Practice Essentials
The cardiovascular systems of patients who undergo general anesthesia and noncardiac surgical procedures are subject to multiple stresses and complications. Cardiac risk assessment allows clinicians to group these patients into the following categories [1] :
-
Low-risk patients, who require no further testing.
-
Intermediate- and high-risk patients, who should undergo preoperative investigations and treatment to reduce overall perioperative morbidity and mortality.
Workup
The preoperative cardiac risk evaluation involves obtaining a thorough history and physical examination, along with a baseline electrocardiogram (ECG). Clinicians should inquire about established cardiac diseases, including ischemic heart disease, hypertension, arrhythmia, valvular heart disease, congestive heart failure (CHF), and the presence of a pacemaker or implantable defibrillator.
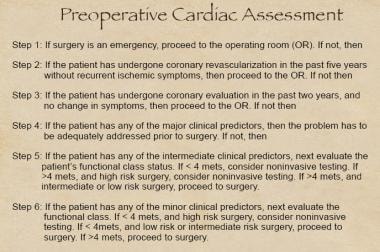
A stepwise approach to cardiac risk stratification includes the assessment of clinical markers, prior cardiac evaluation and management, functional capacity in metabolic equivalents (mets), and surgery-specific risk. Generally, the more extensive the surgical procedure, the greater the physiologic stress, the more significant the postoperative pain, and the greater the incidence of cardiac complications.
The following tests are recommended for cardiac risk stratification:
-
Dobutamine stress echocardiography, which should be avoided in patients with a history of ventricular tachyarrhythmia.
-
Dipyridamole thallium imaging, which should be used with caution in those with underlying reactive airway disease.
-
Coronary angiography, which is generally reserved for patients with evidence of coronary artery disease (CAD).
Transthoracic echocardiography (TTE), exercise treadmill testing, and ambulatory ECG monitoring are not recommended for risk stratification.
Management
Preoperative and intraoperative cardiac management
Beta-blockers should be started 1 week before elective surgery, with the dose titrated to a resting heart rate of 50-60 beats/min. Studies have demonstrated the cardioprotective effects of atenolol and bisoprolol in the perioperative setting.
Postoperative cardiac management
The peak incidence of postoperative ischemia occurs within 48 hours of surgery. In more than 90% of patients, the ischemia is clinically silent. Because postoperative ischemia can be more deleterious than ischemia detected at other times, the perioperative use of beta-blockers and high-dose narcotic analgesics to reduce postoperative pain is recommended.
Prevention
Antimicrobial prophylaxis is indicated prior to invasive dental or surgical procedures for patients with the following cardiac conditions:
-
A prosthetic heart valve
-
A prior history of infective endocarditis
-
A cyanotic congenital heart defect
-
A surgically constructed systemic or pulmonary conduit
-
Hypertrophic cardiomyopathy
-
Mitral valve prolapse with regurgitation, valve thickening, or both
Background
The worldwide elderly population with its associated health concerns is expanding rapidly. Globally, the proportion of individuals older than 80 years averages 5%. In the developed world, almost 15% of individuals are older than 80 years; the proportion is expected to increase to 25% by 2050. [2] This aging population has associated comorbidities; consequently, clinicians are often asked to evaluate the preoperative cardiac risk status of this high-risk population.
See the algorithm for preoperative cardiac assessment below.
The cardiovascular systems of patients who undergo general anesthesia and noncardiac surgical procedures are subject to multiple stresses and complications. A previously stable patient may decompensate postoperatively, leading to significant morbidity and mortality. A substantial number of all deaths among patients who undergo noncardiac surgery are caused by cardiovascular complications.
Each year, approximately 30 million individuals in the United States undergo noncardiac surgery. Approximately one third have cardiac disease or major cardiac risk factors. Estimated rates of serious perioperative cardiac morbidity vary from 1% to 10%. The incidence of perioperative myocardial infarction (MI) is increased 10- to 50-fold in patients who have had previous coronary events.
