterns based on mechanism of injury; the patient’s age, gender, and body habitus; or environmental conditions.
Recognition of these patterns led to the development of the Advanced Trauma Life Support (ATLS) approach by the American College of Surgeons. [5] ATLS is the standard of care for trauma patients, and it is built around a consistent approach to patient evaluation. This protocol ensures that the most immediate life-threatening conditions are quickly identified and addressed in the order of their risk potential.
The objectives of the initial evaluation of the trauma patient are as follows: (1) to rapidly identify life-threatening injuries, (2) to initiate adequate supportive therapy, and (3) to efficiently organize either definitive therapy or transfer to a facility that provides definitive therapy.
Triage and Organization of Care
The objective of triage is to prioritize patients with a high likelihood of early clinical deterioration. Triage of trauma patients considers vital signs and prehospital clinical course, mechanism of injury, patient age, and known or suspected comorbid conditions. Findings that lead to an accelerated workup include multiple injuries, extremes of age, evidence of severe neurologic injury, unstable vital signs, and preexisting cardiac or pulmonary disease (see Normal Vital Signs). [6]
When performing a triage with patients who have different types of injuries, the priorities of the primary survey (see Initial Assessment) help to determine precedence (eg, a patient with an obstructed airway receives greater priority for initial attention than a relatively stable patient with a traumatic amputation). In trauma centers, a team of providers evaluates patients who are critically injured and simultaneously performs diagnostic procedures (see the image below). This parallel processing approach can dramatically reduce the time required to assess and stabilize a patient with multiple injuries. [7]
 Trauma resuscitations involving simultaneous diagnosis and treatment by multiple providers demand leadership and organization to function effectively. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
Trauma resuscitations involving simultaneous diagnosis and treatment by multiple providers demand leadership and organization to function effectively. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
The team approach to trauma is resource intensive [8] ; however, the available personnel and resources can become overwhelmed quickly in nonhospital settings, in smaller institutions, and in mass casualty situations. Under these conditions, additional factors affect the triage process, including the number and skill levels of available providers, the available equipment, and the provider's estimate of the clinical probability of each patient's survival. The triage objective becomes how to maximize the number of patients who are salvaged under the prevailing conditions. This process can result in bypassing seriously injured patients until less critical patients have been stabilized. Triage under conditions of limited resources is difficult. [9]
Regardless of the clinical setting, the care team should be organized before patient arrival. Leadership and unity of command are essential for directing a rapid and efficient workup. In larger institutions with dedicated trauma services, general surgeons form the core of the trauma team in close cooperation with the emergency department staff. A physician from either service who is experienced in the care of trauma patients serves as the team leader and directs evaluation and resuscitation.
Additional physicians or midlevel providers are responsible for managing the airway, conducting the primary and secondary surveys, and performing other procedures as needed. Nurses and technicians monitor vital signs, gain intravenous (IV) access, and obtain blood samples. Respiratory therapists and radiology technologists should also be present. As consultants, neurosurgeons and orthopedic surgeons must be available immediately to the trauma team. Early consultation with a neurosurgeon is mandatory when significant central nervous system injury is present. Specific procedures performed by both neurosurgeons and orthopedists can be life-saving.
Care Systems
Multiple studies have demonstrated higher mortality rates and greater proportion of deaths following injury in rural areas compared to urban areas. Even after implementation of a statewide trauma system that reduced mortality in urban areas, improved concentration of seriously injured patients in major trauma centers and an enhanced process of rural trauma care; outcomes between rural and urban areas did not yield comparable improvement. A number of reasons for poorer outcomes in rural areas have been identified and cited including differences in emergency medical services systems, injury severity, access to major trauma care, and delays in care. Ironically, field triage may be as good or better in rural as opposed to urban areas. However, little more than 10% of seriously injured rural patients are initially transported to major trauma centers and only 39% of these patients are ultimately cared for in major trauma centers. Because of the discrepancy between rural and urban trauma systems, rural trauma deaths typically occur early after injury and often take place outside the hospital, which differs from urban areas. Where higher mortality in rural areas have been identified, delays in care, prolonged discovery times, and limited access to major trauma centers have repeatedly been implicated.
