Practice Essentials
Urinary diversion is indicated when the bladder can no longer safely function as a reservoir for urine storage. This article covers the most common types of diversion, the most common indications for diversion, and the most common early and late complications following urinary diversion. See the image below.
For patient education resources, see eMedicineHealth's Bladder Cancer.
History of the Procedure
Surgeons have been performing urinary tract diversions for almost 150 years. In 1852, Simon performed the first ureteroproctostomy in a patient with exstrophy. Since then, the procedures have been refined, and patient outcomes have improved. Currently, urinary tract diversions are separated into two standard categories: continent diversions and noncontinent diversions, which necessitate external ostomy collecting devices. Further historical milestones of urinary diversion are as follows:
-
1851 - Ureteroproctostomy (Simon)
-
1878 - Ureterosigmoidostomy (direct anastomosis) (Smith)
-
1898 - Rectal bladder (Gersuny)
-
1950s - Ileal loop (Bricker)
-
1959 - Ileal neobladder (Camay)
-
1970s - Koch pouch
-
Early 1980s - Indiana pouch
-
Late 1980s - Orthotopic diversion
Problem
Noncontinent urinary diversion
Diversion into a noncontinent conduit is considered less technically demanding and is associated with the fewest postoperative complications; therefore, this technique is the criterion standard. Noncontinent urinary diversion is performed by either directly anastomosing the ureters to the anterior body wall (ie, cutaneous ureterostomy) or using a segment of bowel to anastomose in a similar manner to the anterior wall for ostomy bag drainage.
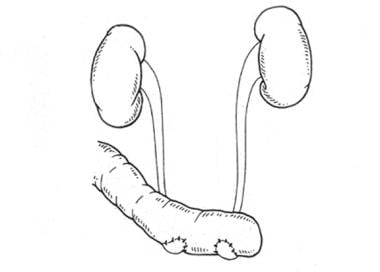
The bowels most commonly used for noncontinent conduit diversion are 15-25 cm of ileum (see the image below), colon, and, least often, jejunum bowel segments. These segments usually lend themselves to easy mobilization on a vascular pedicle, which allows for ureter anastomosis at the proximal end and stoma formation on the abdominal wall (most often in the right lower quadrant) at the distal end. In order to promote drainage and to minimize urine reflux, ensuring that the urine flows in a properistaltic manner relative to bowel segment motility is important.
Direct ureter anastomosis with the skin is the only form of diversion that does not require use of the gastrointestinal tract. In pediatric patients, cutaneous ureterostomy is often performed as a temporizing measure prior to a future and more definitive procedure. In adults, cutaneous ureterostomy is currently rarely performed.
Continent urinary diversion
The most commonly used bowel segments for continent urinary diversion are either ileum (as depicted below) or a combination of terminal ileum and ascending colon. Ensuring that all continent diversions store and empty urine at low pressures is paramount. High storage and voiding pressures ultimately cause high-pressure reflux nephropathy and may result in renal failure; therefore, all bowel segments used for continent diversion, with the exception of their use in a ureterosigmoidostomy procedure, are initially detubularized. The bowel segments are then refashioned in a more spherical shape, which increases capacity and decreases luminal pressure by a magnitude of 3- to 4-times lower than the original segmental pressure.
Orthotopic diversion (ortho meaning correct, topic meaning of a place) is a term that describes the reconstructed pouch anastomosed to the native urethra. Neobladder is a term used synonymously with orthotopic diversion. The continence mechanism in an orthotopic diversion is the native urethral rhabdosphincter. Continent diversion may be further categorized into 3 types: (1) orthotopic or neobladder diversion, (2) continent catheterizable diversion, and (3) ureterosigmoidostomy.
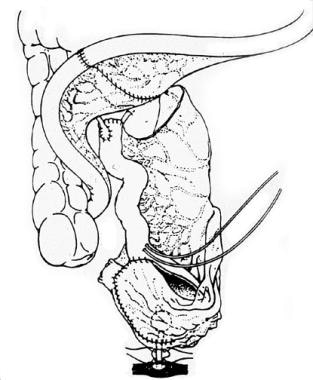
Patients with a continent catheterizable stoma have a one-way valve mechanism fashioned at the insertion site that leads into the urinary storage system. The limb allows for catheterization through a small stoma on the abdominal wall, enabling the system to empty; however, this limb remains continent during the storage phase between catheterizations. Mechanisms for continence of the efferent limb include a flap valve, nipple valve, pressure equilibration, or combinations of thereof. Ureterosigmoidostomy consists of anastomosing the ureters to the sigmoid colon in a nonrefluxing manner. This diversion method relies on the anal sphincter for continence. For reasons listed in Complications, ureterosigmoidostomy is becoming a less popular method of continent diversion. See the image shown below.
