Background
Postoperative pulmonary complications contribute significantly to overall perioperative morbidity and mortality rates. Such complications account for about 25% of deaths occurring within 6 days of surgery. The frequency rate of these complications varies from 5-70%. This wide range is due to variations among studies in the definition of postoperative pulmonary complications, as well as variability in patient- and procedure-related factors.
The goal of perioperative pulmonary management is to identify patients at high risk of significant postoperative pulmonary complications, so that appropriate interventions can be provided to minimize that risk. In most cases, even in high-risk patients, the procedure can be performed safely as planned, but occasionally postponement, modification, or cancellation are warranted.
One of the more comprehensive lists of postoperative pulmonary complications includes fever (due to microatelectasis), cough, dyspnea, bronchospasm, hypoxemia, atelectasis, hypercapnia, adverse reaction to a pulmonary medication, pleural effusion, pneumonia, pneumothorax, and ventilatory failure. [1] Such a broad definition risks including complications that have no clinical significance. Most investigators thus define a postoperative pulmonary complication as an abnormality that produces identifiable disease or dysfunction, is clinically significant, and adversely affects the clinical course.
 Image in a 49-year-old woman with pneumococcal pneumonia. The chest radiograph reveals a left lower lobe opacity with pleural effusion.
Image in a 49-year-old woman with pneumococcal pneumonia. The chest radiograph reveals a left lower lobe opacity with pleural effusion.
Determining which complications fit this definition is challenging, but likely included are: atelectasis, infection (eg, bronchitis, pneumonia), prolonged mechanical ventilation and respiratory failure, exacerbation of an underlying chronic lung disease, and bronchospasm. When such a definition is employed, postoperative pulmonary complications prolong the hospital stay by an average of 1-2 weeks, and are likewise associated with increased morbidity and mortality.
The risk of postoperative complications varies with the type of surgery being performed. Pulmonary complications occur much more often than cardiac complications in patients undergoing elective surgery to the thorax and upper abdomen. Operations at sites farther from the diaphragm are associated with a much lower incidence of postoperative pulmonary complications. Preoperative evaluation for patients undergoing lung resection (ie, for lung cancer) differs considerably from that for those undergoing nonresectional surgery.
Postoperative pulmonary complications are also more common in patients with preexisting lung disease, medical comorbidities, poor nutritional status, overall poor health, and in those who smoke. Not all of these risk factors are modifiable, although strategies exist to reduce the risk of postoperative pulmonary complications even among high-risk patients.
For excellent patient education resources, visit eMedicineHealth's Lung Disease and Respiratory Health Center. Also, see eMedicineHealth's patient education articles Pulmonary Embolism, Bronchitis, Bacterial Pneumonia, ChronicObstructivePulmonaryDisease(COPD), and Deep Vein Thrombosis (Blood Clot in the Leg, DVT).
Perioperative Pulmonary Physiology
Respiratory effects of general anesthesia
Anesthetic agents are associated with marked alterations in respiratory drive. Such agents cause a diminished response to both hypercapnia and hypoxemia. In combination with neuromuscular blockers, anesthetic agents cause diaphragm and chest wall relaxation, which results in a marked reduction in the functional reserve capacity and, thereby, thoracic volume.
This decrease in lung volume promotes atelectasis in the dependent lung regions and persists for more than 24 hours in 50% of patients. Consequently, arterial hypoxemia occurs from ventilation-perfusion (V-Q) mismatching and increased shunt fraction.
Postoperative respiratory physiology in upper abdominal and thoracic surgery
Thoracic and upper abdominal surgery is associated with a reduction in vital capacity by 50% and in functional residual capacity by 30%. Diaphragmatic dysfunction, postoperative pain, and splinting cause these changes.
Following upper abdominal surgery, patients shift to a breathing pattern with which ribcage excursions and abdominal expiratory muscle activities increase. This shift is attributed to decreased central nervous system (CNS) output to the phrenic nerves, thus inhibiting diaphragmatic stimulation. A reflex mechanism arising from the sympathetic, vagal, or splanchnic receptors is thought to be responsible. In humans, this reflex inhibition is partially reversed by epidural anesthesia.
Following upper abdominal and thoracic surgery, patients maintain adequate minute volume, but the tidal volume is smaller and the respiratory rate increases (ie, rapid shallow breathing). These breathing patterns, along with the residual effects of anesthesia and postoperative narcotics, inhibit cough, impair mucociliary clearance, and contribute to the risk of postoperative pneumonia.
Other factors that may contribute to increased respiratory complications include electrolyte imbalance (eg, hypokalemia, hypophosphatemia, hypocalcemia), general debilitation, and underlying lung disease (eg, chronic obstructive pulmonary disease [COPD]).
 Posteroanterior (PA) and lateral chest radiograph in a patient with severe Chronic obstructive pulmonary disease (COPD). Hyperinflation, depressed diaphragms, increased retrosternal space, and hypovascularity of lung parenchyma is demonstrated.
Posteroanterior (PA) and lateral chest radiograph in a patient with severe Chronic obstructive pulmonary disease (COPD). Hyperinflation, depressed diaphragms, increased retrosternal space, and hypovascularity of lung parenchyma is demonstrated.
Patient- and Procedure-Related Risk Factors
Numerous studies have been designed to investigate the relationship between various risk factors and postoperative complications. One of the larger ones was designed as a prospective cohort study where postoperative pulmonary complications ascertained by an investigator blinded to perioperative variables was conducted to determine the risk factors for pulmonary complications after elective nonthoracic surgery. [2]
Of 1055 consecutive patients, 28 (2.7%) suffered a postoperative pulmonary complication within 7 days of surgery; 13 developed respiratory failure that required ventilatory support; 9 developed pneumonia; 5 developed atelectasis that required bronchoscopic intervention; and 1 developed pneumothorax that required intervention. [2] Multivariate analyses revealed that 4 factors were independently associated with increased risk of pulmonary complications: age (odds ratio [OR] 5.9 for age 65 y or older), positive cough test (OR 3.8), perioperative nasogastric tube (OR 7.7), and duration of anesthesia (OR 3.3 for operations lasting at least 2.5 h). [2]
A systematic review of the performance of variables commonly used in the prediction of postoperative pulmonary complications in patients undergoing nonthoracic surgery was performed by Fisher et al. [3] Seven studies fulfilled the investigators' inclusion criteria, and the incidence of postoperative pulmonary complications varied from 2% to 19%. Of 28 preoperative or operative risk factors evaluated in the 7 studies, 16 were associated significantly with postoperative pulmonary complications. [3] Only 2 (duration of anesthesia and postoperative nasogastric tube placement) were significant in more than one study. However, these 16 variables had only modest predictive value. Neither hypercapnia nor reduced spirometry values were independently associated with an increased risk of postoperative pulmonary complications.