Even in states where trauma systems are legislated, performance as a coordinated team of centers is frequently not achieved. When statewide mortality is evaluated, it appears that clustering of trauma centers best serves population centers. Geographic distribution of trauma centers correlates with injury–related mortality as the clustering of state trauma centers are associated with lower fatality rates. While we assume that lower injury fatality rates are due to superior access to trauma care through improved matching of system resources to population centers, specific factors explaining this trend have not been identified. [10]
Recent efforts have examined the implementation of collaborative, inclusive regional trauma systems. In this model, effective coordinated use is made of trauma centers at all levels of sophistication with uniform triage and transfer protocols so that the right patient can get to the right hospital at the right time. Transfer centers and collaboration between multiple hospital systems facilitate efficient and appropriate patient transfers. In addition, collaborative, inclusive regional trauma systems allow aggregation of surgical critical care facilities where the most complex patients may be cared for by a dedicated trauma critical care team. This pattern of organization improves financial and clinical outcomes. Ironically, in some models, having multiple, noncollaborative level I trauma centers in an area may increase confusion as to which center should receive critically injured patients who need the most complex trauma care. Similarly, multiple studies have shown the benefit of high trauma volume on patient mortality. Thus, by increasing the number of trauma centers in an area and decreasing the volume at each trauma center, patient mortality may worsen. [11]
The most intriguing systems work comes from recent military conflicts in Iraq and Afghanistan, where the percentage of wounded service members who died of injuries reached an all-time low of 9.3% compared with 23% during the Vietnam War. A variety of improvements have been identified including advances in hemorrhage control, better resuscitation, and aggressive neurologic critical care. This military experience has led to calls for development of a National Trauma System with the aim of achieving zero preventable deaths after injury and minimizing trauma-related disability. Such a system can learn from accumulated clinical experience and identify avenues to improve performance and outcomes. [12]
Elements needed for a learning trauma system include: 1) leadership and a culture of learning, 2) examination of the entire patient experience from prehospital care to long-term outcomes, 3) coordinated performance improvement and research to generate best practice, 4) rapid dissemination of accumulated knowledge with real-time access to high quality information, 5) transparency and incentives for improved trauma care with provider access to performance data, and 6) systems for ensuring an expert trauma care workforce to train and sustain future generations of trauma care providers.
A cohort study by Hemmila et al that included more than 2.3 million trauma patients reported statistically significant hospital improvements in major complications and venous thromboembolism, as well as improvements in mortality or hospice, after participation in regional collaborative trauma quality improvement programs. [13]
Initial Assessment
The initial evaluation follows a protocol of primary survey, resuscitation, secondary survey, and either definitive treatment or transfer to an appropriate trauma center for definitive care. [5] This approach is the heart of the ATLS system, which is designed to identify life-threatening injuries and to initiate stabilizing treatment in a rapidly efficient manner. Absolute diagnostic certainty is not required to treat critical clinical conditions identified early in the process. When resources are limited (eg, one clinician), do not perform subsequent steps in the primary survey until after addressing life-threatening conditions in the earlier steps.
Primary survey
The steps of the primary survey are encapsulated by the mnemonic ABCDE (airway, breathing, circulation/hemorrhage, disability, and exposure/environment).
The airway is the first priority. Assess it by determining the ability of air to pass unobstructed into the lungs. Critical findings include obstruction of the airway due to direct injury, edema, or foreign bodies and the inability to protect the airway because of a depressed level of consciousness (see the image below). Treatment simply may be secretion control with suctioning or may require endotracheal intubation or placement of a surgical airway (eg, cricothyroidotomy (see the video below), emergent tracheostomy). [14, 15]
 Establishment of a definitive airway may require emergency placement of a surgical airway when facial trauma precludes orotracheal intubation. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
Establishment of a definitive airway may require emergency placement of a surgical airway when facial trauma precludes orotracheal intubation. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
Next, evaluate the breathing to determine patient ability to ventilate and oxygenate. Critical findings include the absence of spontaneous ventilation, absent or asymmetric breath sounds (consistent with either pneumothorax or endotracheal tube malposition), dyspnea, hyperresonance or dullness to chest percussion (suggesting tension pneumothorax or hemothorax), and gross chest wall instability or defects that compromise ventilation (eg, flail chest, sucking chest wound). Treat pneumothorax, hemothorax, tension pneumothorax, and sucking chest wounds with a tube thoracostomy. Initial treatment for a flail chest is mechanical ventilation, which frequently is required for other injuries associated with ventilation and oxygenation deficits.
Evaluate the circulation by identifying hypovolemia, cardiac tamponade, and external sources of hemorrhage. Inspect extremities for quality of perfusion, determine whether the heart tones are auscultated, and determine whether the external hemorrhage is identified and controlled. Initiate treatment of hypovolemia by rapidly infusing a lactated Ringer solution via 2 large-bore, peripheral, IV catheters. Place them preferentially in the upper extremities. Treat cardiac tamponade by pericardiocentesis, or place a subxiphoid pericardial window, followed immediately by surgery to explore and repair the source of bleeding. [16] Control any external bleeding with direct pressure or surgery.
