Practice Essentials
Ureteroscopy is defined as upper urinary tract endoscopy performed most commonly with an endoscope passed through the urethra, bladder, and then directly into the upper urinary tract. Indications for ureteroscopy have broadened from diagnostic endoscopy to various minimally invasive therapies. Technological advancements have led to broader indications while minimizing peri-operative complications resulting in efficacious access to the upper tract.
See image below.
Endoscopic lithotripsy, treatment of upper urinary tract urothelial malignancies, stricture incisions, and ureteropelvic junction obstruction repair are all current treatments facilitated by contemporary ureteroscopic techniques. Because the application of ureteroscopic procedures has evolved from a diagnostic tool to a facilitator in complex therapeutic interventions, a proportional increase in the rate and severity of complications would be expected. However, with improved instrumentation and evolution of surgical technique, the complication rate associated with ureteropyeloscopy has actually decreased significantly.
History of the Procedure
The progression from cystoscopy to upper urinary tract endoscopy was natural, with pediatric cystoscopes being used as the first rigid rod-lens ureteroscopes. Relatively large rod-lens endoscopes, averaging 12F (3F = 1 mm) in diameter, combined with ultrasonic and electrohydraulic lithotripsy probes became the first commonly accepted ureteroscopic equipment combination used to treat distal ureteral calculi.
Ureteroscopic treatment of calculi and, in particular, distal ureteral stones was the first common application of upper urinary tract endoscopy. Early in this evolution, smaller and more precise instrumentation was obviously found to cause less trauma to normal tissues. Rigid ureteroscopes progressed from rod-lens imaging to fiberoptic imaging with outer-diameter miniaturization. The narrow and delicate distal ureter once required vigorous balloon dilation for ureteroscopic access; however, by 1989, the fiberoptic-based rigid endoscopes were small enough (averaging 7F in diameter) for frequent placement in the distal ureter under direct vision. The small rigid ureteroscopes combined with both laser and pneumatic lithotriptors are currently used to treat distal ureteral calculi in both university and community settings.
Flexible ureteroscopy was an attractive alternative to rigid ureteroscopy in that the more proximal ureter and intrarenal collecting system were theoretically more easily accessible with this type of instrument. The application of flexible ureteroscopy was first reported by Marshall in 1964. [1] He described the passage of a 9F endoscope manufactured by American Cystoscope Makers (Pelham Manor, NY) into the ureter to visualize an impacted ureteral calculus. These first flexible ureteroscopes were not capable of being directed and did not have a working channel, thus permitting only the most primitive diagnostic maneuvers. The subsequent addition of a cystoscopically placed “guide tube” facilitated placement of the first flexible ureteroscopes. In addition, irrigant then could be passed through the guide tube to displace the ureteral mucosa and debris from the distal endoscopic lens.
In the early 1980s, Bagley, Huffman, and Lyon began work at the University of Chicago to develop an improved flexible fiberoptic ureteropyeloscope. [2] Three major design changes improved the potential of the flexible ureteroscope. First, the addition of a working channel allowed irrigant and endoscopic accessories to be passed directly through the endoscope rather than through an operating sheath. Second, active tip deflection allowed the endoscope to be directed or steered to areas of interest. Finally, by altering the stiffness (ie, based on durometer measurements) of the endoscope shaft, the actively deflecting portion could be combined with passive buckling of the endoscope (ie, secondary deflection), which facilitated lower-pole intrarenal access as depicted below.
The first steerable, actively deflectable, flexible ureteropyeloscopes were equipped with relatively large fiberoptic bundles for imaging and illumination. The addition of the working channel and a cable-and-pulley system used for active tip deflection required on outer diameter of 3.6 mm. By the late 1980s, optical fiber miniaturization and improved geometrical pixel packing produced a smaller fiberoptic bundle and thus, a smaller-diameter endoscope. Flexible ureteroscope specifications in 1990 included a 10F outer diameter, a standard 3.6F working channel, and unidirectional active tip deflection. Guide tubes were no longer required as direct guidewire endoscope placement became mainstream. Intramural ureteral dilation was often required for placement of this flexible ureteroscope into the upper urinary tract. These endoscopes allowed inspection of the entire intrarenal collecting system and became part of the standard evaluation of filling defects within the upper urinary tract defined on contrast-enhanced imaging studies and pyelograms.
The introduction of small diameter (< 8F) flexible ureteroscopes in 2001 offered greater active tip deflection and significantly advanced the therapeutic and diagnostic efficacy of ureteroscopy. These endoscopes maintained a standard 3.6F working channel for irrigation and accessory use while offering a greater deflection radius. In addition, the stiff shaft allowed for atraumatic direct endoscope placement often without a guidewire.