Patient-related risk factors
Age
Age appears to be an independent risk factor for postoperative pulmonary complications. [4, 5] This conclusion is controversial, as several other studies have shown that age is not a predictor for postoperative pulmonary complications. Importantly, acceptable operative mortality rates can be achieved in older patients.
In a study of patients older than 80 years, the overall 30-day mortality rate was 6.2%, and the mortality rate for patients who belonged to American Society of Anesthesiologists (ASA) class II scale was less than 1%. [6] As age is obviously a nonmodifiable risk factor, and the potential risk of complications does not invariably translate into increased mortality, surgery should not be declined because of advanced age alone.
Obesity
Obesity (ie, body mass index of >27 kg/m2) causes a reduction in lung volume, ventilation-perfusion mismatch, and relative hypoxemia, which are accentuated after surgery. In severe cases, obesity is associated with pulmonary hypertension, cor pulmonale, and hypercapnic respiratory failure (Pickwickian syndrome). Although some studies suggest that obesity increases the risk of postoperative pulmonary complications, others suggest that obesity is not an independent risk factor.
In a review article, the risk of postoperative pulmonary complications was not excessive in 7 studies of obese patients who underwent abdominal or peripheral procedures. [7] Several other studies have also reported no association between obesity and postoperative pulmonary complications, including studies in patients undergoing laparoscopic cholecystectomy, [8] hip fracture surgery, [9] and laparoscopic colectomy. [10] A recent study demonstrated an increased risk of pulmonary insufficiency and pneumonia among obese patients undergoing lobectomy for lung cancer (absolute risk increase of 2-3%). [11] The risk of pulmonary complications was higher among patients with BMI 35 or above, but not among obese patients with a lower BMI, undergoing cardiac surgery. [12]
General health status
The ASA classification and the Goldman Cardiac Risk Index have helped clinicians to successfully predict pulmonary risk. Patients who have poor exercise capacity are at increased risk of developing postoperative pulmonary complications. In a study by Gerson et al, an inability to raise the heart rate with simple exercise predicted a pulmonary complication rate of 79%. [13]
Dependent functional status, low albumin, and weight loss are also specific and independent risk factors for complications. [4] A serum albumin level less than 3.5 mg/dL is an independent risk factor for postoperative pulmonary complications and should be checked in individuals with suspected hypoalbuminemia or at least one other risk factor for complications. [14] The risk of complications increases continuously at serum albumin levels less than 3.5 mg/dL. [15]
Smoking
Patients who currently smoke have a 2-fold increased risk of postoperative complications, even in the absence of COPD. [4] The risk is highest in patients who smoked within the last 2 months. Patients who quit smoking for more than 6 months have a risk similar to those who do not smoke, although the risk of postoperative pneumonia appears to remain elevated up to 1 year after smoking cessation. [4]
COPD
This condition is one of the most important risk factors for postoperative pulmonary complications. Patients with severe COPD (forced expiratory volume in 1 s [FEV1] < 40% predicted) are 6 times more likely to have a major postoperative complication. Similarly, an FEV1< 60% predicted was found to be an independent predictor of increased mortality in patients undergoing coronary artery bypass graft (CABG) procedures. [16]
Despite the increased risk, a prohibitive level of pulmonary function for an absolute contraindication is not apparent. The benefits of surgery must be weighed against these complications. A careful preoperative evaluation of patients with COPD should include identification of high-risk patients and aggressive treatment. Elective surgery should be deferred in patients who are symptomatic, have poor exercise capacity, or have acute exacerbation.
Asthma
Asthma increases the risk of bronchospasm, hypoxemia, hypercapnia, inadequate cough, atelectasis, and pulmonary infection following surgery. [17] Well-controlled asthma does not appear to pose an increased risk of these complications, but suboptimal asthma control does. [18] Optimal asthma control is defined as the absence of (or only rare) symptoms and a forced expiratory volume in 1 second (FEV1) of greater than 80% of predicted or personal best.
Pulmonary hypertension
Patients with pulmonary hypertension experience a higher mortality and morbidity rate following noncardiac surgery than other high-risk historic comparator groups, with a higher New York Heart Association (NYHA) class and other markers of severe pulmonary hypertension being independent risk factors in this cohort. [19] Patients with pulmonary hypertension have an increased risk of congestive heart failure, hemodynamic instability, sepsis, and respiratory failure, and they had longer ICU and hospital length of stay and increased readmission rates compared with patients without pulmonary hypertension undergoing noncardiac surgery. [20] Worse outcomes have also been documented following coronary artery bypass graft (CABG).