Determine the disability of the patient by performing gross mental status and motor examinations. Determine whether a serious head or spinal cord injury exists. Assess the gross mental status using the Glasgow Coma Scale (see the Glasgow Coma Scale calculator). Examine the pupils for size, symmetry, and reactiveness to light. Obtain an early assessment of spinal cord injury by observing spontaneous movement of the extremities and spontaneous respiratory effort.
Pupillary asymmetry or dilation, impaired or absent light reflexes, and hemiplegia or weakness suggest impending herniation of the cerebrum through the tentorial incisura due to an expanding intracranial mass or diffuse cerebral edema. [17] These findings indicate the need for emergency treatment of intracranial hypertension, including administration of IV mannitol, hypertonic saline, sedatives, and muscle relaxants, after obtaining a definitive airway. Urgent neurosurgical consultation is mandatory.
In the absence of a depressed level of consciousness, paraplegia or quadriplegia indicates spinal cord injury. Possibility of a spinal cord injury requires full spinal immobilization. If inspiratory efforts are weak or when a high cervical cord lesion is suspected, perform an endotracheal intubation. [18, 19]
The final step in the primary survey includes patient exposure and control of the immediate environment. Completely remove patient clothes for a thorough physical examination. Simultaneously, initiate treatment to prevent hypothermia, a condition that is frequently iatrogenic in the exposed patient in an air-conditioned emergency department. Treat prophylactically with the administration of warmed IV fluids, blankets, heat lamps, and warmed air-circulating blankets as needed.
Other procedures
Perform several monitoring and diagnostic adjuncts in concert with the primary survey. [5] Place ECG and ventilatory monitoring leads, and start continuous pulse oximetry as soon as possible. Monitors provide data that are critical to guiding resuscitation. If the patient requires an artificial airway, perform a gastric intubation to decompress the stomach and to lessen the likelihood of aspiration of gastric contents. During the resuscitation phase, insert a urinary catheter to facilitate measuring the response to fluid resuscitation. Placement of a Foley catheter is contraindicated if urethral injury is evident. Signs of urethral injury include blood at the meatus, ecchymosis in the scrotum or labium majora, or a high-riding prostate, which can be identified during a rectal examination. Any of these findings mandate a retrograde urethrogram to exclude urethral injury prior to bladder catheterization.
Resuscitation and Comprehensive Assessment
Resuscitation Phase
During the primary survey, when making diagnoses and performing interventions, continue until the patient condition is stabilized, the diagnostic workup is complete, and resuscitative procedures and surgeries are complete. This ongoing effort involves monitoring patient vital signs, protecting the airway with assisted ventilation and oxygenation as required, and providing resuscitation with IV fluids and blood products.
Patients with multiple injuries may require several liters of crystalloid over the first 24 hours to sustain intravascular volume, tissue and vital organ perfusion, and urine output. Administer blood for hypovolemia, which is unresponsive to crystalloid bolus. [20] If ongoing blood loss is not controlled by direct pressure and transfusion with blood or blood products, surgery or imaging-based procedures may be required to attain hemostasis. The endpoints of resuscitation are normal vital signs, absence of blood loss, adequate urine output (0.5-1 cc/kg/h), and no evidence of end-organ dysfunction. Parameters, such as blood lactate levels and base deficit on an arterial blood gas, may be helpful with patients who are severely injured. [21]
An abundance of standard vital sign data guides evaluation and resuscitation of the injured patient.
The Committee on Trauma for the American College of Surgeons has long published categories of shock that allow the clinician to predict the likelihood of significant blood loss and to anticipate the type and amount of fluid requirements. [5]
The shock classification, as shown in the Table below, allows the clinician to characterize the patient’s response to injury, as blood loss associated with injury progresses, mental status deteriorates, heart rate increases, blood pressure falls, and oliguria is apparent. [5] The patient with persistent vital sign evaluation suggesting hypotension is at significant risk for loss of 30-40% of blood volume on presentation.
