Background
Coronary artery revascularization with saphenous vein grafts (SVGs) has become a surgical standard for treatment of coronary artery disease since Favaloro first described it in 1967. Riahi and associates described the rare complication of saphenous vein graft aneurysm (SVGA) in 1975. [1]
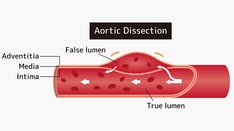
SVGA is defined as a localized dilation of the vessel to 1.5 times the expected normal diameter. These are classified as true and false aneurysms (or pseudoaneurysms): true aneurysms involve all 3 layers of the vessel wall, whereas false aneurysms involve disruption of 1 or more layers of the vessel wall with a well-defined collection of blood or hematoma outside the endothelium. True aneurysms present twice as often as pseudoaneurysms. [2] Further classification of SVGAs as large or small is not well defined, although dilation to more than 2 cm has generally led to consideration for surgical therapy. SVGAs reported in literature range from 1-14 cm in diameter.
Pathophysiology
The most common site for saphenous vein graft aneurysm (SVGA) formation appears to be the right coronary artery (38.0%), followed by the left anterior descending (25.3%), obtuse marginal (10.9%), and left circumflex (10.5%), according to a systematic review of published cases by Ramirez et al. [3] True aneurysms develop in the body of the vein graft and are typically fusiform. Early presentation of SVGA is attributed to an inherent weakness of the venous wall due to lack of circular muscle at the site of venous valves. Late presentation of SVGA is thought to be due to developing atherosclerosis and thrombus related to hyperlipidemia, hypertension, defects to the vein graft, and trauma. [4, 5, 6]
The initial event in SVGA formation is thought to be atheroma formation followed by plaque rupture, resulting in injury to the vessel wall. This cascade of events is exacerbated by arterial pressures within the vein graft. Valve insertion points along the vein graft are especially prone to true SVGA formation, where smooth muscle in the media changes from circular to a weaker longitudinal orientation. Other possible contributing factors include varicosities with impaired elastic tissue integrity not detected at the time of harvesting, vascular injury from previous percutaneous intervention (PCI), and trauma to the graft at the time of surgery. Underlying collagen vascular disease may play a role in the occurrence of SVGA. [7]
False aneurysms are saccular and typically located at the proximal SVG anastomosis, although they have been reported in the body and at the distal anastomosis. These are thought to occur because of tension on the anastomosis with suture rupture, or from technical issues in suture placement. Infection, particularly postoperative mediastinal sepsis involving Staphylococcus aureus, is commonly associated with false aneurysm formation because of suture line dehiscence. SVGA formation in the body of the graft has been reported to occur at the site of previous PCI and in the setting of chronic corticosteroid use.
Etiology
The mechanism responsible for the formation of saphenous vein graft aneurysm (SVGA) is poorly understood. Late formation of SVGA (>5 years after coronary artery bypass grafting [CABG]) is likely related to atherosclerotic degeneration leading to vessel wall weakening and resulting graft dilatation. Other factors contributing to SVGA formation include vessel wall ischemia after disruption of the vasa vasorum during the harvesting and grafting process. The high pressure and pulsatile flow of the arterial system may also contribute to SVGA formation.
Some combination of these entities likely explains late aneurysm development. Conversely, early SVGA formation likely occurs via different pathophysiology. Contributing factors leading to the formation of early SVGA include infection, intrinsic weakness of the venous wall utilized, and technical complications related to CABG surgery itself. [3]
Epidemiology
Incidence
Aneurysmal dilation of saphenous vein grafts (SVGs) is thought to be relatively common; however, putting a number to the incidence remains a challenge. Some literature reports estimate the number to be as high as 14% at 6 to 12 years, [8] whereas one case series suggested a much lower incidence of 0.07%. [9]
The true incidence of significant saphenous vein graft aneurysm (SVGA) is likely underestimated because the initial presentation may be rupture leading to sudden death, the aneurysm may not appear on angiography if it contains a significant thrombus and, importantly, many patients with SVGA do not have symptoms. It has been reported that one third of SVGA cases are found in asymptomatic patients. [3]
Race-, sex- and age-related demographics
Among reported cases of SVGA in which race was identified, the patients were White. Additionally, men represent 87% of the SVGA cases. [10] The sex difference may be, in part, because men have a higher rate of atherosclerotic disease and more men than women undergo coronary artery bypass surgery. [3]
SVGAs present on average within the sixth decade of life. Women tend to be older than men at presentation, probably because they generally develop coronary artery disease later in life and therefore undergo coronary artery revascularization later than men.
Nearly 70% of SVGAs occur 10 years after coronary artery bypass surgery. [3] However, time to onset has been reported over a wide range. Both true and false SVGAs have been reported within months of surgery. Baydoun et al described a SVGA presenting as abdominal pain compressing the adjacent liver 43 years after surgery. [11]
Prognosis
Morbidity/mortality
No long-term studies regarding prognosis are available, but saphenous vein graft aneurysm (SVGA) is thought to carry a poor prognosis, with survival suggested to be around 2 years. [3] Underlying coronary artery disease, hyperlipidemia, and hypertension have negative effects on patient prognosis. [5] Increasing aneurysm size is associated not only with higher risk of rupture but also with high morbidity and mortality. [3] Ischemic symptoms occur from graft occlusion, embolic phenomena, or compression of the graft by the aneurysm. As previously mentioned, many SVGAs remain subclinical, thus morbidity and mortality estimates are likely affected by selection bias. In symptomatic patients, mortality is high, with 13 of 46 patients (28%) dying within 90 days of initial symptoms. Furthermore, in-hospital mortality for giant SVGA has been reported at greater than 15%. [12]
Complications
Complications of SVGAs include the following:
-
Sudden aneurysm rupture leading to hemothorax, hemopericardium, or sudden death
-
Thrombus formation within the aneurysm is very common and may result in embolization to the bypassed vessel with ischemia or infarction.
-
Compression and mass effect on adjacent cardiac and mediastinal structures
-
Fistula formation between the aneurysm and right atrium, left atrium, right ventricle, pulmonary artery, bronchus, or chest wall
-
Superior vena cava (SVC) syndrome has been reported in association with SVGA to right atrial fistulas and with false aneurysm rupture.
-
Saphenous Vein Graft Aneurysms. Computed tomography scan demonstrating a saphenous vein graft aneurysm.
-
Saphenous Vein Graft Aneurysms. Cardiac catheterization demonstrating a saphenous vein graft aneurysm.
-
Saphenous Vein Graft Aneurysms. Aortogram demonstrating a saphenous vein graft aneurysm.
-
Saphenous Vein Graft Aneurysms. This computed tomography scan reveals a saphenous vein graft aneurysm.
-
Saphenous Vein Graft Aneurysms. Angiogram of a saphenous vein graft to the distal right coronary artery demonstrating a large aneurysm in the mid portion of the graft. Video courtesy of John S. Douglas, MD.
-
Saphenous Vein Graft Aneurysms. Final angiogram demonstrating coils within the aneurysm, and almost complete cessation of flow from the parent vessel into the aneurysm. Video courtesy of John S. Douglas, MD.
-
Saphenous Vein Graft Aneurysms. Another view demonstrating the saphenous vein graft aneurysm. Video courtesy of John S. Douglas, MD.
-
Saphenous Vein Graft Aneurysms. The first of many coils being deployed in the aneurysm. Video courtesy of John S. Douglas, MD.