Features associated with an increased risk among patients with pulmonary hypertension include: history of pulmonary embolism, obstructive sleep apnea, chronic kidney disease, coronary artery disease, New York Heart Association (NYHA) class 2 or above, right-axis deviation or right ventricular hypertrophy on ECG, and poor hemodynamic parameters (including right ventricular systolic pressure >70 mm Hg, right atrial dilation, decreased left ventricular ejection fraction). Surgery, aside from minor procedures, should be avoided in patients with evidence of right ventricular failure (elevated right atrial pressure or decreased cardiac output). [21]
Interstitial lung disease
Patients with pulmonary fibrosis experienced a higher rate of morbidity and mortality following resection for lung cancer. About 50% of patients with interstitial lung disease with a high composite physiologic index (CPI >40) developed postoperative lung injury. [22] Another scoring system (incorporating operative approach, preoperative immunosuppressive therapy, age, and preoperative ICU admission) showed good discrimination for mortality following lung biopsy. [23]
A review article summarizes the limited data concerning the increased risk of an acute exacerbation of idiopathic pulmonary fibrosis following thoracic surgery (lung resection for lung cancer or surgical lung biopsy). Low forced vital capacity, low diffusing capacity, ongoing exacerbation at the time of surgery, and larger extent of resection have all been associated with a higher risk of and/or mortality from postoperative exacerbation. [24]
The risk of exacerbation also seems to be higher among patients with a greater degree of radiographic fibrosis, particularly on the nonoperated lung. [25]
Sleep apnea
Obstructive sleep apnea is present in 3-5% of the general population, and the prevalence among surgical patients is likely significantly higher. Based on questionnaires, 24-41% of surgical patients are at risk for obstructive sleep apnea. The vast majority of these patients have not been diagnosed preoperatively. [26] A study by Cordovani et al reported that the majority of anesthesiologists surveyed continue to rely on clinical suspicion alone to identify obstructive sleep apnea. [27]
Patients with sleep apnea are at increased risk of developing deterioration of sleep-disordered breathing, severe hypoxemia, and hypercapnia in the postoperative period. The risk of aspiration pneumonia, acute respiratory distress syndrome, and pulmonary embolism were all greater among patients with obstructive sleep apnea. Although this risk is increased even in patients undergoing lower-risk (orthopedic) operations, postoperative complications do not seem to be higher in patients with obstructive sleep apnea undergoing outpatient surgery. [26]
Individuals with sleep apnea who are also obese may present difficulties with endotracheal intubation or early postoperative upper airway obstruction, requiring reintubation or other therapies.
In patients with known or possible sleep apnea, the intraoperative and postoperative use of sedatives and narcotics should be minimized. Careful monitoring (continuous pulse oximetry and/or capnometry) in the postoperative period is required for worsening of sleep apnea, development of airway obstruction, or carbon dioxide retention. Patients with multiple postanesthesia care events (bradypnea, apnea, desaturation) are at increased risk for postoperative desaturation and respiratory complications. [26]
In patients who may have sleep apnea, the diagnosis should be confirmed and the severity should be assessed preoperatively with a formal polysomnographic sleep study. As obtaining preoperative polysomnography in all patients at risk presents a challenge, the use of questionnaires to identify patients at risk of moderate-to-severe obstructive sleep apnea (specifically, the STOP-BANG [Snoring? Tired? Observed? Pressure?–BMI >35? Age >50 y? Neck size large? Gender=Male?] questionnaire) may be useful to select higher-risk patients for preoperative testing. The STOP-BANG questionnaire includes 8 questions pertaining to snoring, daytime hypersomnolence, witnessed apneas, hypertension, BMI, age, neck circumference, and sex (with 3 or more positive answers being associated with a high risk of obstructive sleep apnea).
The severity of sleep apnea is judged based on the apnea-hypopnea index and the lowest oxygen saturation value during sleep. Whenever possible, patients should be adequately treated preoperatively with nasal continuous positive airway pressure (CPAP) therapy. Further, patients with sleep apnea often benefit from regional anesthesia rather than general anesthesia.
If polysomnography cannot be performed preoperatively, nocturnal oximetry testing is another option to identify patients with clinical features suggestive of OSA at increased risk of complications. Specifically, those with 5 or more desaturation events per hour had a 15% incidence of complications (mostly pulmonary), while those with fewer desaturation events had a complication rate around 3%. [28]
Neurologic impairment
Patients with impaired sensorium or residual deficits from a previous stroke have an increased risk of postoperative pneumonia and respiratory failure. [4]
Immunosuppression
Chronic steroid use is associated with an increased risk of postoperative pneumonia. Daily use of alcohol within 2 weeks of surgery is associated with an increased risk of postoperative pneumonia and respiratory failure. Insulin-treated diabetes is associated with an increased risk of postoperative respiratory failure. [4]
Procedure-related risk factors
Surgical site
The incidence of postoperative pulmonary complications is inversely related to the distance of the surgical incision from the diaphragm. The complication rates for upper abdominal surgery range from 17% to 76%. For lower abdominal surgery, the rate is 0-5%. For thoracic surgery, the rate is 19-59%. Abdominal aortic aneurysm repair is associated with the highest risk of postoperative pulmonary complications. [4]
Duration of surgery
Patients undergoing procedures lasting longer than 3-4 hours have a higher incidence rate of pulmonary complications (40%) compared with those undergoing surgeries lasting shorter than 2 hours (8%).
Type of anesthesia
Data are inconsistent about whether the pulmonary complication rate is lower with spinal or epidural anesthesia compared with general anesthesia. A study published by Celli et al reported no difference in patients anesthetized with spinal or general anesthesia for abdominal surgery. [29] An earlier study of high-risk patients showed that the rate of respiratory failure was significantly higher with general anesthesia. [30]
Several other studies found high rates of respiratory failure and other postoperative complications in patients undergoing general anesthesia compared with spinal or epidural anesthesia. [31, 32] Spinal or epidural anesthesia, in conjunction with general anesthesia, may be associated with a lower risk of postoperative pneumonia, venous thromboembolic disease, myocardial infarction, renal failure, and respiratory depression. [33] Patients who received epidural analgesia following abdominal aortic aneurysm repair had fewer complications than those receiving parenteral opioids. [34]
These results suggest that the addition of neuraxial anesthesia, rather than avoidance of general anesthesia, may be the key to reducing pulmonary complications. In any case, spinal or epidural anesthesia is safe and should be considered in high-risk patients. Regional nerve block is associated with a low risk and, when feasible, should also be considered for high-risk patients. Residual neuromuscular blockade was more common with pancuronium than intermediate-acting agents (eg, atracurium or vecuronium), and pulmonary complications occurred more often among patients who experienced persistent weakness following administration of pancuronium. Intermediate-acting neuromuscular blocking agents should therefore be considered in high-risk patients.
Minimally invasive surgery
Laparoscopic abdominal surgery, particularly cholecystectomy, is associated with fewer postoperative pulmonary abnormalities and a shorter hospital stay. These techniques use small incisions, and the reduced manipulation of visceral organs minimizes the adverse effects on respiratory muscles. Laparoscopic surgery leads to a 23% decrease in forced vital capacity (FVC) and a 16% decrease in FEV1, and it is associated with a lower incidence of complications compared with laparotomy [35] ; therefore, even patients with severe COPD can tolerate surgery.