Table. Estimated Fluid and Blood Losses Based on Patient’s Initial Presentation [5] (Open Table in a new window)
|
Class I |
Class II |
Class III |
Class IV |
Blood Loss (mL) |
Up to 750 |
750-1500 |
1500-2000 |
>2000 |
Blood Loss (% blood volume) |
Up to 15% |
15-30% |
30-40% |
>40% |
Pulse Rate |
< 100 |
>100 |
>120 |
>140 |
Blood Pressure |
Normal |
Normal |
Decreased |
Decreased |
Pulse Pressure (mm Hg) |
Normal or increased |
Decreased |
Decreased |
Decreased |
Respiratory Rate |
14-20 |
20-30 |
30-40 |
>35 |
Urine Output (mL/h) |
>30 |
20-30 |
5-15 |
Negligible |
CNS/Mental Status |
Slightly anxious |
Mildly anxious |
Anxious, confused |
Confused, lethargic |
Fluid Replacement (3:1 rule) |
Crystalloid |
Crystalloid |
Crystalloid and blood |
Crystalloid and blood |
Secondary Survey
Formally begin this survey after completing the primary survey and after starting the resuscitation phase. At this time, identify all injuries by conducting a thorough head-to-toe examination.
Review the patient's vital signs, and perform a quick repeat of the primary survey to assess patient response to the resuscitation effort and to identify any deterioration.
Then, review the patient's history, including reports from prehospital personnel and from family members or other victims.
If the patient is able or other information sources are available, collect critical data, including preexisting medical problems, current medications and allergies, tetanus immunization status, time of last meal, and events surrounding the injury. These data assist with focusing the secondary survey by identifying the mechanism of injury, the likelihood of cold or heat injury, and the patient's general physiologic status.
Subsequent Physical Examination
The dictum "fingers or tubes in every orifice" guides this examination.
Examine each region of the body for signs of injury, bony instability, and tenderness to palpation.
Evaluate the head and face for maxillofacial fractures, ocular injury, and an open or closed head injury, including a basilar skull fracture.
 Periorbital ecchymosis, or "raccoon eyes," is a classic diagnostic sign of basilar skull fracture. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
Periorbital ecchymosis, or "raccoon eyes," is a classic diagnostic sign of basilar skull fracture. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
Perform a detailed cranial nerve examination as part of a thorough neurologic evaluation.
Inspect the neck anteriorly for evidence of airway or great vessel injury, and palpate posteriorly for bony abnormality or tenderness suggestive of cervical spine injury.
In patients with blunt trauma and patients with an unknown mechanism of injury (eg, "found down"), observe full spine precautions until injury to the spinal column is excluded.
Chest examination
Palpate the chest wall for tenderness, instability, or crepitation, followed by auscultation of the lungs and heart.
In the patient with penetrating trauma, perform a thorough search for additional entry or exit wounds, including examining the axillae and back.
Assess chest tubes for output and air leaks, and use the portable chest x-ray to evaluate for bony abnormalities, persistent pneumothorax, evidence of mediastinal injury, and placement of tubes and lines.
Abdomen and pelvis examination
Inspect the abdomen for distension or other evidence suggesting gross intra-abdominal bleeding or injury.
The presence of a seatbelt sign should prompt a CT scan and a high index of suspicion for bowel injury. [22]
In patients with penetrating trauma, locally explore low-velocity wounds to determine if the muscular fascia is penetrated.
Urgently explore high-velocity penetrating injuries in the operating room.
Palpate the iliac crests once for instability to detect significant pelvic fractures. Use a portable anteroposterior (AP) radiograph to aid in detecting these fractures. If a fracture is diagnosed, avoid additional manipulation of the pelvis to prevent exacerbation of pelvic bleeding, which is notoriously difficult to control. [23]
Inspect for evidence of bleeding (ecchymosis) on the perineum, gross blood on the vaginal and rectal examinations, and urethral injury, followed by placement of a Foley catheter.
In patients with a suspected spinal cord injury, record the anal sphincter motor tone.
Extremity evaluation
In this evaluation, identify long bone fractures that require stabilization, may cause vascular compromise, and show evidence of a major nerve injury.
Perform plain x-ray films to identify deformity, tenderness, or instability.
Conduct temporary splint stabilization prior to moving the patient from the emergency department.
Immediately act on any evidence of vascular compromise, since ischemic injury to an extremity can become irreversible in hours.
Neurologic examination
The elements of the neurologic examination frequently are completed during the regional portions of the secondary survey; however, include a formal assessment of the spine to complete the neurologic assessment.
Log roll the patient with inline stabilization of the head and neck.
Inspect the entire spine from the occiput to the sacrum for bony abnormalities, deformities, and tenderness. At the same time, perform a detailed survey of the back to identify penetrating injuries, ecchymoses, or other injuries. Back injuries frequently are missed.