Cardiac risk stratification allows clinicians to group patients into various risk categories; therefore, low-risk patients can be spared further testing, whereas intermediate- and high-risk patients should undergo preoperative investigations and treatment to reduce overall cardiac perioperative morbidity and mortality. [3]
Perioperative Cardiac Physiology
Cardiac effects of general anesthesia
The cardiovascular effects of general anesthesia include changes in the arterial and central venous pressures, cardiac output, and varying heart rhythms, which occur by the following mechanisms: decreased systemic vascular resistance, decreased myocardial contractility, decreased stroke volume, and increased myocardial irritability.
Induction of general anesthesia lowers systemic arterial pressures by 20-30%, tracheal intubation increases the blood pressure by 20-30 mm Hg, and agents such as nitric oxide lower cardiac output by 15%.
The use of fentanyl, sufentanil, or alfentanil results in less myocardial depression compared with inhaled anesthetics. Yet, these intravenous (IV) agents still cause venodilation, thus reducing preload and, hence, depressing cardiac output. Patients with congestive heart failure (CHF) are particularly sensitive to these hemodynamic changes. By increasing the preoperative volume status and applying the Frank-Starling principle, this decrease in cardiac output can be offset.
Additionally, inhalational and IV anesthetics along with muscle relaxants can be detrimental by sensitizing the myocardium to circulating catecholamines. As a result of the stress of the surgical procedure, circulating catecholamine levels are elevated, thereby increasing the risk of ventricular ectopy.
Cardiac effects of regional anesthesia
Both epidural and spinal anesthetics cause arteriodilation and venodilation by blocking sympathetic outflow, decreasing preload and, ultimately, reducing cardiac output. To offset this deleterious effect, the clinician may volume load the patient preoperatively. However, this intervention increases the risk of postoperative CHF by 10-15%.
Although many clinicians believe that regional anesthesia is safer than general anesthesia, randomized studies comparing the two modalities have shown no difference in cardiopulmonary complications or mortality. Combined epidural and general anesthesia with analgesia for pain control may attenuate sympathetic hyperactivity, reduce the need for additional parenteral analgesia postoperatively, improve postoperative pulmonary function, and reduce the duration of stay in the intensive care unit following surgery. [4]
Patient- and Procedure-Related Factors
Patient-related factors
Hypertension
Approximately 50% of patients in the United States who are aware they have hypertension are either not treated or inadequately treated with pharmacologic therapy.
In the perioperative period, poorly controlled hypertension is associated with an increased incidence of ischemia, left ventricular dysfunction, arrhythmia, and stroke. Patients with hypertension are at a higher risk for labile blood pressure and for hypertensive emergencies during surgery and immediately following extubation. Patients should continue taking preoperative antihypertensive medications throughout the entire perioperative period. The goal should be a systolic blood pressure less than 140 mm Hg and a diastolic blood pressure lower than 90 mm Hg before proceeding with elective surgery in the ideal situation.
In any patient with stage 3 hypertension (ie, >180/110 mm Hg), blood pressure should be well controlled prior to surgery. Intravenous esmolol, labetalol, nitroprusside, or nitroglycerin may be used for acute episodes of hypertension, whereas calcium-channel blockers or angiotensin-converting enzyme (ACE) inhibitors may be used in less acute situations.
Congestive heart failure
The mortality rate following noncardiac surgery increases with advancing New York Heart Association stage. The perioperative mortality rate appears to be more dependent on the patient's condition at the time of surgery than on the myocardial depressant effects of the anesthesia. CHF should be aggressively and adequately treated before the patient undergoes major elective surgery. Therapy is aimed at reducing ventricular filling pressures in addition to improving cardiac output.
Medications proven to show a morbidity and mortality benefit include ACE inhibitors, beta-blockers, spironolactone, and angiotensin receptor blockers (ARBs). Digoxin and diuretics have been shown to improve morbidity rates without reducing mortality rates. Detsky et al suggest that patients with decompensated CHF should be stabilized for at least 1 week before undergoing elective surgery. [5, 6]
Ischemic heart disease
Ischemic heart disease (IHD) is a major determinant of perioperative morbidity and mortality. During the 1970s, several studies reported a 30% risk of reinfarction or cardiac death for patients undergoing surgery within 3 months of an MI, 15% when surgery was performed 3-6 months after an infarction, and 5% when the operation was performed 6 months later. However, this traditional definition has been replaced by the consensus of the American College of Cardiology (ACC) Cardiovascular Database Committee. In particular, an acute MI is now defined as occurring within 7 days, a recent MI is defined as occurring within 7 days to 1 month, and a history of prior MI refers to an event occurring more than 1 month previously.
