Background
West Nile virus (WNV) was first described in 1937 and is named for the West Nile district of Uganda, where it was discovered. [1] The virus has been detected in all 50 states, Puerto Rico, and 9 Canadian provinces. [2, 3]
The disease is caused by the West Nile virus, a positive-strand RNA flavivirus. [4] It is transmitted via the bite from the Culex mosquito and is known to infect humans, birds, horses, and other mammals. Birds act as a primary reservoir and means of viral replication, with high levels of viremia observed in infected crows, sparrows, blue jays, and other passerine birds. [5] WNV infection manifests as two clinical syndromes: West Nile fever (WN fever) and West Nile encephalitis (WNE).
WNE can be defined as disease that causes encephalitis, meningitis, or acute flaccid paralysis. [6] When the virus infects these structures of the central nervous system, it may be described as neuroinvasive disease.
West Nile fever can be defined as WNV disease that causes fever and nonspecific symptoms (eg, headache, muscle aches, rash, neck stiffness, vomiting) without any evidence of brain/meningeal involvement. [6] West Nile fever is generally less severe than WNE and produces symptoms in only about 25% of cases. [7] WNE, however, is generally a much more severe form of WNV infection, especially in elderly individuals, and carries a mortality rate of approximately 8%. [8, 9]
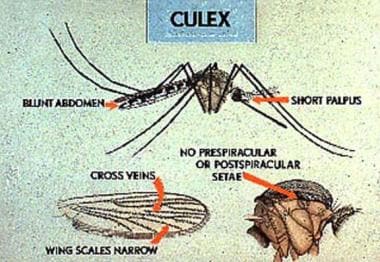 The Culex mosquito, common in the eastern United States, is the primary vector responsible for infecting humans with West Nile virus. Prevention of West Nile virus is primarily directed at reducing the mosquito population from May to October and by taking precautions to limit human exposure during these months of high mosquito activity. Image courtesy of the Centers for Disease Control and Prevention.
The Culex mosquito, common in the eastern United States, is the primary vector responsible for infecting humans with West Nile virus. Prevention of West Nile virus is primarily directed at reducing the mosquito population from May to October and by taking precautions to limit human exposure during these months of high mosquito activity. Image courtesy of the Centers for Disease Control and Prevention.
See 7 Bug Bites You Need to Know This Summer, a Critical Images slideshow, for helpful images and information on various bug bites.
For more information, see the Centers for Disease Control and Prevention (CDC) fact sheet on West Nile virus, links to state and local government web sites on West Nile virus, and the Environmental Protection Agency (EPA) article on mosquito control.
For current and up to date information on disease activity from the CDC, see https://www.cdc.gov/westnile/index.html
Prognosis
West Nile fever generally has an excellent prognosis. Most WNV infections (70%-80%) are asymptomatic and self-limited. Cases that prove to be symptomatic may produce symptoms that range from a mild febrile illness to a severe lethal encephalitis. [3] 94% of patients with encephalitis or other neuroinvasive disease were hospitalized with the highest hospitalization rates in those ≥70 years (98%). In an analysis of data from 2009-2018, CDC reported 1,154 (9%) of neuroinvasive disease cases resulting in death. The case-fatality ratio increased with increasing age; 2% of cases among patients aged < 50 years were fatal, compared with 6% of cases among those aged 50–69 years and 21% of those aged ≥70 years. [3] These findings were similar to the range of 7%-10% as reported in prior years. [8] Other age-adjusted risk factors positively correlated with death due to WNE include chronic kidney disease, hepatitis C virus infection, and immunosuppression. [10] Significant risk factors associated with development of WNE (as opposed to West Nile fever), as well as increased mortality risk, includes advanced age, malignancy, or organ transplant recipient status. [11] Other important risk factors for development of WNE include hypertension, cardiac disease, diabetes, alcohol abuse, and male sex. [10, 12]
Patients who recover from WNE may be left with considerable long-term morbidity and functional deficits. [13] About two-thirds of patients who develop paralysis during the disease course retain significant weakness in that extremity. [13] Besides muscle weakness, other, more complex, neurocognitive deficits may develop, including memory loss. [14] A small case series showed that symptoms such as fatigue, headache, and myalgias tended to persist at 8 months postinfection, with roughly 40% maintaining their gait or movement symptoms. [15] Those with WNE who developed meningitis or encephalitis had better neurological recovery at 8 months than those with acute flaccid paralysis. [15]
Epidemiology
In 2000, the CDC established ArboNet, an online epidemiologic surveillance system for the tracking of infections reported throughout the year. [16] From 1999 through the end of 2016, 46,086 cases of WNV disease were reported in the United States. Of these, 21,574 were categorized as neuroinvasive disease. There were 2,017 deaths reported over the same time period, 1,888 from neuroinvasive disease (9% case fatality rate), and 129 from non-neuroinvasive disease (< 1% case fatality rate). The 5 states with the highest number of overall cases were California (6,031), Colorado (5,362), Texas (5,277), Nebraska (3,653), and Illinois (2,368). The 5 states with the highest number of neuroinvasive cases were California (3,390), Texas (3,171), Illinois (1,481), Colorado (1,249), and Louisiana (1,009). [8]