Imaging and Laboratory Studies
Radiographic imaging studies provide crucial diagnostic data that guide the initial evaluation. The sequence and timing of these studies are important. Stage the imaging studies so that lifesaving interventions identified in the primary survey and resuscitation phases are not impeded. Also, ensure that the patient is hemodynamically stable enough for transfer to the radiology suite.
Anteroposterior radiographs
The AP chest radiograph is the most common imaging study performed on trauma patients. It can be easily obtained during the resuscitation phase, and it provides information on the presence of a hemothorax, pneumothorax, or pulmonary contusion. The AP chest radiograph also aids in the placement of chest and endotracheal tubes, which are critical to the resuscitation effort and the primary survey. [24]
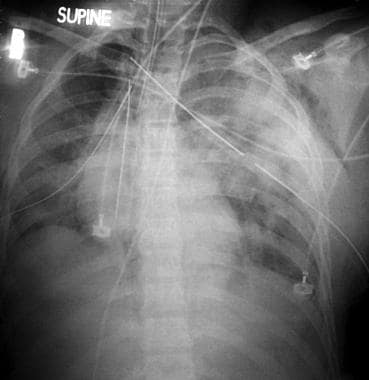 This chest radiograph demonstrates bilateral pulmonary contusions in a trauma patient. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
This chest radiograph demonstrates bilateral pulmonary contusions in a trauma patient. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
For patients with blunt trauma, a portable AP pelvis film can easily be obtained during the resuscitation phase. This film can help confirm the presence of significant pelvic fractures (as depicted in the image below), which are often the sites of hemorrhage that require external fixation and/or angiographic embolization for control.
 The anteroposterior pelvis radiograph quickly helps identify major pelvic fractures and joint disruptions. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
The anteroposterior pelvis radiograph quickly helps identify major pelvic fractures and joint disruptions. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
Focused abdominal sonogram
The extended focused abdominal sonogram for trauma (eFAST) complements the portable chest and pelvis films. [25] A trauma clinician who has been formally trained in the technique quickly and easily performs this portable ultrasound examination in the trauma resuscitation room. It is used to identify free fluid in the peritoneal cavity, pericardial effusion, hemothorax, and pneumothorax. [25] Because of its speed, sensitivity, and noninvasive character, eFAST largely has supplanted other techniques for rapid assessment of unstable trauma patients. This technique requires a major commitment to attain proficiency; therefore, it is not frequently used outside of major trauma centers. [26, 27]
Generally, do not perform diagnostic studies if the capability to act on the information gained is not immediately present. For example, patients with blunt trauma initially transported to small rural emergency departments frequently have indications for advanced imaging. If an appropriately trained surgeon is not present in the institution, then these studies are of questionable value, since they may delay the transfer of the patient to a trauma center. Consequently, stage imaging studies and prioritize them based on patient stability, the practical utility of the data to be obtained, and the imperative need for early transfer to obtain definitive care.
CT scan
The CT scan is the definitive radiographic study in most patients with trauma. CT imaging of the abdomen, pelvis, chest, cervical spine, and head is the most sensitive and accurate noninvasive diagnostic tool for identifying major injury. Bedside assessment of blunt traumatic injury was recently evaluated to assess the impact of CT scans. [28] Bedside evaluation was effective in ruling out serious injuries in patients with low risk of serious injury. Overall diagnostic accuracy of bedside assessment was low, however, suggesting that CT be utilized in high-acuity patients to avoid missing injuries. [28, 29]
Over reliance on CT imaging can be detrimental if emergent operations are delayed. One review of patients presenting with hypotension (systolic BP < 90 mm Hg) and significant abdominal injury demonstrated greater mortality if surgery was delayed by a CT scan. [30] Excessive radiation exposure is also a concern. [31]
 CT scan of the abdomen identifies significant soft tissue injury with high sensitivity and specificity. A traumatic liver laceration due to blunt trauma with rib fragment penetration into the liver parenchyma is shown. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
CT scan of the abdomen identifies significant soft tissue injury with high sensitivity and specificity. A traumatic liver laceration due to blunt trauma with rib fragment penetration into the liver parenchyma is shown. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
Obtain a CT scan of the head to identify intracranial bleeding (as seen in the image below) and to guide neurosurgical intervention. [32] Obtain a head CT scan for trauma without IV contrast, and perform it first when indicated, prior to the injection of an IV contrast for abdominal and pelvic scans. Most centers scan the cervical spine at the same setting in patients receiving CT evaluation of the head.