Epidemiology
Bladder cancer is the sixth most common cancer in the United States. Bladder cancer is 3 times more common in men than in women and is 1.5-2 times more common in White Americans than in Black Americans.
The American Cancer Society estimates that 81,180 new cases of bladder cancer will be diagnosed in the United States in 2022 and that 17,100 people will die of the disease. [1] The incidence of bladder cancer increases with age, with a median age at diagnosis of 73 years. Bladder cancer is rarely diagnosed in patients aged younger than 40 years. [2]
For additional information on bladder cancer, see Medscape’s Bladder Cancer Resource Center.
Etiology
The most common indications for urinary system diversion are as follows:
-
Bladder cancer requiring cystectomy
-
Neurogenic bladder conditions that threaten renal function
-
Intractable incontinence in females
Pathophysiology
The pathophysiology of the specific indications for urinary diversion listed above is well reviewed in other Medscape Reference articles and is not addressed here.
The pathophysiology of urinary diversion is best described by the interaction of stored urine with the mucosal lining of bowel segments. The inherent property of all bowel segments is that they absorb components of fluids with which they are in contact. Therefore, the urologist who treats patients with urinary diversions is presented with many unique clinical challenges. Specific details regarding the metabolic abnormalities and other problems experienced are discussed further in Complications.
Presentation
Patients who require urinary diversion are often monitored for a time by their urologist, and the decision for surgical intervention is made if conservative management fails. Patients with complications of urinary diversion may present to the primary care physician at any time. Because the complications of urinary diversion are the most common clinical presentation to the primary provider in the urgent setting, this section focuses on the clinical presentation of complications.
Most often, patients with complications of urinary diversion present with an appearance of obvious illness. In the 1950s, Ferris and Odel described the classic presentation of such patients, which consisted of easy fatigability, weakness, anorexia, weight loss, polydipsia, nausea, vomiting, and diarrhea. [3] Additionally, these patients may be bacteremic or septic due to overgrowth in their often-colonized urinary reservoirs or conduits.
The hallmark metabolic abnormality observed in a patient with a jejunal conduit is hyperkalemic, hypochloremic, hyponatremic metabolic acidosis. Patients with ileal conduits, colon conduits, or continent reservoirs tend to present with hyperchloremic metabolic acidosis with normal or low potassium levels.
Patients with urinary retention usually present with abdominal pain and distension. This condition is a medical emergency, and drainage of the reservoir is indicated. Haupt et al reported on a patient with an orthotopic bladder who produced enough mucous to result in bladder outlet obstruction and reservoir rupture. [4]
In patients who have undergone ileal resection for diversion and present with megaloblastic anemia, vitamin B-12 deficiency should be considered.
Patients with continent reservoirs are at risk for secretory and/or osmotic diarrhea, depending on the length of ileum used and whether the ileocecal valve was resected for construction of the urinary pouch. Diarrhea and the metabolic abnormalities discussed above result in a presentation that consists primarily of dehydration.
Indications
Conservative nonoperative medical therapy is the first modality of choice in the management of any spinal abnormality, whether traumatic or congenital. Surgical diversion or augmentation of the urinary tract is indicated only when other less-invasive options have failed. The primary indications for diversion include preservation of renal function, prevention of recurrent infection, and elimination of the need for permanent indwelling catheters.
Indications for diversion arise when the native bladder becomes inherently dangerous to the host. The most common indications for diversion are as follows, in descending order of frequency:
-
Bladder cancer requiring cystectomy
-
Neurogenic bladder conditions that threaten renal function
-
Severe radiation injury to the bladder
-
Intractable incontinence in females
-
Chronic pelvic pain syndromes
Indications for diversion of the upper urinary tract may be divided into malignant and benign disease. Cancer may involve the bladder as a primary lesion, or the bladder may be involved with cancer originating in contiguous pelvic organs. In either case, a radical bladder excision, at times, may provide the patient's best chance for long-term survival.
Patients who present with muscle-invasive tumors (T2 or greater tumor stage) or those who have a particularly aggressive and/or progressive T1 tumor stage are most often treated with a radical cystectomy. The cystectomy includes a radical prostatectomy in men and a hysterectomy with or without an anterior layer of vaginal tissue in women. [5, 6]
Neurogenic conditions that require urinary diversion are most often caused by either traumatic or congenital etiologies. Traumatic spinal cord injury most often affects men aged 16-35 years. Of patients who experience spinal cord trauma, 25% are incomplete quadriplegics, 25% are complete quadriplegics, 25% are incomplete paraplegics, and 25% are complete paraplegics. After spinal shock resolves, the patient's bladder often stores and empties urine in a relatively predictable pattern.
