Practice Essentials
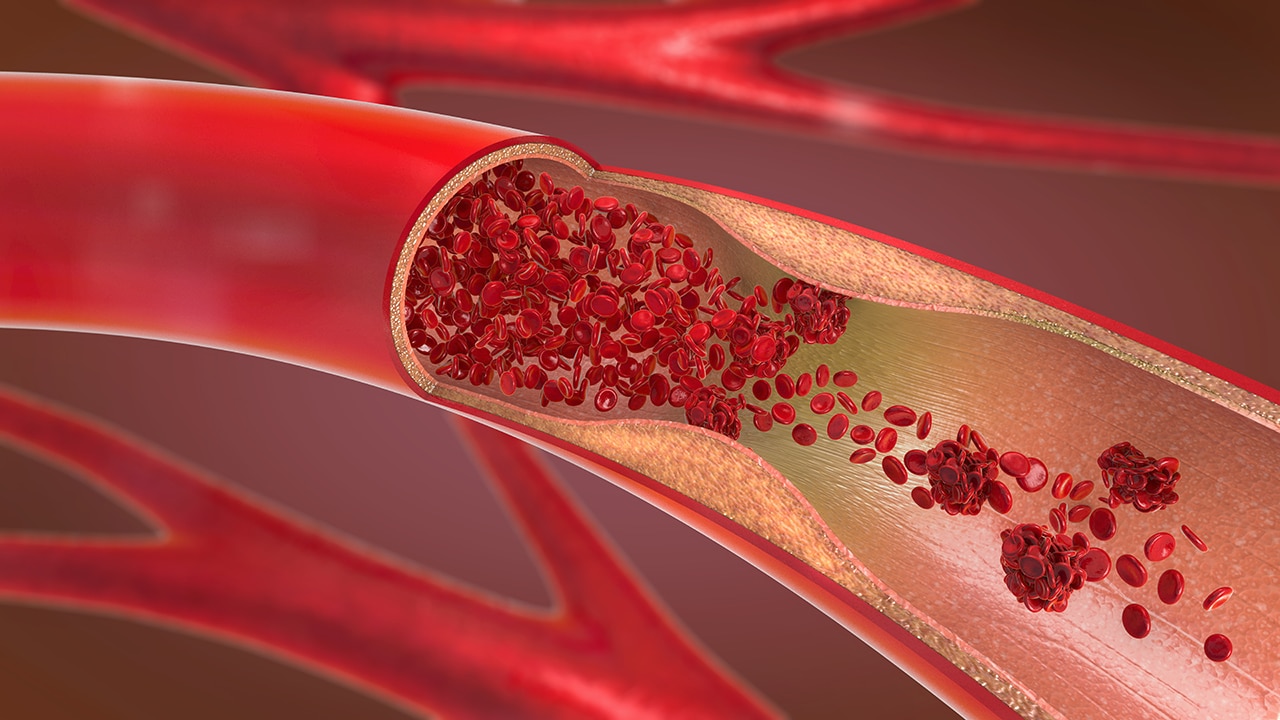
Superficial thrombophlebitis is a common inflammatory-thrombotic disorder in which a thrombus develops in a vein located near the surface of the skin. Most superficial veins that develop thrombosis also have phlebitis, in contrast to deep venous thrombosis (DVT), a sometimes asymptomatic condition in which phlebitis may be absent. (See Etiology and Workup.)
Although superficial thrombophlebitis usually occurs in the lower extremities, it also has been described in the penis and the breast (Mondor disease). Superficial thrombophlebitis can also develop anywhere that medical interventions occur, such as in the arm or neck (external jugular vein) when intravenous (IV) catheters are used. (See Etiology, Presentation, and Workup.)
Thrombosis and thrombophlebitis of the superficial venous system receive little attention in medical and surgical textbooks. However, thrombophlebitis is encountered frequently, and although it is usually a benign, self-limiting disease, it can be recurrent and tenaciously persistent, at times causing significant incapacitation. (See Epidemiology and Prognosis.)