CDC presented a data update analyzing 21,869 cases of WNV disease from 2009-2018. Of these, 12,835 (59%) were WNV neuroinvasive disease cases and were reported to CDC from all 50 states, the District of Columbia, and Puerto Rico. 89% of all WNV patients had onset of disease during July–September with later cases in more northern lattitudes. Neuroinvasive disease incidence, case-fatalities, and hospitalization rastes increased with increasing age. WNV neuroinvasive disease peaked in 2012 (0.92 cases per 100,000 population) and remained relatively stable during 2013–2018 (average annual incidence: 0.44; range: 0.40–0.51). In contrast, state level incidence varied from year to year. During 2009–2018, the highest average annual incidence of neuroinvasive disease occurred in North Dakota (3.16 cases per 100,000 population), South Dakota (3.06), Nebraska (1.95), and Mississippi (1.17), and the largest number of total cases occurred in California (2,819), Texas (2,043), Illinois (728), and Arizona (632). [3]
Among neuroinvasive WNV cases, 53% were reported as encephalitis, 37% as meningitis, 7% as AFP, and 3% as an unspecified neurologic presentation. The median age of patients with encephalitis (66 years; IQR: 54–75 years), AFP (60 years; IQR: 51–70 years), or an unspecified neurologic presentation (64 years IQR: 53–74 years) was higher than that of patients with meningitis (52 years; IQR: 38–64 years). Case-fatality ratios were higher among patients with encephalitis (14%) or AFP (13%) compared with those with an unspecified neurologic presentation (5%) or meningitis (2%). [3]
The peak month for WNV disease is August, with 83% infections occurring from July-September and 95% of infections occurring from July through the end of October. [8, 9]
The three largest outbreaks in the United States occurred in 2002 (2,946 cases), 2003 (2,866 cases), and 2012 (2,873 cases). The 2012 outbreak saw an above-average incidence of neuroinvasive disease throughout the country. [17] More than half of the WNE cases in 2012 were reported from only four states, and 29% of the overall WNE cases were reported from Texas alone. [17] That year, the incidence of WNE was 7.3 per 100,000 in Dallas County, Texas, significantly higher than the previous record rate for the county (2.91 per 100,000). [18] This outbreak was associated with an unusually warm winter and correlated strongly with the local infected-mosquito population. [18]
For current ongoing disease activity information, please see https://wwwn.cdc.gov/arbonet/maps/ADB_Diseases_Map/index.html
Patient Education
Avoidance of mosquito exposure, particularly around dawn and dusk, may help mitigate the risk of exposure to WNV. Mosquito repellents, such as DEET, as well as barrier netting, are helpful.
Pathophysiology
The WNV vector is the Culex mosquito, which typically feeds around dusk and dawn. Virus-laden saliva from the carrier mosquito infects the host. Dissemination occurs stepwise from replication in local subcutaneous tissues, and the virus spreads via lymphatics and blood vessels to solid organs and the CNS. [2]
WNV may spread to multiple host species, most commonly to horses, dogs, and other mammals. Horses can be severely affected, with a 30% mortality rate reported during a 2002 outbreak. [2] These animals, including humans, may be described as “dead end” hosts, as the levels of viremia do not facilitate high enough animal-to-mosquito transmission to perpetuate the replication cycle. [6]
More than 150 bird species have been reported as WNV-positive in CDC surveillance programs. [5] However, passerine birds (eg, species of jay, sparrow, crow, songbirds) have been shown the most competent in acting as disease reservoirs, demonstrating high levels of viremia for up to 1 week. [5] Bird-to-bird oral transmission has been demonstrated among birds kept in close contact, but bird-to-human transmission has not been reported. [4] However, standard precautions are still recommended when handling dead birds.
In addition to mosquito-borne transmission, the virus may be transmitted via solid organ transplant, trans-placental, and via blood transfusion. [19, 20, 21] Transfusion-related transmission was first described in 2002, and enhanced nucleic acid–based testing was instituted in 2003 and is now a part of routine screening to prevent transmission. [19] Laboratory-technician transmission has also been documented. [22]
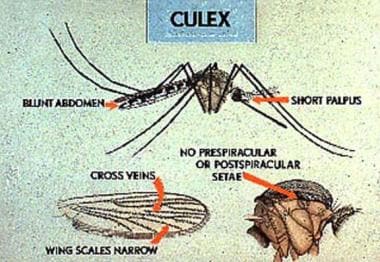 The Culex mosquito, common in the eastern United States, is the primary vector responsible for infecting humans with West Nile virus. Prevention of West Nile virus is primarily directed at reducing the mosquito population from May to October and by taking precautions to limit human exposure during these months of high mosquito activity. Image courtesy of the Centers for Disease Control and Prevention.
The Culex mosquito, common in the eastern United States, is the primary vector responsible for infecting humans with West Nile virus. Prevention of West Nile virus is primarily directed at reducing the mosquito population from May to October and by taking precautions to limit human exposure during these months of high mosquito activity. Image courtesy of the Centers for Disease Control and Prevention.
-
Common encephalitis associations.
-
Clinical features of arboviral encephalitis.
-
Differential diagnoses of meningoencephalitis.
-
The Culex mosquito, common in the eastern United States, is the primary vector responsible for infecting humans with West Nile virus. Prevention of West Nile virus is primarily directed at reducing the mosquito population from May to October and by taking precautions to limit human exposure during these months of high mosquito activity. Image courtesy of the Centers for Disease Control and Prevention.
-
The geographic distribution of the Japanese encephalitis servocomplex of the family Flaviridae, 2000. Image courtesy of the Centers for Disease Control and Prevention.
-
States reporting laboratory-positive West Nile virus infection in birds, mosquitoes, animals, or humans between January 1 and August 28, 2002. Image courtesy of the Centers for Disease Control and Prevention.