In 2014, digital imaging replaced fiberoptics for the small diameter flexible ureteroscope. This addition provides greater clarity with digital enhancement that improves the sensitivity of tumor mapping. The digital imager removes the round “insect eye” appearance of the quartz bundles providing a bright clear rectangular image that has 20 times the resolution of the fiberoptic and can be enhanced to accentuate malignant lesions and other urothelial anomalies. The tiny CMOS chip imager has been incorporated with the now standard specifications of small shaft diameter, exaggerated tip deflection, standard 3.6F working channel, etc. [3] Integrated digital ureteroscopes are lighter, with integrated L.E.D.s at the end of the device. Without the need for an attached camera head and light cord, there are fewer potential points for device failure, and are also ergonomically superior to its predecessor. [4]
Currently, rigid and flexible ureteroscopes average 8F in tip diameter and are commonly passed atraumatically into the upper urinary tract without intramural dilation. These endoscopes are used to diagnose and treat various upper urinary tract disorders including calculi, urothelial malignancies, stricture disease, and bleeding lesions. The addition of laser energy applied through optical quartz fibers passed through the working channel of the endoscope has facilitated these treatments. Specific treatments are discussed further in subsequent sections of this article.
Problem
Ureteroscopy is used as a diagnostic tool in situations such as investigating abnormal imaging findings, assessing obstruction or unilateral essential hematuria, or localizing the source of positive urinary cytology results.
Therapeutic uses of ureteroscopy have broadened to include various minimally invasive therapies. Endoscopic lithotripsy (treating stones), treatment of upper urinary tract urothelial malignancies, stricture incisions, and ureteropelvic junction obstruction repair are all current treatments facilitated by contemporary ureteroscopic techniques.
Epidemiology
Ureteroscopy is a routine procedure performed by urologists. The most common indication is to treat upper urinary tract calculi, particularly those that are either unsuitable for extracorporeal shockwave lithotripsy or are refractory to that form of treatment. Other common indications include evaluation of an abnormal lesion revealed by less invasive imaging tools (eg, intravenous pyelography [IVP], MRI, CT scanning) or localization of the source of positive urine culture or cytology results. Thus, ureteroscopy is often an essential part of the diagnostic algorithm and can also be used to treat the underlying disorder.
Indications
Diagnostic indications for ureteropyeloscopy are as follows:
-
Abnormal imaging findings - Filling defect
-
Obstruction - Determination of etiology
-
Unilateral essential hematuria
-
Localizing source of positive urinary cytology results, culture results, or other test results
-
Evaluation of ureteral injury
-
Surveillance with known history of urothelial malignancy
Therapeutic indications for ureteropyeloscopy are as follows:
-
Endoscopic lithotripsy
-
Retrograde endopyelotomy
-
Incision of ureteral strictures
-
Improvement of calyceal drainage
-
Treatment of calyceal diverticular lesions
-
Treatment of malignant urothelial tumors
-
Treatment of benign tumors and bleeding lesions
Relevant Anatomy
The ureter has 3 physiologic narrowings: (1) the ureteropelvic junction, (2) the crossing over the iliac vessels, and (3) the ureterovesical junction. This is crucial in the manifestations of calculus disease. These narrowings may result in ureteral stones becoming trapped and obstructing at these specific levels. For more information about the relevant anatomy, see Ureter Anatomy.
The segments of the ureter in which calculi can become lodged are also natural barriers for the ureteroscope. The intramural ureter is the narrowest segment and can prohibit endoscope passage. Guidewires are frequently passed into the ureteral orifice cystoscopically and are then directed into the renal pelvis with fluoroscopic assistance. Guidewires straighten the ureter and can facilitate (1) dilation of obstructed segments with balloon or graduated dilators, (2) advancement of endoscopes over the wires into the proximal collecting system, and (3) placement of internal stents and drainage catheters.
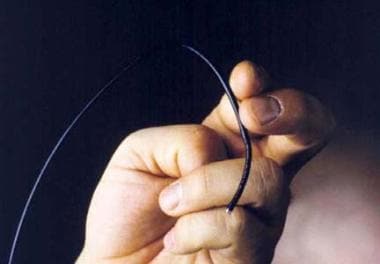
The intramural ureter once required balloon dilation for endoscope access. Small diameter semirigid ureteroscopes commonly employed in the lower ureter have graduated shafts with an oval or triangular 7.5F tip (see image below). This facilitates direct tip access, and when advanced the intramural segment is also modestly dilated (ie, dilation under direct vision). Use of a working sheath to facilitate passage of the ureteroscope beyond the intramural ureter can be employed when repeated access to the ureter is expected or if the intramural ureter is unusually tight or restrictive. The use of operative sheaths is optional, and is generally not required. Furthermore, recent literature has suggested that the use of such sheaths may have detrimental effects, [5] including recent studies demonstrating cellular damage in animal models. [6]
 Comparison of the semi-rigid Karl Storz ureteroscope and tip (above) with that of the ACMI MR6 endoscope (below).