When affecting the great saphenous vein (GSV; also referred to as the greater or long saphenous vein), thrombophlebitis will sometimes progress into the deep venous system. Damage to deep venous valves leads to chronic deep venous insufficiency (often referred to as postphlebitic syndrome), as well as to recurrent pulmonary embolism (PE) and an increased risk of death. [1]
Causes and sites of development
Superficial thrombophlebitis can occur spontaneously, especially in the lower extremities in the GSV, or as a complication of medical or surgical interventions. Although the etiology is frequently obscure, superficial venous thrombosis is most often associated with one of the components of the Virchow triad; ie, intimal damage (which can result from trauma, infection, or inflammation), stasis or turbulent flow, or changes in blood constituents (presumably causing increased coagulability). (See Etiology.)
In each type of superficial thrombophlebitis, the condition presents as redness and tenderness along the course of the vein, usually accompanied by swelling. Bleeding also can occur at the site of a varicose vein. (See Presentation.)
Although unusual, superficial thrombophlebitis may occur in the small saphenous vein (SSV; also referred to as the lesser saphenous vein), which empties into the popliteal vein.
Superficial thrombophlebitis can also occur in the external jugular vein, if it has been used for an infusion site. Superficial thrombophlebitis of the upper extremities usually occurs at infusion sites or sites of trauma.
Diagnosis and treatment
Superficial thrombophlebitis is a clinical diagnosis in which the clinician identifies tender and inflamed superficial veins. However, ruling out DVT in the clinical setting is difficult; further testing is often required to evaluate for this condition. (See Presentation and Workup.)
Treatment for superficial thrombophlebitis is aimed at patient comfort and at preventing superficial phlebitis from involving the deep veins. [2, 3] (See Treatment and Medication.)
Superficial phlebitis with infection, such as phlebitis originating at an IV catheter site, is referred to as septic thrombophlebitis, a clinical entity requiring diagnostic and therapeutic approaches that are different from those applied to sterile phlebitis.
Pathophysiology
Microscopic thrombosis is a normal part of the dynamic balance of hemostasis. In 1846, the German pathologist Virchow recognized that if this dynamic balance were altered by venous stasis or turbulence, abnormal coagulability, or vessel wall injuries, then microthrombi could propagate to form macroscopic thrombi.
In the absence of a triggering event, neither venous stasis nor abnormal coagulability alone causes clinically important thrombosis, but vascular endothelial injury does reliably result in thrombus formation. The initiating injury triggers an inflammatory response that results in immediate platelet adhesion at the injury site. Further platelet aggregation is mediated by thromboxane A2 (TxA2) and by thrombin. A more detailed visual of the coagulation pathway can be seen in the image below.
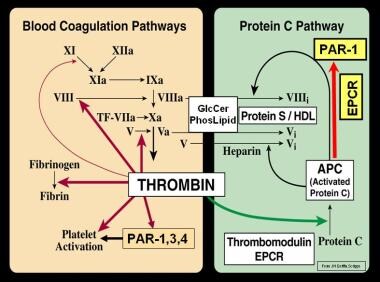 Blood coagulation (thrombin) and protein C pathways. Courtesy of Wikimedia Commons ©John H Griffin, PhD.
Blood coagulation (thrombin) and protein C pathways. Courtesy of Wikimedia Commons ©John H Griffin, PhD.
Platelet aggregation due to TxA2 is inhibited irreversibly by aspirin and reversibly by other nonsteroidal anti-inflammatory drugs (NSAIDs); thrombin-mediated platelet aggregation, on the other hand, is not affected by NSAIDs, including aspirin. This is why aspirin and other NSAIDs are somewhat effective in preventing arterial thrombosis, where platelet aggregation is mediated via TxA2, as seen in patients with stroke and myocardial infarction (MI), but are not very effective in preventing venous thrombophlebitis, where it is believed that clot formation is more of a result of thrombin activation.
Etiology
Risk factors
The most important clinically identifiable risk factors for thrombophlebitis are a prior history of superficial phlebitis, DVT, and PE. Some common risk markers include recent surgery or pregnancy, prolonged immobilization, and underlying malignancy.