Video-assisted thoracoscopic surgery uses much smaller incisions; consequently, the hospitalization time is substantially reduced. Smaller incisions, performed without separation of the ribs and resulting in less postoperative pain, lead to early ambulation and reduced pulmonary complications.
Preoperative Risk Assessment
History
Obtain a complete history and perform a complete physical examination to help identify risk factors for pulmonary complications. Seek any history of smoking, exercise intolerance, unexplained dyspnea, or cough. Note evidence of COPD, such as decreased breath sounds, wheezing, crackles, or a prolonged expiratory phase.
Workup
Pulmonary function tests
Several retrospective studies of routine preoperative pulmonary function test (PFT) results found only a marginal benefit in predicting postoperative complications in patients, other than those undergoing lung resection. A critical review reported that preoperative spirometry was not predictive of complications following abdominal surgery. [36] Therefore, pulmonary function studies should not be performed routinely in patients undergoing nonresectional surgery. Rather, testing should be restricted to those patients with unexplained dyspnea or exercise intolerance.
Preoperative identification of patients with asthma or COPD is important, as some individuals may benefit from specific preoperative interventions, but most can probably be detected by history, physical examination, and symptom-directed physiologic testing. Although data from studies by Kroenke et al [37] and Wong et al [38] indicated that patients with severe COPD have an overall high risk of postoperative complications (29%), the degree of physiologic impairment (eg, FEV1 or FVC) does not correlate with the risk of postoperative pulmonary complications. Therefore, nonresectional surgery should never be withheld based solely on results from PFT’s.
Arterial blood gases
Although hypercapnia has been associated with an increased risk of postoperative pulmonary complications in case series, a systematic review suggested that arterial blood gas (ABG) results are not independently predictive of complications. [3] Presumably patients with hypercapnia may be identified as high-risk on the basis of other criteria.
Chest radiography
Chest x-ray studies add little to the clinical evaluation in healthy patients. A preoperative chest x-ray is the most frequently ordered radiologic test. A systematic review of the literature on the value of screening chest x-rays to establish evidence to support guidelines for its use was performed by Joo et al. [39] The investigators reviewed 14 studies that met both inclusion criteria and exclusion criteria and identified chronic disorders, such as cardiomegaly and chronic obstructive pulmonary disease, in up to 65%. The rate of subsequent investigations was highly variable (4-47%). The findings led to a change in management in 10% of investigated patients. [39]
Postoperative pulmonary complications were also similar between patients who had preoperative chest x-rays (12.8%) and patients who did not (16%). [39] The recommendation from the Guidelines Association Committee that routine chest x-rays should not be performed routinely for preoperative evaluation in patients without risk factors is supported by Joo et al's study. [39]
Risk indices
A number of scoring systems have been devised to predict an individual patient’s risk of postoperative pulmonary complications. Each of these systems has potential limitations.
Postoperative pneumonia and respiratory failure risk indices
Arozullah et al derived and validated scoring systems to predict the risk of postoperative pneumonia and respiratory failure. [4, 40] The respiratory failure model has subsequently been revised. [41] These indices incorporate the following procedure and patient factors:
-
Procedure: Type of surgery, emergency surgery, general anesthesia
-
General health: Age, functional status, ASA class, serum albumin, weight loss
-
Immunosuppression: Chronic steroid use, alcohol use, insulin-treated diabetes
-
Lung disease: COPD, smoking, preoperative pneumonia, dyspnea
-
Other preexisting disease: Neurologic impairment, sepsis, ascites, bilirubin/AST, bleeding disorders/platelet count/Hct, WBC
-
Fluid status: Congestive heart failure, renal failure, sodium, blood urea nitrogen, preoperative transfusion
Points are assigned based on the relative risk of postoperative pulmonary complications associated with each factor. The points are totaled and the patient is assigned to a risk class (1 through 5 for pneumonia; low, medium, or high for respiratory failure). The risk of postoperative pneumonia and respiratory failure are less than 1% for patients in risk class 1 (or low risk), whereas patients in risk class 5 have a 15% risk of postoperative pneumonia and those in high-risk group have about a 7% risk of respiratory failure. These indices were derived from Veterans Affairs medical center data and thus may lack generalizability to younger patients and women. [40, 41]
More recently, Kinlin et al derived and validated a model to predict risk of pneumonia following coronary artery bypass surgery. This model was derived from a population with a higher proportion of women (about 30%) and shares a number of risk factors with the model described above. [42]
Kor et al developed a model to predict postoperative acute lung injury. Variables predicting acute lung injury/ARDS included high-risk vascular, cardiac, or thoracic surgery; COPD; diabetes; gastroesophageal reflux disease; and alcohol abuse. [43]
Pulmonary risk index/cardiopulmonary risk index
A combined cardiopulmonary risk index is proposed for risk stratification of pulmonary complications. Pulmonary risk factors have been added to the Goldman Cardiac Risk Index; patients with a combined score of greater than 4 points (of a total of 10) are 17 times more likely to develop complications. These pulmonary risk factors include the following:
-
Obesity (ie, body mass index >27 kg/m2)
-
Cigarette smoking within 8 weeks of surgery
-
Productive cough within 5 days of surgery
-
Diffuse wheezing within 5 days of surgery
-
FEV1/FVC ratio less than 70% and PaCO2 >45 mm Hg
This index was developed to predict the risk of pulmonary complications specifically following thoracic surgery. Only limited predictive ability was noted in a prospective validation study. [44]
American Society of Anesthesiology classification
This score is based on simple clinical criteria and is easy to quantify. Although subjective, assignment to class II through V indicates an increased level of severity and increased postoperative morbidity. The ASA classification, along with examples of each class, is described below:
-
ASA class I - A normal, healthy patient without organic, physiologic, or psychiatric disturbance (eg, healthy with good exercise tolerance)
-
ASA class II - A patient with controlled medical conditions without significant systemic effects (eg, controlled hypertension or controlled diabetes without systemic effects, cigarette smoking without COPD, anemia, mild obesity, age younger than 1 yr or older than 70 yrs, pregnancy)
-
ASA class III - A patient with medical conditions with significant systemic effects, intermittently associated with significant functional compromise (eg, controlled congestive heart failure, stable angina, old myocardial infarction, poorly controlled hypertension, morbid obesity, bronchospastic disease with intermittent symptoms, chronic renal failure)
-
ASA class IV - A patient with a medical condition that is poorly controlled, associated with significant dysfunction and is a potential threat to life (eg, unstable angina, symptomatic COPD, symptomatic congestive heart failure, hepatorenal failure)
-
ASA class V - A patient with a critical medical condition that is associated with little chance of survival with or without the surgical procedure (eg, multiorgan failure, sepsis syndrome with hemodynamic instability, hypothermia, poorly controlled coagulopathy)
-
ASA class VI - A patient who is brain dead and undergoing anesthesia care for the purposes of organ donation
ASA class I was associated with a mortality rate of 0.1%, while ASA class 4 with an 18.3% risk, in one study. This scoring system suffers from a lack of positive predictive value, only 57% in one study. [45]
Physiologic and Operative Severity Score for Enumeration of Mortality and Morbidity (POSSUM)
This score incorporates 12 patient-specific variables and can stratify risk among patients undergoing a particular type of operation. It has been used to assess outcomes among patients undergoing general surgery, ruptured abdominal aorta repair, vascular surgery, and lung resection for lung cancer. Additional procedure-related variables are needed to enable comparison between low- and high-risk operations. [46, 47]
Preoperative Evaluation: Thoracic Surgery
Preoperative evaluation - lung resection
Surgical resection remains the only potential curative therapy for patients with localized non–small-cell lung cancer. These patients often have COPD from a long history of smoking. Development of COPD is considered a risk factor for bronchogenic carcinoma. The first successful pneumonectomy for the treatment of lung cancer was performed by Graham and Singer in 1933. Complete resection of stage I and II non–small-cell lung cancer is associated with a 5-year survival of rate approximately 70%. The overall 5-year survival rate from lung cancer is dismal, at 14%. Hence, every patient with limited lung cancer should be rigorously evaluated for potential resectability and cure.