 The head CT scan for trauma identifies space-occupying lesions and directs operative evacuation. The lenticular shape of this lesion identifies it as an epidural hematoma. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
The head CT scan for trauma identifies space-occupying lesions and directs operative evacuation. The lenticular shape of this lesion identifies it as an epidural hematoma. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
Obtain a CT scan of the chest to evaluate mediastinal injuries. [33] CT scanning is replacing aortography as the state-of-the-art study for imaging mediastinal vascular structures, particularly the aorta. [34] CT scanning is also more sensitive than AP chest radiography in the detection of pneumothorax, rib fractures, pulmonary contusion, and hydrothorax. For most patients with trauma, CT scans of the head, chest, abdomen, and pelvis are sufficient to guide operative and nonoperative management of injuries in their respective regions of the body. [35]
CT scans of the abdomen and pelvis usually are performed together, using IV and sometimes oral contrast. [36] Use this study to identify injuries to abdominal and pelvic organs and to identify bleeding in the retroperitoneum and pelvis.
As the quality of CT scans continues to increase, the role of angiography continues to focus to a greater degree on interventions rather than on diagnosis. [37] CT technology can readily evaluate vascular injury using a single dose of intravenous contrast.
A growing volume of data supports the aggressive use of CT scanning in the evaluation of blunt trauma. [38, 39] For example, abdominal injury becomes more likely with velocity changes of greater than 20 km/h. Extremes of age or extremity, head, or spine injuries are predictive of abdominal trauma as well. The absence of coincident injury decreases the risk of abdominal injury. [40] One review of aortic injuries reveals an increased risk with lateral impacts and lack of seatbelt use. Associated injuries were poor predictors. [41]
Several reports from major trauma centers emphasize the value of CT scanning to evaluate penetrating torso injuries. Patients requiring hospitalization or extended periods of observation in the emergency department may now be sent home with a late generation CT scan that demonstrates the benign track of a bullet wound or stabbing injury. [42, 43, 44, 45] With increasing resolution, even small bowel and mesenteric injuries are now readily identified. [46] These injuries were previously difficult to detect and can be a source of late morbidity for patients. [47]
A practice of early comprehensive multislice CT is rapidly evolving in urban trauma centers. This use of advanced CT technology leads to a more accurate and faster diagnosis with a reduction in resource utilization. Whether increasing radiation exposure with the use of advanced CT technology will become a clinical and social issue is unclear.
Spine evaluation
CT scanning is replacing plain radiographs in many patients being evaluated for spine trauma. [48, 49] Current scanners offer the capability to reconstruct spine images at the same time that scans are obtained of the chest, abdomen, and pelvis. [50] Many clinicians will scan the cervical spine in patients with other indications for scans of the head or the head and torso. Orthopedic and neurosurgical consultants are making increased use of CT in evaluation of the spine.
Obtain plain x-ray films of the spine in patients with high-energy blunt trauma and in other trauma patients with known or suspected neurologic deficits if CT scanning is unavailable or if a complimentary image is desired. [51]
For patients with a low likelihood of spinal injury, defer most or all of the spinal radiograph series until the resuscitation phase is well underway and, if necessary, after performing a lifesaving emergent laparotomy, craniotomy, or other operations.
If a greater-than-routine need to exclude cervical spine injury exists, perform a portable lateral cervical spine (C-spine) film during the resuscitation phase. An adequate lateral C-spine x-ray (eg, visualizing from the skull base to T1) helps identify most C-spine fractures and subluxations. Ultimately, a full C-spine series (ie, AP, lateral, and odontoid views) must be performed to exclude injury, and virtually all trauma clinicians will request CT if any doubt exists.