Phlebitis also occurs in diseases associated with vasculitis, such as polyarteritis nodosa (periarteritis nodosa) and Buerger disease (thromboangiitis obliterans). Buerger noted phlebitis in eight of 19 patients, and Shionoya reported it in 43% of the 255 patients he followed. [4, 5] After 2010, a medically emergent cutaneous thombophlebitis began to be noted more frequently, after an increase in use of levamisole (an antihelminth) for bulking cocaine in the United States. In a review of the literature by Pearson et al, cutaneous thrombosis was noted in 84% of patients presenting with levamisole-induced vasculopathy. [6, 7]
Pregnancy
The increased likelihood of developing thrombophlebitis occurs through most of pregnancy and for approximately 6 weeks after delivery. This is partly due to increased platelet stickiness and partly due to reduced fibrinolytic activity.
The association between pregnancy and thrombophlebitis is of particular concern to women who carry the factor V Leiden or prothrombin C-20210-a gene, because they already have a predisposition to clotting, which would also be exacerbated by pregnancy. [8]
Estrogen therapy
High-dose estrogen therapy is another risk factor. Case-controlled and cohort studies based on clinical signs and symptoms of thrombosis suggest that by taking high-estrogen oral contraceptives, a woman may increase her risk of thrombosis by a factor of 3-12 times, though the absolute risk remains low. Newer low-dose oral contraceptives are associated with a much lower risk of thrombophlebitis, though the absolute risk has not been well quantified. [9]
Additional risk factors
Other recognized markers of risk for venous thromboembolic disease include the following:
-
Varicose veins
-
Obesity
-
Age older than 60 years (however, there are fewer complications in this age group)
-
Cigarette smoking
-
IV drug abuse
-
Hypercoagulable states (eg, factor V Leiden mutation, prothrombin gene mutation, and protein S deficiency)
-
Systemic lupus erythematosus
-
Acquired immunodeficiency syndrome (AIDS) - Lupus anticoagulant
-
Drug-induced lupus anticoagulant
-
Antithrombin III deficiency
-
Behçet disease
-
Blood type A
-
Burns
-
Catheters (indwelling venous infusion catheters)
-
Chemotherapy
-
Congestive heart failure
-
Estrogen replacements (high dose only)
-
Fibrinogen abnormality
-
Fractures
-
Hemolytic anemias
-
Heparin-associated thrombocytopenia
-
Homocysteinemia
-
Homocystinuria
-
Hyperlipidemias
-
Immobilization
-
Malignancy
-
MI
-
Phenothiazines
-
Plasminogen abnormality
-
Plasminogen activator abnormality
-
Polycythemia
-
Postoperative
-
Protein C deficiency
-
Protein S deficiency
-
Resistance to activated protein C
-
Thrombocytosis
-
Trauma
-
Ulcerative colitis
-
Venography
-
Venous pacemakers
-
Venous stasis
-
Warfarin - First few days of therapy
-
Caustic materials, such as lighter fluid, injected intravenously [10]
Traumatic thrombophlebitis
Superficial venous thrombosis following an injury usually occurs in an extremity, manifesting as a tender cord along the course of a vein juxtaposing the area of trauma. Ecchymosis may be present early in the disease, indicating extravasation of blood associated with injury to the vein; this may turn to brownish pigmentation over the vein as the inflammation resolves.
Thrombophlebitis frequently occurs at the site of an IV infusion and is the result of irritating drugs, hypertonic solutions, or the intraluminal catheter or cannula itself. This is by far the most common type of thrombophlebitis encountered. Usually, redness and pain signal its presence while the infusion is being given, but thrombosis may manifest as a small lump days or weeks after the infusion apparatus has been removed. It may take months to completely resolve.
The features of iatrogenic form of traumatic (chemical) phlebitis may be deliberately produced by sclerotherapy during the treatment of varicose veins.
Thrombophlebitis in varicose vein
Superficial thrombophlebitis frequently occurs in varicose veins. It may extend up and down the saphenous vein or may remain confined to a cluster of tributary varicosities away from the main saphenous vein.
Although thrombophlebitis may follow trauma to a varix, it often occurs in varicose veins without an antecedent cause.