Preoperative assessment helps identify patients at greatest risk for postoperative complications and those patients with severe impairment, in whom surgery is prohibitive.
A multicenter study found an in-hospital patient mortality rate of 3.8% after wedge resection, 3.7% after segmental resection, 4.2% after lobectomy, and 11.6% after pneumonectomy. [48] The significant predictors of mortality were age older than 60 years, extended resection, chronic heart or lung disease, and low FEV1.
Guidelines from the American College of Chest Physicians (ACCP), [49] British Thoracic Society, and Society of Cardiothoracic Surgeons of Great Britain and Ireland [50] suggest a sequential evaluation of patients before lung resection, including spirometry and diffusing capacity measurement, estimation of predicted postoperative lung function, and exercise testing (see the flowchart below).
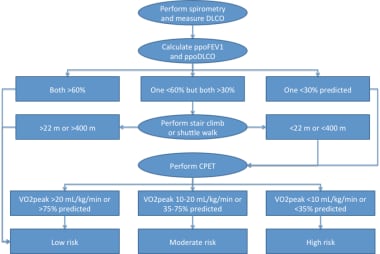 An algorithm for assessing candidates for lung resection. DLCO = diffusing capacity of the lung for carbon monoxide; FEV1 = forced expiratory volume in 1 second; MVO2 = myocardial oxygen consumption; PPOFEV1 = predicted postoperative FEV1.
An algorithm for assessing candidates for lung resection. DLCO = diffusing capacity of the lung for carbon monoxide; FEV1 = forced expiratory volume in 1 second; MVO2 = myocardial oxygen consumption; PPOFEV1 = predicted postoperative FEV1.
Step 1: Preoperative lung function
The ACCP recently revised its guidelines for pulmonary evaluation before major resection (removal of at least one lobe) for lung cancer. [49] Spirometry and diffusing capacity measurement are recommended for all patients being considered for such surgery. Cardiac risk stratification has now been added to these guidelines, but will not be discussed in the context of this review.
Step 2: Predicted postoperative lung function
Following pulmonary function testing, predicted postoperative values for FEV1 and diffusing capacity measurement should be estimated, as follows:
Predicted postoperative function = (preoperative function) × (% of function contributed by the lung that will remain postoperatively)
The percentage of function remaining can be estimated anatomically, by dividing the number of segments that will remain by the total number of segments (19).
This anatomic method performs well for predicting lung function that remains after segmentectomy and lobectomy. Quantitative radionuclide perfusion scanning is an alternative method and is particularly recommended for predicting lung function following pneumonectomy. This study provides a relative perfusion for each area of the lung (expressed as a percentage), so the percentage of function remaining can be determined by subtracting the percentage of the area(s) that will be resected from 100%. Quantitative computed tomography (CT) scanning is a newer approach that can be used similarly.
In the past, a predicted postpneumonectomy FEV1 of greater than 0.8 L was suggested as the lower limit of operability. This threshold was selected based on 2 studies. Segall and Butterworth showed that hypercapnia (PaCO2 >45 mm Hg) developed in patients with an FEV1 of less than 0.8 L. [51] Olsen et al reported that a postpneumonectomy FEV1 of less than 0.8 L was associated with prohibitive risk. [52] Other studies have since demonstrated acceptable mortality following pneumonectomy in patients with a postoperative FEV1 lower than this threshold. Additionally, the use of an absolute cutoff biases against women and shorter or older patients. Therefore, the percentage of predicted postoperative FEV1 and DLCO (%ppoFEV1 and %ppoDLCO) are preferred.
Step 3: Additional testing and risk stratification
If both predicted postoperative values are greater than 60%, the patient is stratified as low risk, generally equating to less than 1% operative mortality. If one value is less than 30%, cardiopulmonary exercise testing is recommended for further risk stratification. If one value is less than 60%, but both are greater than 30%, stair climbing or shuttle walk testing is recommended. Good performance on either of these tests places the patient in the low-risk category.
Poor performance should mandate cardiopulmonary exercise testing. Those patients who achieve greater than 20 mL/kg/min or 75% predicted on cardiopulmonary exercise testing are low risk. Those who reach less than 10 mL/kg/min or 35% predicted are high risk, which generally suggests consideration of lesser resection (wedge or segmentectomy) or a nonoperative approach (eg, stereotactic body radiation therapy, radiofrequency ablation).