True lifesaving procedures should be performed regardless of cardiac risk, but consideration should be given to performing elective surgery 4-6 weeks after an MI. In patients requiring semiurgent surgery, the patient's risk should be evaluated with prognostic studies (see Preoperative Risk Assessment). Shah et al revealed that 25% of patients with unstable angina had an MI after noncardiac procedures. [7] Medical therapy, revascularization, or both will be necessary to ameliorate this risk factor.
No evidence-based trials compare perioperative cardiac outcomes after noncardiac surgery for individuals treated with preoperative percutaneous coronary intervention (PCI) versus medical therapy. Indications for PCI in the perioperative setting should adhere to the ACC/American Heart Association (AHA) guidelines established for PCI in general. [8] In the setting of PCI without stenting, wait 1 week prior to surgery. In the setting of PCI with a coronary stent, wait 4-6 weeks prior to noncardiac surgery.
Aortic stenosis
Aortic stenosis (AS) is associated with a 13% risk of perioperative death. Risk varies based on the severity of AS. The death rate associated with critical AS is approximately 50%.
While taking a history, the clinician should inquire about symptoms of syncope, angina, and dyspnea. During the examination, assess for a crescendo-decrescendo murmur in the right intercostal space radiating to the carotids. Pulsus parvus et pulsus tardus, a soft second heart sound (S2), a late peaking murmur, brachioradial delay, and an apical-carotid delay should raise the suggestion of AS. Critical AS is often characterized by an absent S2 and pulsus parvus et tardus. Echocardiography that reveals an aortic valve area less than 0.7 cm2 and/or a mean gradient of 50 mm Hg/peak gradient of 80 mm Hg is deemed critical stenosis. The clinician should delay surgery, except for emergencies, and should consider preoperative valve replacement in these patients.
Anticoagulation
The clinician must remember that patients with atrial fibrillation (AF) and prosthetic heart valves are on anticoagulation therapy. Warfarin therapy should be discontinued 4-5 days before elective surgery, given its half-life. Patients at high risk for thromboembolic events include those with prosthetic valves in the mitral position, AF associated with mitral valve disease, and a history of thromboembolism. Such patients should be admitted for IV heparin treatment. Outpatient therapy with preoperative low–molecular-weight heparin (LMWH) instead of conventional unfractionated IV heparin is often used, although no randomized controlled trials have validated this protocol. Patients with highly thrombotic valves (eg, Starr-Edwards valve), two prosthetic valves, or recent arterial embolism should be considered for standard IV heparin therapy perioperatively.
Procedure-related factors
The clinician must consider two factors when assessing the patient's cardiovascular risk: (1) the type of surgery, and (2) the hemodynamic stress associated with the procedure. Generally, the more extensive the surgical procedure, the greater the physiologic stress, the more significant the postoperative pain, and the greater the incidence of cardiac complications. Surgical procedures may be classified as follows:
-
High risk (>5% rate of perioperative death or MI) - Emergency major operations (particularly in elderly patients), peripheral vascular or aortic surgery, and prolonged procedures with large amounts of blood loss involving the abdomen, thorax, head, and neck
-
Intermediate risk (1-5% rate of perioperative death or MI) - Carotid endarterectomy and urologic, orthopedic, uncomplicated abdominal, head, neck, and thoracic operations
-
Low risk (< 1%) - Cataract removal, endoscopy, superficial procedure, and breast surgery
Preoperative Risk Assessment
A preoperative cardiac risk assessment involves obtaining a thorough history and physical examination, along with a baseline ECG. Established cardiac diseases, including IHD, hypertension, arrhythmia, valvular heart disease, CHF, and the presence of a pacemaker or implantable defibrillator should be sought as part of the patient's history.