Thrombophlebitis in a varicose vein develops as a tender, hard knot and is frequently surrounded by erythema. At times, bleeding may occur as the reaction extends through the vein wall. It frequently is observed in varicose veins surrounding venous stasis ulcers.
Superficial thrombophlebitis along the course of the GSV is observed more often to progress to the deep system.
Infection-related thrombophlebitis
Infection-related thrombophlebitis is associated with several different conditions, including a serious complication of intravascular cannulation and can be suspected in patients who have persistent bacteremia in the setting of appropriate antibiotic therapy. [11] It is characterized by perivascular inflammation with or without evidence of purulence within the venous lumen. It also frequently is associated with bloodstream infection.
In 1932, DeTakats suggested that dormant infection in varicose veins was a factor in the development of thrombophlebitis occurring following operations or after injection treatments, trauma, or exposure to radiation therapy. [12]
Altemeier et al suggested that the presence of L-forms and other atypical bacterial forms in the blood may play an important etiologic role in the disease and recommended administration of tetracycline. [13]
Migratory thrombophlebitis
Jadioux described migratory thrombophlebitis in 1845, determining it to be an entity characterized by repeated thromboses developing in superficial veins at varying sites but occurring most commonly in the lower extremity. Although numerous etiologic factors have been proposed for this condition, none have been confirmed.
The association of carcinoma with migratory thrombophlebitis was first reported by Trousseau, in 1856. Sproul noted migratory thrombophlebitis to be especially prevalent with carcinoma of the tail of the pancreas. [14]
Thrombophlebitis of superficial veins of breast and anterior chest wall (Mondor disease)
Mondor disease is a rare condition. Thrombophlebitis is usually located in the anterolateral aspect of the upper portion of the breast or in the region extending from the lower portion of the breast across the submammary fold toward the costal margin and the epigastrium.
A characteristic finding is a tender, cordlike structure that may be best demonstrated by tensing the skin via elevation of the arm.
The cause of Mondor disease is unknown, but a search for malignancy is indicated. Mondor disease is more likely to occur after breast surgery, with the use of oral contraceptives, and with protein C deficiency.
Thrombophlebitis of the dorsal vein of the penis, generally caused by trauma or repetitive injury, is also referred to as Mondor disease. [15, 16]
Epidemiology
Superficial thrombophlebitis is a common condition worldwide.
In the author's experience, superficial thrombophlebitis most frequently occurs in the age group ranging from young adulthood to middle age. However, Markovic et al reported that a common risk factor is age older than 60 years, though fewer complications occur in this age group. [17]
As previously mentioned, pregnancy, puerperium, and high-dose estrogen therapy are recognized risk factors for phlebitis. However, there are no intrinsic, sex-linked risks for the disease.
Prognosis
The prognosis in superficial thrombophlebitis is usually good. Superficial phlebitis is rarely associated with PE, though it can occur, particularly if the process extends into a deep vein. However, individuals with superficial venous thrombosis do not seem to have a great tendency to develop DVT. In contrast, patients with DVT are frequently found to have superficial venous thrombosis.
The patient should be told to expect the disease process to persist for 3-4 weeks or longer. If it occurs in the lower extremity in association with varicose veins, it has a high likelihood of recurrence unless excision is performed.
Patient Education
Because thrombophlebitis tends to recur if the vein has not been excised, instructing the patient in ways to prevent stasis in the vein is usually advisable. The use of elastic stockings may be indicated, especially if the patient plans to stand in an upright position for long periods. Slight elevation of the foot of the bed, avoidance of long periods of standing in an upright position, and avoidance of prolonged inactivity is recommended.
For patient education information, see Varicose Veins, Deep Vein Thrombosis (Blood Clot in the Leg, DVT), and Phlebitis.
-
Deep venous thrombosis.
-
Thrombosis of great saphenous vein and tributaries. Note lack of full compressibility of vein secondary to intraluminal thrombus. Courtesy of Wikimedia Commons ©Nevit Dilmen.
-
Blood coagulation (thrombin) and protein C pathways. Courtesy of Wikimedia Commons ©John H Griffin, PhD.