Intermediate cardiopulmonary exercise testing results place the patient in a moderate risk group, for which additional testing (perfusion study to more accurately quantify postoperative lung function) and/or consideration of patient and procedure risk factors overall should be factored into further decision-making.
Preoperative evaluation - cardiac surgery
The incidence of left lower lobe atelectasis has been reported in up to 90% of patients, which may increase the postoperative morbidity and prolong the hospital stay. The incidence is attributed to phrenic nerve injury and may last from 30 days to 2 years. Operative factors associated with this complication are a longer bypass time, entrance into the pleural cavity, direct injury during mobilization of the internal mammary artery, and cold cardioplegia.
 Chest radiograph showing collapse of the left lower lobe toward the posterior and inferior aspect of the thoracic cavity. The atelectatic left lower lobe is present as a sail sign behind the cardiac shadow.
Chest radiograph showing collapse of the left lower lobe toward the posterior and inferior aspect of the thoracic cavity. The atelectatic left lower lobe is present as a sail sign behind the cardiac shadow.
The overall incidence of pulmonary complications after coronary bypass surgery is 7.5%. Patients with abnormal results from PFT’s are more likely to have prolonged mechanical ventilation and postoperative pneumonia. No studies indicate a value of pulmonary function below which cardiac surgery is precluded.
Fuster et al evaluated the effect of chronic lung diseases by correlating preoperative pulmonary function tests to postcardiac surgery outcome. [16] Of 1412 patients with preoperative PFT’s, an abnormal result was found in 39% of patients: obstructive in 26% (FEV1/FVC < 0.7), restrictive in 9%, and combined obstructive-restrictive in 4%. In addition, i-hospital mortality was higher in patients with an abnormal test (6.5%) than those without an abnormal test (0.9%). [16]
The study also demonstrated mortality was clearly related with the severity of lung disease: 0.9% in patients with an FEV1 of greater than 80%, 0.4% in patients with an FEV1 of 60-80%, 10.8% in patients with an FEV1 of 40-59%, and 54% in patients with an FEV1 of less than 40%. [16] Although COPD was not an independent predictor of mortality, an FEV1 of 60% or less was significantly associated with death (24.6% vs 1.4%).
Preparation for Surgery
Smoking cessation
Although smoking is a risk factor for postoperative pulmonary complications, one concern about smoking cessation in the immediate preoperative period is that abrupt removal of the irritant effect of cigarette smoke can inhibit coughing and lead to retention of secretions and small airway obstruction. As the beneficial effects of smoking cessation, including improvement in ciliary and small airway function and a decrease in sputum production, occur gradually over several weeks, a longer duration of abstinence before surgery would be expected to result in improved postoperative outcomes.
Warner et al prospectively investigated the role of preoperative smoking cessation on postoperative pulmonary complications in patients undergoing CABG surgery. [53] Those who currently smoked developed postoperative complications at a rate of 33%, compared with 57% for individuals who quit for less than 8 weeks. The complication rates were 11.9% in persons who never smoked and 14.5% in patients who had quit for more than 8 weeks. [53]
Although these results support the hypotheses presented above, a systematic review by Theadom and Cropley has suggested that smoking cessation should be pursued in most patients in the preoperative period, even very close to the time of surgery. [54] The study by Warner et al was the only 1 of 12 studies included in the review to suggest an increase in postoperative complications in patients who quit smoking within 2 months of surgery, although the majority of the other studies focused on low-risk operations.
Although Theadom and Cropley's review confirmed that a longer duration of smoking cessation provides a greater risk reduction, patients should be counseled to abstain from smoking regardless of the time remaining before surgery. When feasible, counseling, nicotine replacement therapies, bupropion, and varenicline improve the quit rate and should be used aggressively.
COPD
Aggressively treat patients with COPD to achieve the best possible baseline function. Bronchodilators, smoking cessation, antibiotics, and chest physical therapy may help significantly reduce pulmonary complications. Treat patients who have a persistent wheeze, functional limitation, or severe air flow obstruction with perioperative steroids.
A study of patients with COPD undergoing CABG demonstrated a decreased risk of postoperative complications among the group receiving prednisolone 20 mg daily for 10 days before surgery and continued until hospital discharge. [55] The mean pretreatment FEV1 was approximately 55% predicted. A similar study failed to show a difference in pulmonary complications between patients with COPD who did and did not receive preoperative steroids, but treated patients had a shorter intensive care unit (ICU) length of stay. [56]
Asthma
Optimize asthma control before surgery. Perioperative systemic corticosteroids are recommended for persistent symptoms if the peak flow rate and FEV1 are less than 80% predicted or previous best. Such treatment has been shown to decrease the risk of bronchospasm. [57] The safety of perioperative corticosteroids is well established in patients with asthma, and their use is not associated with death, serious infections, or adrenal suppression. Hypothalamic-pituitary-adrenal axis suppression should be assumed to be present in patients who have received systemic steroids for more than 3 weeks in the past 6 months. These patients should receive stress-dose coverage perioperatively (hydrocortisone 100 mg IV q8h, with rapid tapering after 24 h).
Preoperative antibiotics
Indiscriminate use of prophylactic antibiotics does not lead to a reduction in pulmonary complications. These drugs may be used in patients with a clinically apparent respiratory infection. Cancel elective surgery if the patient has an active infection.
Inspiratory muscle training
Studies in patients undergoing particularly high-risk operations, specifically abdominal aortic aneurysm (AAA) repair and CABG, have shown benefit for a preoperative regimen aimed at increasing inspiratory muscle strength. This intervention, consisting of exercises performed regularly for 2-4 weeks before surgery, decreased the frequency of atelectasis in patients undergoing AAA repair. [58]
An earlier study with similar intervention decreased complications and length of stay for patients at high risk of pulmonary complications following CABG. [1] Although further studies, including patients undergoing other types of operations, should be performed to validate and generalize these findings, inspiratory muscle training for at least 2 weeks before surgery may be considered for high-risk patients.
Pulmonary rehabilitation
One small study demonstrated that a 4-week inpatient pulmonary rehabilitation program improved exercise tolerance and enabled 8 patients who had previously not met criteria for lung resection for lung cancer to undergo surgery. [59] Sekine et al noted decreased hospital length of stay in patients with COPD who had undergone preoperative pulmonary rehabilitation compared to a group of patients (with a higher average baseline FEV1) who had not. [60] Bobbio et al found that brief, intense preoperative pulmonary rehabilitation can improve exercise tolerance (VO2 max) significantly among patients with COPD undergoing resection for lung cancer. [61]
Patient education
Lung expansion, deep breathing and coughing, and incentive spirometry are best taught to the patient before surgery and are useful for postoperative reduction of atelectasis.