The Advanced Trauma Life Support curriculum points out that, with identification of a cervical spine fracture, the likelihood of another break in the spinal column is 10%. Many centers now accept complete CT imaging as sufficient evaluation to rule out injury of the cervical spine and other spine levels. Some centers continue to perform MRI where a question of occult ligamentous injury exists. Large datasets have reported that in more than 20% of patients, injuries were identified on MRI that were not seen on high resolution CT. However, few of the additional injuries identified with MRI were clinically significant and a small number led to additional surgical procedures. [52, 53]
For patients with a neurologic deficit but negative plain films and CT scans (formerly called spinal cord injury without radiographic abnormality), conduct an MRI of the spinal column and nerve roots. An MRI is the most sensitive method for detecting this type of soft tissue injury, although CT scanning has become the standard for acute evaluation of the vast majority of spinal column injuries. [19, 27, 54]
Angiography
Angiography can be both a diagnostic procedure and a therapeutic procedure, and it is valuable in selected trauma patients. The most common indication for emergent angiography in trauma is to identify and control arterial bleeding from pelvic fractures or in the retroperitoneum. Contemplate emergent thoracic aortic angiography when plain x-ray films or a CT scan of the chest reveals evidence of atypical mediastinal bleeding. CT is now the diagnostic modality and stent grafting the treatment for blunt aortic injury. [55, 56, 57] In aortic injury, angiography is the historical standard for diagnosis and operative planning. [57] With suspected bleeding in the retroperitoneum and pelvis, an angiographic embolization often is quicker and safer than surgical approaches in these difficult difficult-to-access areas; however, this is only true with arterial bleeding, while the more common case of venous bleeding remains a difficult management problem. [55]
Angiography also facilitates nonoperative management of injury to the liver, spleen, and kidney following blunt trauma. Specific criteria for angiography and embolization have not been agreed upon. [58] A CT scan of the abdomen with intravenous contrast frequently demonstrates areas of active bleeding, which may be targeted by the interventional radiologist in the patient who is sufficiently stable to tolerate the time delay required to obtain angiography and organ-specific embolization of bleeding points.
Laboratory studies during the initial evaluation
The most important laboratory study is the type and crossmatch, which often can be completed within 20 minutes of receipt of the blood sample.
Arterial blood gases are also useful in the initial assessment period, although their use for serial monitoring has declined since the introduction of continuous pulse oximetry.
A baseline hemoglobin or hematocrit determination is useful on arrival, with the understanding that in acute hemorrhage, a fall in hematocrit may not be apparent until autogenous mobilization of extravascular fluid or administration of IV resuscitation fluids commences.
Urine screens for drugs of abuse commonly are ordered in trauma centers. For similar reasons, check blood alcohol and glucose levels to identify correctable causes of a decreased level of consciousness. A review from the data of the National Trauma Data Bank of the United States reveals a disturbing decline in substance use screening, despite the importance of substance use as a contribution to injury. [59] Early hyperglycemia has been linked to an increased risk of infectious complications and mortality after injury. [60]
For most trauma patients, serum electrolytes, coagulation parameters, cell blood counts, and other common laboratory studies are less useful during the first 1-2 hours than they are after stabilization and resuscitation.
Special Injuries
The foregoing discussion is applicable to most trauma patients with either blunt trauma or penetrating trauma; however, patients with burns, cold injuries, and electrical injuries have special considerations that must be addressed during the initial assessment and resuscitation.
Burns
An early imperative is to stop the burning process, especially in the case of chemical burns, in which the continued contact of the agent with the patient's skin may not be readily apparent. This process may require repeated testing of the patient's skin, specific chemical neutralization, and extensive lavage of the affected areas. If full thickness burns of an extremity or the thorax are suspected, escharotomies may be required to prevent compartment syndrome and impaired ventilation, respectively. [61]
If the clinical history or the physical examination suggests that upper airway burns or inhalation injury may be present, then early intubation and mechanical ventilation are indicated.
Finally, patients with large burns require large volumes of IV crystalloid resuscitation fluids. While this resuscitation can be delayed briefly while performing lifesaving interventions, early commencement is beneficial.
Cold injuries
The dominant imperative is rewarming, particularly in the case of systemic hypothermia, but it is equally applicable to cold injuries to the extremities (eg, frostbite). [62] While mild hypothermia is managed as described above for the primary survey (see Primary survey in Initial Assessment), treat severe cold injuries with immersion in water warmed to 40°C or with cooling devices wihch allow simultaneous performance of other needed procedures. Administer IV fluids as indicated, based on the patient's physiologic status (not on the wound size). In the case of severe hypothermia with cardiac arrest and/or apnea, do not stop resuscitation efforts until the patient is rewarmed thoroughly. [63]
High-voltage electrical injuries
Although sometimes considered as burn injuries, high-voltage electrical injuries (eg, lightning strikes, power lines) present a different set of problems. [61] First, much of the tissue injury from electrical injuries may not be apparent on physical examination. Massive myonecrosis and damage to both soft tissue and bone may be concealed beneath normal-appearing skin between the entrance and exit wounds; therefore, maintain a low threshold for measurement of compartment pressures and performance of decompressive fasciotomies. Carefully and continuously monitor the urine output for evidence of myoglobinuria, which can lead to acute renal failure if untreated. Likewise, provide continual cardiac monitoring to the patient because of the risks of direct myocardial injury and hyperkalemia arising from myonecrosis.