A number of studies pertaining to cardiac risk stratification have been published over the past three decades, including the Goldman, Detsky, and Eagle indices. Updated ACC/AHA guidelines for the perioperative cardiovascular evaluation for noncardiac surgery are available. A stepwise strategy that includes the assessment of clinical markers, prior cardiac evaluation and management, functional capacity in mets, and surgery-specific risk is followed. [9, 10]
The following clinical markers are assessed:
-
Major clinical predictors - Unstable coronary syndrome, decompensated CHF, significant arrhythmia, and severe valvular disease [11]
-
Intermediate clinical predictors - Mild angina, prior MI, compensated or prior CHF, diabetes mellitus, and renal insufficiency
-
Minor clinical predictors - Advanced age, abnormal findings on echocardiography, rhythm other than sinus, history of stroke, low functional capacity, and uncontrolled hypertension
Functional capacity can be assessed as follows:
-
Poor functional class (< 4 mets) - Energy expended during activities, including dressing, eating, and walking around the house
-
Adequate functional class (>4 mets) - Energy expended during activities, including walking up a flight of stairs, scrubbing floors, and swimming
For assessment of surgery-specific risk, see the following:
-
See Patient- and Procedure-Related Factors.
-
See the algorithm presented in the image shown below.
Noninvasive Cardiac Evaluation
Tests for risk stratification
Dobutamine stress echocardiography
Dobutamine is a beta-receptor agonist that increases both heart rate and contractility. In combination with echocardiography, regional wall abnormalities and, thus, ischemia may be assessed. The negative and positive likelihood ratios of dobutamine stress echocardiography for detecting CAD are 0 and 4.5, respectively. Of note, avoid dobutamine stress echocardiography testing in patients with a history of ventricular tachyarrhythmia (see image below).
 Perioperative cardiac management. The transthoracic echocardiogram illustrates a parasternal long axis view of the left ventricle with preserved cardiac function.
Perioperative cardiac management. The transthoracic echocardiogram illustrates a parasternal long axis view of the left ventricle with preserved cardiac function.
Dipyridamole thallium imaging
Intravenous dipyridamole increases coronary blood flow to the myocardium two- to threefold. Viable myocardial cells take up thallium-201, a radionucleotide tracer, in proportion to blood flow. Hence, delayed thallium redistribution following dipyridamole administration helps identify areas of ischemia (see image below). The test has a negative predictive value (NPV) of 95-100% for CAD in patients having vascular surgery; negative results have a likelihood ratio (LR) of 0.12, whereas positive results have an LR of 3.02.
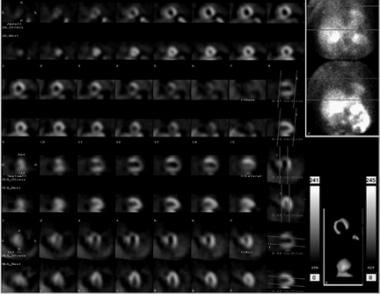 Perioperative cardiac management. The sestamibi perfusion scan illustrates reversible ischemia in the anterior wall of the myocardium, comparing rest and stress images.
Perioperative cardiac management. The sestamibi perfusion scan illustrates reversible ischemia in the anterior wall of the myocardium, comparing rest and stress images.
Of note, be cautious when performing dipyridamole thallium scanning in patients with an underlying history of reactive airway disease, including asthma and severe chronic obstructive pulmonary disease (COPD).
Coronary angiography
Studies to date have not evaluated the role of coronary angiography as a risk predictor. Coronary angiography should not be performed routinely in all vascular patients, but it is generally recommended for those individuals with clinical or noninvasive evidence of CAD, as determined by dobutamine echocardiography results or dipyridamole methoxyisobutyl isonitrile testing. Furthermore, indications for coronary artery bypass grafting (CABG) before noncardiac surgery are identical to those established by the ACC/AHA guidelines for CABG, in particular left main disease and critical three-vessel disease with a reduced ejection fraction (EF) (see the following image).
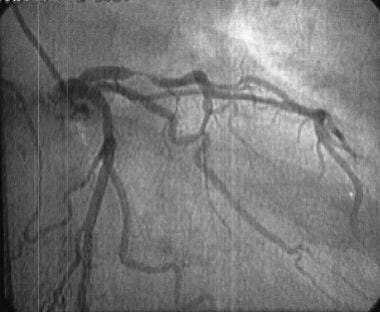 Perioperative cardiac management. Coronary angiogram revealing severe left circumflex and left anterior descending disease.