 Incentive spirometry, along with deep breathing and coughing, is very helpful for reducing postoperative atelectasis.
Incentive spirometry, along with deep breathing and coughing, is very helpful for reducing postoperative atelectasis.
Summary
The following preoperative measures help minimize pulmonary complications in at-risk patients:
-
Smoking cessation
-
Antibiotics for acute bronchitis
-
Optimize COPD and asthma treatment regimens - Course of systemic steroids if suboptimal control
-
Educate patients on lung expansion maneuvers
-
Consider inspiratory muscle training or pulmonary rehabilitation in high-risk patients
Intraoperative Strategies
Type of anesthesia
The type of anesthesia and neuromuscular blockade affect the incidence of postoperative pulmonary complications. Intermediate- and shorter-acting agents (eg, vecuronium, rocuronium) are preferred, because residual neuromuscular blockade from longer-acting agents may contribute to pulmonary complications.
Spinal or epidural anesthesia in combination with general anesthesia is associated with less postoperative respiratory depression, but no difference in the incidence of postoperative pneumonia, compared with general anesthesia alone. Adjunctive neuraxial anesthesia should therefore be considered for high-risk patients. Depending on the type and duration of surgery, endotracheal intubation and mechanical ventilation may be preferable because of the ability to monitor and control the respiratory rate and tidal volume.
Type of neuromuscular blockade
Pancuronium, a long-acting neuromuscular blocker, may lead to residual effects, cause hypoventilation, and increase complications. Use the intermediate-acting agents (eg, vecuronium, atracurium) in high-risk pulmonary patients.
Duration and type of surgery
When available, a less ambitious, shorter procedure should be considered in extremely high-risk patients. The duration of the surgical procedure is known to affect the rate of postoperative complications. Because upper abdominal and thoracic operations carry the greatest risk, a percutaneous (laparoscopic) procedure should be substituted for an open procedure if possible.
Ventilatory strategy
In patients with COPD undergoing lung resection via thoracotomy, the use of high-frequency percussive ventilation (HFPV) for the non-dependent lung (the lung on which the surgeon was operating) resulted in improved sputum clearance following surgery and a shorter duration of hospitalization compared to intraoperative CPAP. [62] Low tidal volume ventilation decreases the risk of postoperative complications (in particular, respiratory failure) and length of stay among moderate- to high-risk patients undergoing major abdominal surgery. [63]
Fluid management
A more positive fluid balance (>5 mL/kg/h) intraoperatively was associated with an increased risk of acute exacerbation in patients with idiopathic pulmonary fibrosis who underwent resection for lung cancer. [64]
Postoperative Strategies
Lung expansion maneuvers
Lung expansion maneuvers include incentive spirometry, deep breathing exercises, postural drainage, percussion and vibration, cough, suctioning, mobilization, intermittent positive pressure breathing (IPPB), and CPAP. A meta-analysis of 48 trials suggested that the routine use of incentive spirometry provides no benefit following abdominal and cardiac surgery. [65] No conclusions could be reached concerning the use of incentive spirometry following thoracic surgery, as none of the studies addressing that question met the quality criteria for inclusion in this review.
A recent preintervention/postintervention trial attributed a significant reduction in postoperative complications following thoracotomy to the introduction of a perioperative chest physiotherapy program (consisting of bicycle or treadmill exercise, cough and deep breathing maneuvers, and upper extremity exercise), although this result may not be generalizable as the nursing ratio was 1:12 at the study institution during the course of the trial. [66] High-frequency chest wall oscillation (with use of a percussive vest every 8 h) resulted in a more rapid improvement in pulmonary function and better oxygenation than chest physiotherapy (performed every 6 h) in patients who had undergone pulmonary resection for lung cancer. [67]
In most of the studies that were included in the large meta-analysis, incentive spirometry was compared to some other lung expansion modality rather than to no therapy. [65] Among those studies with a control group, some demonstrated a reduction in complications with incentive spirometry, and others did not. These conflicting results may be due to disparities in patient populations, as incentive spirometry and other lung expansion maneuvers appear to be effective in higher risk patients.
Comparisons between modalities suggest that most are equally effective in reducing the risk of complications in such patients. For example, early mobilization was equivalent to early mobilization plus either incentive spirometry or deep breathing following cardiac surgery. [68] Incentive spirometry, deep breathing, and IPPB were equivalent, and superior to no treatment, following abdominal surgery. [29]
Studies suggest that CPAP is the most effective lung expansion maneuver. A notable benefit of this modality is that it does not require patient cooperation or effort. Disadvantages include higher cost and greater risk of adverse events. CPAP administered for 12-24 hours following thoracoabdominal aortic aneurysm repair reduced pulmonary complications, compared with intermittent CPAP use. [69] Manual chest physical therapy and early ambulation were employed in all patients. [69] Prophylactic use of continuous positive airway pressure (CPAP) or noninvasive positive-pressure ventilation (NIPPV) has been shown to decrease postoperative complications in patients following cardiac surgery, lung resection, and esophagectomy. [70, 71, 72]
In conclusion, lung expansion maneuvers, aside from early mobilization, may not be required in most patients. Other methods are likely equivalent in moderate- and high-risk patients, so selection should focus on cost, availability, and expertise. CPAP may be targeted to high-risk patients, particularly those who are not able to cooperate with other modalities. Preoperative initiation and/or patient education improve the efficacy of these maneuvers.
Pain control
Pain is a highly complex process involving specialized nociceptor fibers in the peripheral tissues; neurotransmitters and neuromodulators at all levels of neuraxis; integration of information in central nervous system; and learned behavior, affect, and cognitive status. Adequate postoperative pain control helps minimize pulmonary complications by encouraging earlier ambulation and performance of lung expansion maneuvers.