Perils, Pitfalls, and Controversies
A sudden, expected deterioration of an initially stable patient is a common problem encountered during the care of multiple trauma patients. This situation is especially problematic after performing thorough primary and secondary surveys and instituting a resuscitation plan. The solution to these crises lies in the ABCs (airway, breathing, and circulation) of the primary survey. [64]
Injuries can evolve from subclinical to clinically apparent over the course of a rapid trauma workup, and even the best diagnostic workup is not perfect; therefore, it is necessary to ensure that the airway is clear, that ventilation is adequate, and that the blood pressure and end-organ perfusion are sufficient. By rapidly rechecking the elements of the primary survey first, easily corrected problems (eg, malpositioned endotracheal tubes, tension pneumothorax, unsuspected hemorrhage) can be rapidly identified and addressed.
Nevertheless, the initial surveys may miss injuries, especially in seriously injured patients who require intensive resuscitative and/or surgical procedures to stabilize. This tendency is exacerbated by the focused priorities of the primary survey and resuscitation phase. A simple remedy for this problem is frequent and thorough reassessment. Perform a formal tertiary survey within 18-36 hours after admission. It consists of a thorough head-to-toe examination in conjunction with a review of all laboratory data and imaging studies obtained since admission. While the tertiary survey does not reduce the incidence of injuries missed during the primary and secondary surveys, it decreases their morbidity and mortality by earlier identification and treatment.
A difficult aspect of treating multiple trauma patients is prioritizing between competing injuries in the same patient. The three examples that follow illustrate clinical dilemmas in decision-making faced by surgeons caring for trauma victims.
Patient 1
A relatively straightforward example is an individual with a posterior dislocation of the knee joint and concomitant vascular compromise below the knee. In this case, the competing interests are the orthopedic repair of the knee joint versus the repair of damaged vessels, presumably including the popliteal artery. Although a disrupted knee joint is clearly an urgent problem, especially if the joint space is open, the short viability of a devascularized limb (3-4 h) and the increasing risk of compartment syndrome with increasing time of ischemia are the paramount issues. Therefore, vascular repair usually is performed first, followed by the orthopedic repair.
Patient 2
A more difficult dilemma occurs in the unstable hypotensive patient with abdominal and head injuries. The need for operative exploration and control of abdominal hemorrhage must be balanced against the need for a head CT scan to identify and localize potentially fatal intracranial mass lesions for neurosurgical drainage. A rule of thumb in situations such as these is that blunt head trauma alone usually does not cause hypotension, and hypovolemia is the probable culprit. Preserving the blood pressure and cerebral perfusion is essential to prevent secondary brain injury; thus, measures to control hypotension and intra-abdominal bleeding often are prioritized earlier than head injuries, which are prognostically more serious.
Patient 3
A final example lies in the timing of operative versus angiographic treatment of blunt pelvic trauma with known or suspected hemorrhage from pelvic fractures. The safety and efficacy of angiographic embolization must be balanced against the knowledge that most causes of pelvic hemorrhage are venous in origin and, therefore, are not amenable to angiographic embolization. Furthermore, the resuscitation of the unstable patient is much more difficult in the angiography suite than in the ICU. No simple rules apply, and only the good judgment of the senior clinician responsible for the patient can identify the best approach in each case.
-
Immediate mortality in trauma occurs at the scene of the injury. Prevention of these deaths requires a multidisciplinary public health systems approach. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
-
Trauma resuscitations involving simultaneous diagnosis and treatment by multiple providers demand leadership and organization to function effectively. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
-
Establishment of a definitive airway may require emergency placement of a surgical airway when facial trauma precludes orotracheal intubation. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
-
Periorbital ecchymosis, or "raccoon eyes," is a classic diagnostic sign of basilar skull fracture. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
-
This chest radiograph demonstrates bilateral pulmonary contusions in a trauma patient. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
-
The anteroposterior pelvis radiograph quickly helps identify major pelvic fractures and joint disruptions. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
-
CT scan of the abdomen identifies significant soft tissue injury with high sensitivity and specificity. A traumatic liver laceration due to blunt trauma with rib fragment penetration into the liver parenchyma is shown. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
-
The head CT scan for trauma identifies space-occupying lesions and directs operative evacuation. The lenticular shape of this lesion identifies it as an epidural hematoma. Courtesy of Kevin Kilgore, MD; Carson Harris, MD; and David Hale, MD, Regions Hospital, St Paul, Minn.
-
Surgical cricothyroidotomy Seldinger. Video courtesy of Therese Canares, MD, and Jonathan Valente, MD, Rhode Island Hospital, Brown University.