Perioperative cardiac management. Coronary angiogram revealing severe left circumflex and left anterior descending disease.
Tests not recommended for risk stratification
Transthoracic echocardiography
Noninvasive assessment of left ventricular systolic dysfunction was once considered predictive of increased perioperative cardiac complications because the measurement was considered an indirect measurement of left heart failure. This finding no longer holds true because TTE does not provide any further data over the clinical cardiac examination for predicting perioperative cardiac complications. Although a high EF is associated with a low perioperative cardiac risk, even a normal EF cannot exclude severe CAD. TTE does play an important role in evaluating the severity of stenotic and regurgitant valvular lesions.
Exercise treadmill testing
Exercise stress testing is useful in patients who are able to exercise, but a significant percentage of patients undergoing noncardiac surgery are unable to reach the maximal predicted heart rate, given the magnitude of their concomitant vascular disease. In individuals who are able to walk the treadmill, the sensitivity and specificity for predicting CAD are 65% and 85%, respectively.
Studies have confirmed that exercise stress testing does not provide a high NPV. [12] Physiologically, exercise increases the heart rate and systemic vascular resistance, thus increasing oxygen consumption by the myocardium. Therefore, a positive test result indicates a high risk of developing ischemia perioperatively. However, many ischemic events that occur intraoperatively are not associated with changes in the heart rate or blood pressure; therefore, the minimal threshold of myocardial oxygen utilization to evoke ischemia is not reached, and the significance of a negative stress test result is misleading.
Ambulatory electrocardiographic monitoring
Although preliminary data suggested that the absence of ST depression had an NPV of 99%, this finding no longer holds true.
Cardiac Management Perioperatively
Preoperative and intraoperative cardiac management
The stress of surgery results in the release of catecholamines. Increasing the rate-pressure product may predispose the patient to a cardiac event. Mangano et al evaluated the role of atenolol perioperatively in reducing long-term cardiac morbidity and mortality. [13] Patients received a beta-blocker if they had known CAD or met two of the following criteria: older than 65 years, hypertension, total cholesterol level higher than 6.2 mmol/L, smoking history, or diabetes mellitus.
Atenolol produced a 15% absolute risk reduction in the end points of MI, unstable angina, CHF requiring hospitalization, or death at 6 months and reduced mortality at 6 months and 2 years in noncardiac surgery.
Similarly, another randomized controlled trial evaluated the cardioprotective effects of bisoprolol in high-risk patients undergoing vascular surgery. The study was stopped early because of the dramatic results. Poldermans et al screened 1351 patients awaiting vascular surgery and included those who had one or more cardiac risk factors and positive results on a dobutamine echocardiography study. [14] The 112 patients remaining were randomized to receive either standard care or standard care plus bisoprolol. Bisoprolol, at a dose of 10 mg PO (orally) qd given 1 week preoperatively and continued for 1 month postoperatively, reduced the incidence of perioperative death from cardiac causes and nonfatal MI.
Consequently, when possible, beta-blockers should be started 1 week before elective surgery, with the dose titrated to a resting heart rate of 50-60 beats/min. As for the use of nitrates, digitalis, and calcium-channel blockers, no studies have evaluated their use in the perioperative state.
Postoperative management
Historically, postoperative MI carried a grave prognosis (ie, >50% mortality rate). Postoperative ischemia is well characterized, with its peak incidence within 48 hours of surgery. Postoperative ischemia is clinically silent in more than 90% of cases. The Perioperative Ischemia Research Group evaluated the use of continuous echocardiographic monitoring perioperatively and found that ischemia occurred most frequently on postoperative days 1 and 2 (ie, 20% preoperative, 25% intraoperative, 55% postoperative). Because postoperative ischemia can be more deleterious than ischemia detected at other times, interventions, including the perioperative use of beta-blockers and high-dose narcotic analgesia to reduce postoperative pain, are recommended.