Myelodysplasia is the most common congenital spinal abnormality and the most common etiology of a neuropathic bladder in children. Myelodysplasia occurs in approximately 1 per 1000 births in the United States. In the last half century, the incidence of neural tube defects at birth has decreased, likely because of increased prenatal diagnosis and pregnancy termination. Most patients with myelodysplasia are treated with bladder augmentation; however, some patients require urinary diversion. Approximately 40% of children with myelodysplasia are at high risk for upper urinary tract changes, and approximately 6-8% of these patients require surgical intervention.
Benign disease usually involves elevated storage pressure of the native bladder, which is inherently dangerous to the upper urinary tract. Less commonly, diversion is indicated for patients with intractable incontinence or chronic pelvic pain syndromes. In men, the prostate is usually removed with the bladder, whether the indication is benign or malignant in nature. When treating benign disease in women, the decision to perform a bladder excision is based more on the surgeon's preference.
Chronic pelvic pain syndromes most commonly arise from bladder cancer. Congenital or traumatic injury to the spinal cord often leads to abnormal urinary storage and emptying. Most often, the neuropathic abnormalities are managed in a nonoperative manner. Occasionally, surgical diversion or urinary tract augmentation is required.
Other specific conditions may include abnormally high urinary storage pressures, often observed late in an areflexic bladder that never recovers function after spinal shock. This condition is also common in patients with detrusor external sphincter dyssynergy.
Relevant Anatomy
Anatomy relevant to urinary diversion is primarily associated with the bowel blood supply, specifically, branches of the superior mesenteric artery. Both continent and noncontinent urinary diversions are performed with the use of ileum as shown below, ascending colon, or both or with transverse colon and, occasionally, sigmoid colon. Each bowel segment must be mobilized on its mesenteric pedicle, respecting the major arterial supply on which it depends for survival.
Because regular variation exists in arterial branches of the ileum and large bowel, most arcades are identified intraoperatively by examination and back lighting in order to preserve the proper plexus.
Diversion with ileal segments usually begins at least 15 cm from the ileocecal valve and involves segments from 15-80 cm in length, depending on the surgeon's goals. The ileocolic arterial branch and relevant marginal arterial arcade are most often the source of the pedicle. Ileocecal, ascending, and transverse colonic segments rely on a combination of superior mesenteric branches (ileocolic and right and middle colic arteries). See the image below.
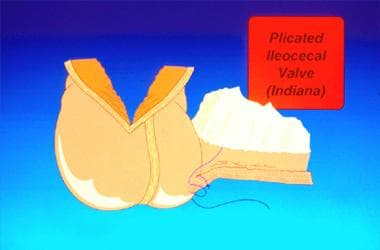 Ileocecal urinary diversion using a plicated efferent limb and catheterization; ureters are anastomosed into the bowel wall. Courtesy of Karl Kreder, MD.
Ileocecal urinary diversion using a plicated efferent limb and catheterization; ureters are anastomosed into the bowel wall. Courtesy of Karl Kreder, MD.
Gastric segments are not used commonly for urinary diversion, although they remain popular for bladder augmentation.
For more information about the relevant anatomy, see Arterial Supply Anatomy, Colon Anatomy, and Bladder Anatomy.
Contraindications
The major contraindications to urinary diversion are bowel-type specific. Because of refractory metabolic abnormalities, jejunal segments should be used only in the absence of another acceptable type of bowel segment. Bowel injured by radiation should not be used for diversion. Patients with poor renal function, severe metabolic abnormalities, and significant proteinuria should not undergo diversion with continent reservoirs. Additionally, patients who lack motivation or are unable to catheterize a continent reservoir should not undergo diversion in this manner.
Because of the potential complications of a continent reservoir versus a noncontinent diversion, the urologist must be aware of the following specific contraindications prior to performing continent diversion:
-
Elderly age and spinal cord injuries associated with poor hand coordination are absolute contraindications for continent urinary diversion (including neobladder) because of the need for intermittent catheterization and the potential for catastrophic complications should these individuals fail to do so.
-
Bowel abnormalities such as Crohn disease, severe irritable bowel syndrome, fat malabsorption, and, potentially, ulcerative colitis preclude the surgeon from taking long segments of bowel.
-
Patients with a preoperative creatinine clearance of less than 60 mL/min should not undergo continent urinary diversion.
-
Those with a prior history of high-dose radiotherapy to the abdomen and/or pelvis should not have long lengths of small bowel used.
-
Noncontinent urinary diversion with ileum. Courtesy of Karl Kreder, MD.
-
Ileocecal urinary diversion using a plicated efferent limb and catheterization; ureters are anastomosed into the bowel wall. Courtesy of Karl Kreder, MD.
-
Schematic diagram of continent urinary diversion with ileum. Courtesy of Karl Kreder, MD.
-
Continent urinary diversion using ileum.
-
Close-up photograph of continent urinary diversion using ileum.