Comparison of the semi-rigid Karl Storz ureteroscope and tip (above) with that of the ACMI MR6 endoscope (below).
Operative ureteral access sheaths have, in general, a relatively large outer diameter ranging from 12F to 16F, often significantly greater than the normal diameter of the ureteral lumen with the obvious risk of wall trauma during insertion. Traxer and colleagues in Paris recently underscored this concern by evaluating ureters immediately after sheath removal. [5] Ureteral trauma with wall damage was found in almost one-half of patients (46.5%), with high grade full thickness injury identified in 13.3%. Similar findings were confirmed by Guzelburc et al with low-grade injuries found in 41.5% of patients, [7] and a meta-analysis by Huang et al demonstrated a higher incidence of post-operative complications with the use of ureteral access sheaths (OR 1.46), including persistent post-operative hematuria, increased need for post-operative ureteral stents and ureteral strictures. [8] These high rates of trauma are exponentially greater than noted in series where small diameter endoscopes were placed directly into the ureter, thus questioning the long term risk of subsequent stricture disease associated with routine operative sheath use. For these reasons access sheaths should be employed judiciously.
As the fiberoptic-based rigid ureteroscope continues proximally past the ureteral orifice, it then is inhibited by the natural curvature of the ureter as it crosses the iliac vessels, psoas muscle, and the ureteropelvic junction. If the ureter is dilated, the rigid endoscope may be safely passed proximally. If not, then conversion to an actively deflectable flexible endoscope is indicated.
Flexible ureteroscopes are passed into the upper urinary tract with a wireless technique or over a guidewire. The flexible ureteroscope is a particularly useful instrument, especially when a rigid endoscope cannot be placed safely into the more proximal ureter or if intrarenal inspection is required. In these cases, endoscope tip deflection is essential to completely inspect the calyces.
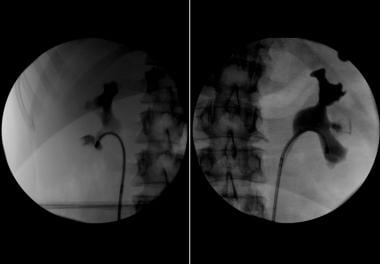
Lower pole intrarenal access performed with a flexible ureteroscope can be challenging and may require both active tip and passive shaft deflection. Design improvements of the small diameter flexible ureteroscopes include two-way logical or “intuitive” active endoscope tip deflection (ie, thumb lever down causes tip to go down and vice versa), a large radius of deflection, and incorporation of a standard passive secondary deflecting segment of the more proximal shaft (which buckles to produce greater deflectability for the most dependent lower pole intrarenal access).
To place the tip of the endoscope into the lower pole, the instrument must first be actively deflected and then advanced to allow the proximal shaft to buckle as depicted below. This maneuver, termed secondary deflection, was historically required in 60% of traditional flexible ureteroscopies for a complete inspection. The increased active deflection offered by new-generation flexible ureteroscopes significantly decreases the need for secondary deflection and enhances the surgeon’s ability to inspect all aspects of the renal collecting system.
Contraindications
Diagnostic ureteroscopy has few contraindications. Untreated urinary tract infection, endoscopy without appropriate antibiotic coverage, and uncorrected bleeding diathesis are relative contraindications.
Contraindications to therapeutic ureteroscopy (eg, lithotripsy, endopyelotomy, tumor therapy) are more numerous and can mirror those associated with the corresponding more invasive open surgical intervention. In general, the major contraindications are related to untreated infections and uncorrected bleeding diathesis prior to therapeutic endoscopy.
-
Flexible fiberoptic ureteropyeloscope.
-
Secondary endoscope deflection that allows lower-pole intrarenal access.
-
Plain radiograph that defines a large renal pelvic calculus with the flexible ureteroscope passed beyond the stone burden.
-
Ureteroscopic image of an impacted jack stone in the ureter. These calculi are composed of calcium oxalate monohydrate.
-
Ureteroscopic image of a papillary transitional cell carcinoma of the ureter.
-
A parapelvic cyst (star) causes splaying of the middle and lower pole calyces making access to a lower pole stone (arrow) very difficult.
-
Comparison of the semi-rigid Karl Storz ureteroscope and tip (above) with that of the ACMI MR6 endoscope (below).
-
Using secondary deflection, access to this lower pole stone burden is made possible.
-
The use of dilute contrast injected through the ureteroscope ensures adequate mapping and inspection of all calyces
-
Wireless ("no touch") ureteroscopy, laser lithotripsy and stone extraction technique performed with the digital ureteroscope.