The PeriOperative Ischemic Evaluation (POISE) trial was a cohort study of 8351 patients undergoing noncardiac surgery who had troponin levels routinely checked 3 days after surgery. MI was defined as elevated troponin with clinical, electrocardiographic, or imaging evidence of myocardial ischemia. The 30-day mortality rate was five times higher in patients with postoperative MI (11.6% vs 2.2%) and was similar between those with and without ischemic symptoms. [15]
A study by Puelacher et al that included 2018 patients who underwent noncardiac surgery reported that perioperative myocardial injury occurred in 16% of surgeries. The adjusted risk of death with perioperative myocardial injury was almost three times higher at 30 days (hazard ratio [HR], 2.7) and almost two times higher at 1 year (HR, 1.6). [16, 17]
Endocarditis Prophylaxis
According to the revised guidelines of the AHA, [18] cardiac conditions in which antimicrobial prophylaxis is indicated prior to invasive dental or surgical procedures include the following:
-
Prosthetic heart valve
-
Prior history of infective endocarditis
-
Cyanotic congenital heart defect
-
Surgically constructed systemic or pulmonary conduit
-
Mitral valve prolapse with regurgitation, valve thickening, or both
Endocarditis prophylaxis is not recommended for the following:
-
Atrial septal defect
-
Surgically repaired ventricular septal defect
-
Patent ductus arteriosus
-
Isolated mitral valve prolapse
-
Mild tricuspid regurgitation
-
Previous rheumatic fever or Kawasaki disease without valvular dysfunction
-
Cardiac pacemaker
-
Implantable defibrillator
The following antimicrobial regimen is suggested for prophylaxis:
-
Dental, oral, or upper respiratory tract procedures - Amoxicillin 2 g PO 1 hour prior to the procedure; if the patient is allergic to penicillin, alternatives include clindamycin 600 mg PO, cephalexin 2 g PO, or azithromycin 500 mg PO 1 hour prior to the procedure.
-
Genitourinary or gastrointestinal procedures - Ampicillin 2 g IV and gentamicin 1.5 mg/kg 30 minutes prior to the procedure, followed by amoxicillin 1 g PO/IV/IM (intramuscularly) 8 hours later; if the patient is allergic to penicillin, alternatives include vancomycin 1 g IV and gentamicin 1.5 mg/kg 1-2 hours prior to the procedure.
Questions & Answers
Overview
What is perioperative cardiac management?
What are cardiac effects of general anesthesia relevant to perioperative cardiac management?
What are cardiac effects of regional anesthesia relevant to perioperative cardiac management?
How does hypertension affect perioperative cardiac management?
How does congestive heart failure affect perioperative cardiac management?
How does ischemic heart disease (IHD) affect perioperative cardiac management?
How does aortic stenosis (AS) affect perioperative cardiac management?
How does anticoagulation affect perioperative cardiac management?
How is surgical risk assessed during perioperative cardiac management?
How is preoperative cardiac risk assessed?
What is the role of clinical markers in the preoperative cardiac risk assessment?
What is the role of functional capacity in the preoperative cardiac risk assessment?
What is the algorithm for preoperative cardiac risk assessment?
What is the role of dobutamine stress echocardiography in perioperative cardiac management?
What is the role of dipyridamole thallium imaging in perioperative cardiac management?
What is the role of coronary angiography in perioperative cardiac management?
What is the role of transthoracic echocardiography in perioperative cardiac management?
What is the role of exercise treadmill testing in perioperative cardiac management?
What is the role of ambulatory electrocardiographic monitoring in perioperative cardiac management?
What is included in preoperative and intraoperative cardiac management?
What is included in postoperative cardiac management?
What is the role of antimicrobial prophylaxis in the perioperative management of cardiac patients?
-
Perioperative cardiac management. Algorithm for preoperative cardiac assessment.
-
Perioperative cardiac management. The transthoracic echocardiogram illustrates a parasternal long axis view of the left ventricle with preserved cardiac function.
-
Perioperative cardiac management. The sestamibi perfusion scan illustrates reversible ischemia in the anterior wall of the myocardium, comparing rest and stress images.
-
Perioperative cardiac management. Coronary angiogram revealing severe left circumflex and left anterior descending disease.