Management of postoperative pain includes administration of opioid and/or anesthetic agents into the intrathecal, epidural, or paravertebral space, or in proximity to intercostal nerves. Intrathecal administration of narcotics is associated with a longer duration of analgesia (15-22 h), respiratory depression, and headaches. Paravertebral blocks may be associated with fewer pulmonary complications than epidural analgesia. [73] Intercostal nerve blocks have been shown to be beneficial in upper abdominal, as well as thoracic, surgery.
Some studies have popularized the use of epidural analgesia as an alternative to parenteral narcotics. In upper abdominal procedures, patients who received epidural analgesia had lower rates of pulmonary complications and a shorter duration of hospital stay. Epidural catheters can be used for patients undergoing thoracic or upper abdominal surgery by placing the catheter at the thoracic vertebral level. Epidural narcotics provide a longer duration of action, a lack of excessive sedation and respiratory depression, and a minimum of or no sensory motor loss. The addition of a local anesthetic provides a more rapid onset of action and may help localize correct catheter placement; however, hypotension and motor blockade are potential adverse effects.
Epidural narcotics are morphine, fentanyl, sufentanil, and hydroxymorphine; the local anesthetics used for epidural analgesia are bupivacaine and ropivacaine. Adding small doses of local anesthetics to narcotics is a preferred approach. This potentiates pain relief, minimizes nerve blockade, and reduces adverse effects from both agents. Postoperative epidural analgesia and intercostal nerve blocks improve pain control and help reduce postoperative complications, with little risk.
Cuschieri et al reported a postoperative pulmonary complication rate of 24% in postoperative patients receiving epidural analgesia, compared with a rate of 64% in those randomized to receive intramuscular morphine. [74] Results from other studies provide conflicting results, with one possible conclusion being that patient-controlled analgesia and epidural analgesia are both superior to on-demand analgesia. [75] A recent meta-analysis supports this conclusion, but also indicates a decreased incidence of pneumonia and respiratory failure among patients receiving epidural analgesia following thoracic or abdominal surgery. [76]
Epidural hematoma is a rare complication, except when concomitant anticoagulation is prescribed. Epidural hematomas have been reported in patients receiving low molecular weight heparin (LMWH) who had epidural catheters. Warnings have been issued on this issue by the national advisory panels. A safe practice is to not place the epidural catheter for at least 12 hours after the last dose of LMWH.
Perioperative use of nonsteroidal anti-inflammatory drugs (NSAIDs) may complement other pain management strategies. Nonsteroidal agents are known to decrease the narcotic requirement in the postoperative period. The agent ketorolac may be administered intramuscularly as needed. Other nonsteroidal agents are given orally or rectally. Caution is advised in patients at risk for bleeding, with a history of peptic ulcer disease, and established renal dysfunction.
Fast track protocol
A fast track regimen that included early mobilization and enteral feeding and epidural (vs. intercostal) analgesia resulted in fewer postoperative pulmonary complications, specifically atelectasis and pneumonia, than standard care. [77]
Glycemic control
Glycemic control was associated with a reduced duration of mechanical ventilation in a mixed medical-surgical population, [78] but the impact of this intervention specifically on postoperative pulmonary complications is unclear. Additionally, the optimal blood glucose target range remains a matter of debate.
Nasogastric decompression
Routine use of nasogastric tubes until bowel function returns following abdominal surgery is associated with higher rates of pneumonia and atelectasis relative to selective use of nasogastric tubes in patients who develop postoperative nausea or vomiting, inability to tolerate oral intake, or symptomatic abdominal distention. [75] Selective nasogastric use was associated with a shorter time to oral intake without an increase in the risk of aspiration. [75]
Total parenteral nutrition
Although poor nutrition is a risk factor for postoperative pulmonary complications, the routine use of total parenteral nutrition demonstrates no benefit over total enteral nutrition or no hyperalimentation, except perhaps in patients with severe malnutrition (>10% weight loss over 6 mo) or prolonged (10-14 d) inadequate enteral feeding. [75]
Postanesthesia care unit monitoring
Identification of postanesthesia care unit events (bradypnea, apnea, desaturation, or pain/sedation mismatch) is a better predictor of subsequent pulmonary complications than a multivariable clinical score in patients with obstructive sleep apnea. [79]
Prevention of thromboembolism
Although not technically considered a postoperative pulmonary complication, brief mention should be made of venous thromboembolic disease (VTE). Surgery is a well-recognized risk factor for the development of deep vein thrombosis and subsequent pulmonary embolism. Much as postoperative pulmonary complications, the risk of VTE is influenced by patient- and procedure-related factors. Risk assessment and recommendations for prevention of VTE in surgical patients (stratified by orthopedic and nonorthopedic) are revised annually. [80, 81] (See Perioperative DVT Prophylaxis).
Summary
The following postoperative measures help minimize pulmonary complications in at-risk patients:
-
Early mobilization
-
Lung expansion maneuvers - Consider CPAP in high-risk patients
-
Adequate pain control - Consider epidural analgesia in at-risk patients
-
Selective use of nasogastric decompression and total parenteral nutrition
-
DVT prophylaxis
-
An algorithm for assessing candidates for lung resection. DLCO = diffusing capacity of the lung for carbon monoxide; FEV1 = forced expiratory volume in 1 second; MVO2 = myocardial oxygen consumption; PPOFEV1 = predicted postoperative FEV1.
-
Incentive spirometry, along with deep breathing and coughing, is very helpful for reducing postoperative atelectasis.
-
Chest radiograph demonstrating complete atelectasis of the left lung.
-
Chest radiograph showing collapse of the left lower lobe toward the posterior and inferior aspect of the thoracic cavity. The atelectatic left lower lobe is present as a sail sign behind the cardiac shadow.
-
Deep sulcus sign in a supine patient in the ICU. The pneumothorax is subpulmonic.
-
Image in a 49-year-old woman with pneumococcal pneumonia. The chest radiograph reveals a left lower lobe opacity with pleural effusion.
-
Posteroanterior (PA) and lateral chest radiograph in a patient with severe Chronic obstructive pulmonary disease (COPD). Hyperinflation, depressed diaphragms, increased retrosternal space, and hypovascularity of lung parenchyma is demonstrated.
-
Chronic obstructive pulmonary disease (COPD). A CT scan shows hyperlucency due to hypovascularity and bullae formation diffusely, predominantly in upper lobes.









